Marginal zone lymphoma
| Marginal zone lymphoma | |
|---|---|
| Diagnosis in short | |
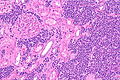
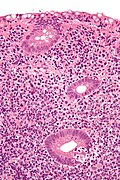
 Marginal zone lymphoma of the kidney. H&E stain. | |
|
| |
| LM | small lymphoid cells +/-plasmacytoid features +/-lymphoepithelial lesion |
| LM DDx | other small cell lymphomas, DLBCL |
| IHC | CD20 +ve, BCL2 +ve, CD21 +ve, CD43 +ve/-ve |
| Site | gastrointestinal tract, lymph nodes |
|
| |
| Prevalence | moderate |
| Endoscopy | +/-nodularity |
| Other | CD11c +ve (flow cytometry or laser scanning cytometry) |
Marginal zone lymphoma, abbreviated MZL, is a common type of lymphoma composed of small cells.
General
- The MALTomas arise in the context chronic infective or inflammatory conditions, e.g. Sjögren disease (salivary gland), Hashimoto thyroiditis (thyroid gland), Helicobacter pylori gastritis (stomach).[1]
Classification
- Comes in three different flavours:
- Extranodal marginal zone lymphoma.
- Splenic marginal zone lymphoma (SMZL).
- Nodal marginal zone lymphoma (NMZL).
Whilst there are some immunohistochemical differences between the 3 types, separating them out depends on clinical features and radiological findings, e.g. splenic marginal zone lymphoma with spread to lymph nodes may be indistinguishable from primary nodal marginal zone lymphoma.
Microscopic
Features:
- Small (lymphoid) cells that may be plasma cell-like (plasmacytoid):[2]
- +/-Clockface nucleus.
