Difference between revisions of "Prostate cancer staging"
Jump to navigation
Jump to search
(→Tumour) |
|||
| Line 9: | Line 9: | ||
===Tumour=== | ===Tumour=== | ||
{| class="wikitable sortable" | |||
! Stage | |||
! Criteria | |||
! Notes | |||
|- | |||
| T2 | |||
| confined to prostate | |||
| subdivision based on bilateral/unilateral involvement not predictive | |||
|- | |||
| T3a | |||
| extension into periprostatic soft tissue | |||
| | |||
|- | |||
| T3b | |||
| extension into the muscle of the seminal vesicles ''or'' bladder neck | |||
| | |||
|- | |||
| T4 | |||
| extension into a surrounding anatomical structure, e.g. [[urinary bladder]], [[uterus]] | |||
| bladder neck invasion is T3b | |||
|} | |||
====Extraprostatic extension==== | ====Extraprostatic extension==== | ||
Revision as of 04:47, 4 July 2016
The article deals with prostate cancer staging. A general discussion about staging is found in cancer staging.
An introduction to prostate cancer is found in the prostate cancer article.
General
- Important for prognosis and treatment.
TNM staging system
Tumour
| Stage | Criteria | Notes |
|---|---|---|
| T2 | confined to prostate | subdivision based on bilateral/unilateral involvement not predictive |
| T3a | extension into periprostatic soft tissue | |
| T3b | extension into the muscle of the seminal vesicles or bladder neck | |
| T4 | extension into a surrounding anatomical structure, e.g. urinary bladder, uterus | bladder neck invasion is T3b |
Extraprostatic extension
- Abbreviated EPE.
General
- Extraprostatic extension (EPE) is difficult to assess in prostatectomy specimens.[1]
- The prostate does NOT have a well defined capsule.
- Intraobserver agreement for EPE is fair-moderate and lower than for the surgical margin.[2]
- The prostate does NOT have a well defined capsule.
- EPE, typically, upstages tumours from T2x to T3a.
Prostatectomy specimens
EPE is present in a prostatectomy if there is either:
- A "significant bulge" in the contour of the prostate at low power and no fibromuscular tissue surrounding the malignant cells.
- Malignant cells directly adjacent to peri-prostatic adipose tissue.
Note:
- The apex of the prostate gland may have some skeletal muscle. Thus, it is difficult to define extension at this site. EPE is not called at the apex by some pathologists; however, it is generally believed to exist.[1]
Prostate biopsy
EPE is present in prostate biopsy if:
- Tumour touches adipose tissue.[3]
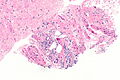
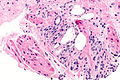
Images
Seminal vesicle invasion
- Abbreviated SVI.
General:
- Typically upstages to pT3b.
- Associations:[4]
- Most SVI is by direct extension ~90%.
- Approximately 20% of patients with pT3x have SVI.
- Usually associated with a large tumour volume (22% versus 12%).
Microscopic:
- Tumour must be in the muscle surrounding the epithelial component; tumour in the adventitia (the loose connective tissue surrounding the seminal vesicles) does not count.[5][6]
Notes:
- Invasion of the adventitia (only) would quality as EPE; this is, usually, T3a.
- Immunostains useful to separate prostate carcinoma from SV are discussed in the seminal vesicle article.
- It is not possible to differentiate the seminal vesicles and ejaculatory ducts based only on histology; thus, on biopsy one can generally comment only on seminal vesicle/ejaculatory duct invasion.
Lymph node
Note:
- Lymph node metastases essentially never happen in Gleason score 6 cancers.
- A study of over 14,000 Gleason score <=6 cases found 22 cases with lymph node metastases -- all of the 19 cases available for review were determined to have a higher Gleason score and some Gleason pattern 4 or 5.[7]
See also
References
- ↑ 1.0 1.1 Magi-Galluzzi, C.; Evans, AJ.; Delahunt, B.; Epstein, JI.; Griffiths, DF.; van der Kwast, TH.; Montironi, R.; Wheeler, TM. et al. (Jan 2011). "International Society of Urological Pathology (ISUP) Consensus Conference on Handling and Staging of Radical Prostatectomy Specimens. Working group 3: extraprostatic extension, lymphovascular invasion and locally advanced disease.". Mod Pathol 24 (1): 26-38. doi:10.1038/modpathol.2010.158. PMID 20802467.
- ↑ Evans, AJ.; Henry, PC.; Van der Kwast, TH.; Tkachuk, DC.; Watson, K.; Lockwood, GA.; Fleshner, NE.; Cheung, C. et al. (Oct 2008). "Interobserver variability between expert urologic pathologists for extraprostatic extension and surgical margin status in radical prostatectomy specimens.". Am J Surg Pathol 32 (10): 1503-12. doi:10.1097/PAS.0b013e31817fb3a0. PMID 18708939.
- ↑ Epstein, JI.; Srigley, J.; Grignon, D.; Humphrey, P. (Sep 2007). "Recommendations for the reporting of prostate carcinoma.". Hum Pathol 38 (9): 1305-9. doi:10.1016/j.humpath.2007.05.015. PMID 17707261.
- ↑ Sapre, N.; Pedersen, J.; Hong, MK.; Harewood, L.; Peters, J.; Costello, AJ.; Hovens, CM.; Corcoran, NM. (Dec 2012). "Re-evaluating the biological significance of seminal vesicle invasion (SVI) in locally advanced prostate cancer.". BJU Int 110 Suppl 4: 58-63. doi:10.1111/j.1464-410X.2012.11477.x. PMID 23194127.
- ↑ Lester, Susan Carole (2010). Manual of Surgical Pathology (3rd ed.). Saunders. pp. 409. ISBN 978-0-323-06516-0.
- ↑ Berney, DM.; Wheeler, TM.; Grignon, DJ.; Epstein, JI.; Griffiths, DF.; Humphrey, PA.; van der Kwast, T.; Montironi, R. et al. (Jan 2011). "International Society of Urological Pathology (ISUP) Consensus Conference on Handling and Staging of Radical Prostatectomy Specimens. Working group 4: seminal vesicles and lymph nodes.". Mod Pathol 24 (1): 39-47. doi:10.1038/modpathol.2010.160. PMID 20818343.
- ↑ Ross, HM.; Kryvenko, ON.; Cowan, JE.; Simko, JP.; Wheeler, TM.; Epstein, JI. (Sep 2012). "Do adenocarcinomas of the prostate with Gleason score (GS) ≤6 have the potential to metastasize to lymph nodes?". Am J Surg Pathol 36 (9): 1346-52. doi:10.1097/PAS.0b013e3182556dcd. PMID 22531173.