- +/-Eccentric nucleus.
- +/-"Lymphoepithelial lesion" - gastric crypts invaded by a monomorphous population of lymphocytes.[3]
- Features:
- Cluster of lymphocytes - three cells or more - key feature.
- Single lymphocytes don't count.
- Clearing around the lymphocyte cluster.
- Cluster of lymphocytes - three cells or more - key feature.
- Not specific for MALT lymphoma, i.e. may be seen in other types of lymphoma.[4]
- Features:
DDx:
- Other small cell lymphomas.
- Marginal zone hyperplasia
- DLBCL - should be a distinctive region at low power.[citation needed]
Images


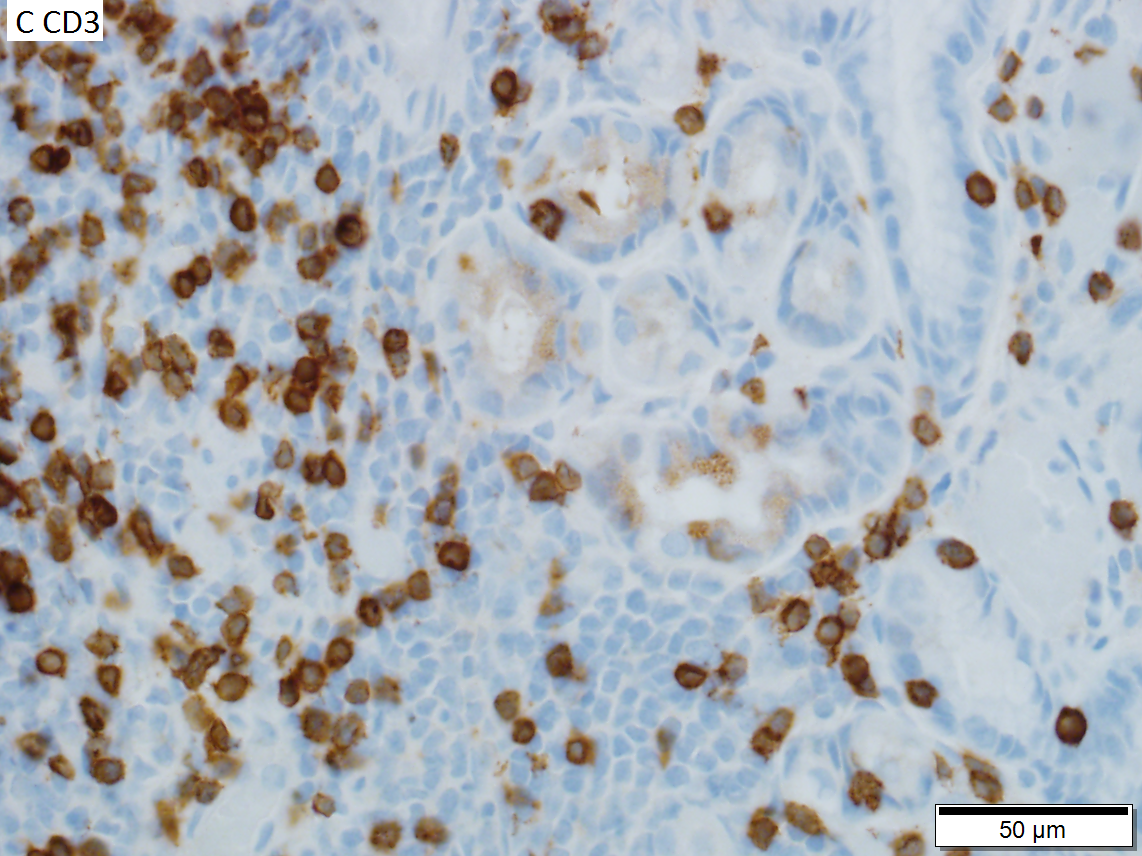

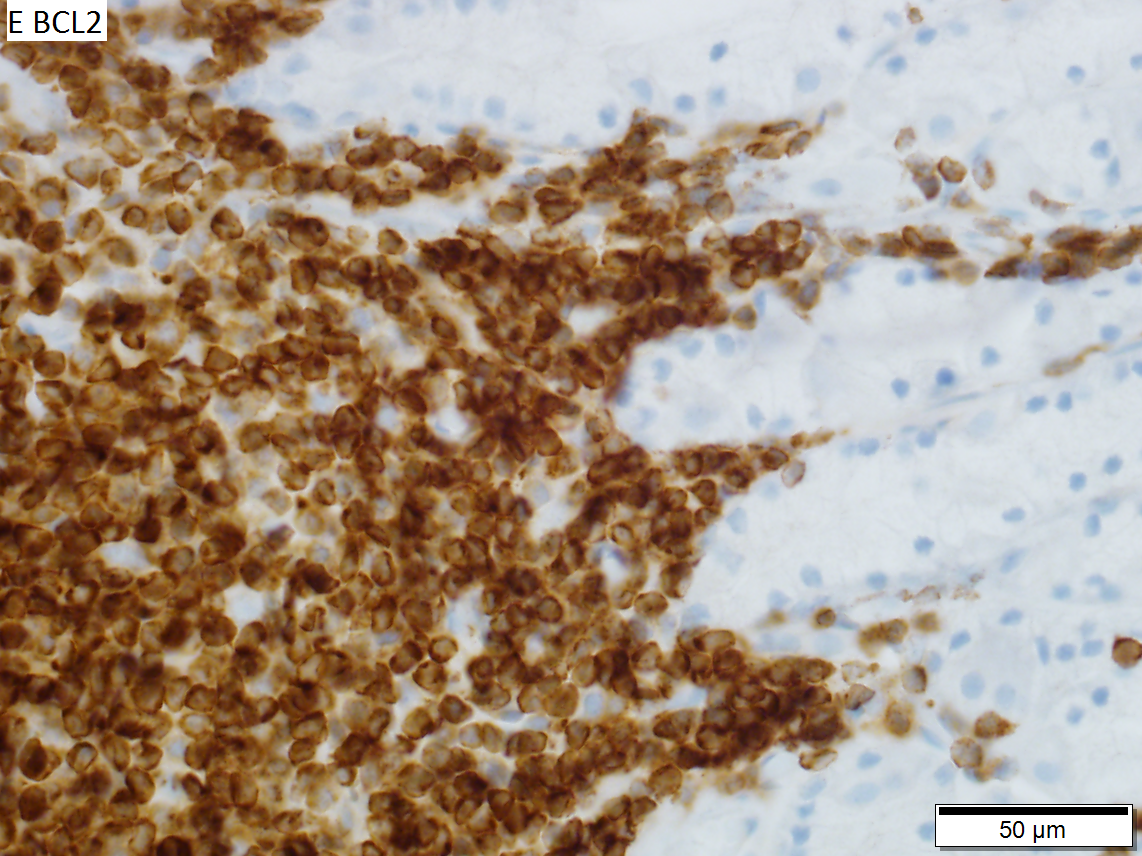
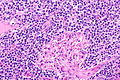
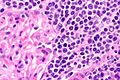
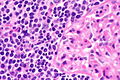
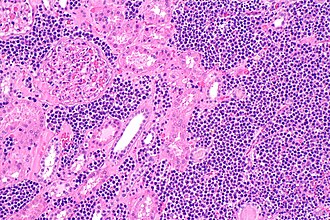
Extrazonal marginal zone lymphojma of mucosa-associates lymphoid tissue (MALT lymphoma) in stomach of 64 Year old man, identified in sleeve gastrectomy performed for weight loss. A. Predominantly submucosal blue masses without definite follicles. B. Small round to irregular lymphoid cells surround the most inferior pits. C. Non-neoplastic T cells are seen in abundance, sometime within pit epithelium. D. Neoplastic B cells mass and surround pits, but do not extensively invade the epithelium; lymphoepithelial lesions were not seen. E. Cancer cells expressed BCL2. Cancer cells were negative for CD5, CD10, and cyclin D1.
www:
Lymphoepithelial lesion
IHC
Features:[5]
- CD20 +ve.
- BCL2 +ve.
- CD21 +ve.
- CD11c +ve (flow cytometry or laser scanning cytometry - only; not available for paraffin).
- CD43 +ve/-ve.
- Typically positive in mantle cell lymphoma.
Others:
- CD5 -ve.
- CD10 -ve.
- CD23 -ve.
Molecular
There are several associated with MALT lymphoma:[6]
- t(11;18)(q21;q21) / API2‐MALT1[7] - most common translocation in MALT lymphoma.[8]
- t(14;18)(q32;q21) / IGH‐MALT1.
- Should not be confused with t(14;18) seen in follicular lymphoma between IGH-BCL2.[9]
- t(1;14)(p22;q32) / IGH‐BCL10.
The MALT1 associated translocations can be assessed with an ISH break apart probe for MALT1.
See also
References
- ↑ Mitchell, Richard; Kumar, Vinay; Fausto, Nelson; Abbas, Abul K.; Aster, Jon (2011). Pocket Companion to Robbins & Cotran Pathologic Basis of Disease (8th ed.). Elsevier Saunders. pp. 326. ISBN 978-1416054542.
- ↑ URL: http://surgpathcriteria.stanford.edu/bcell/marginalnodal/printable.html. Accessed on: 6 March 2012.
- ↑ Papadaki, L.; Wotherspoon, AC.; Isaacson, PG. (Nov 1992). "The lymphoepithelial lesion of gastric low-grade B-cell lymphoma of mucosa-associated lymphoid tissue (MALT): an ultrastructural study.". Histopathology 21 (5): 415-21. PMID 1452124.
- ↑ DB. 6 August 2010.
- ↑ Lester, Susan Carole (2005). Manual of Surgical Pathology (2nd ed.). Saunders. pp. 95. ISBN 978-0443066450.
- ↑ Bacon CM, Du MQ, Dogan A (April 2007). "Mucosa-associated lymphoid tissue (MALT) lymphoma: a practical guide for pathologists". J. Clin. Pathol. 60 (4): 361–72. doi:10.1136/jcp.2005.031146. PMC 2001121. PMID 16950858. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2001121/.
- ↑ Mitchell, Richard; Kumar, Vinay; Fausto, Nelson; Abbas, Abul K.; Aster, Jon (2011). Pocket Companion to Robbins & Cotran Pathologic Basis of Disease (8th ed.). Elsevier Saunders. pp. 170. ISBN 978-1416054542.
- ↑ Streubel, B.; Lamprecht, A.; Dierlamm, J.; Cerroni, L.; Stolte, M.; Ott, G.; Raderer, M.; Chott, A. (Mar 2003). "T(14;18)(q32;q21) involving IGH and MALT1 is a frequent chromosomal aberration in MALT lymphoma.". Blood 101 (6): 2335-9. doi:10.1182/blood-2002-09-2963. PMID 12406890.
- ↑ Vitolo, U.; Ferreri, AJ.; Montoto, S. (Jun 2008). "Follicular lymphomas.". Crit Rev Oncol Hematol 66 (3): 248-61. doi:10.1016/j.critrevonc.2008.01.014. PMID 18359244.