Salivary duct carcinoma
| Salivary duct carcinoma | |
|---|---|
| Diagnosis in short | |
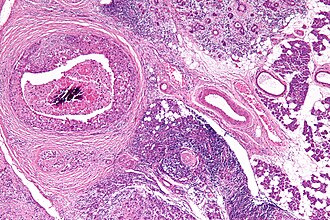 Salivary duct carcinoma. H&E stain. | |
|
| |
| LM | varied arch. (sheets, nests, cords, cribriform, micropapillary), neoplastic cells line-up around cystic spaces "Roman bridges", nuclear atypia, apocrine snouts, decapitation secretions |
| LM DDx | carcinoma ex pleomorphic adenoma with SDC component, ductal carcinoma of the breast |
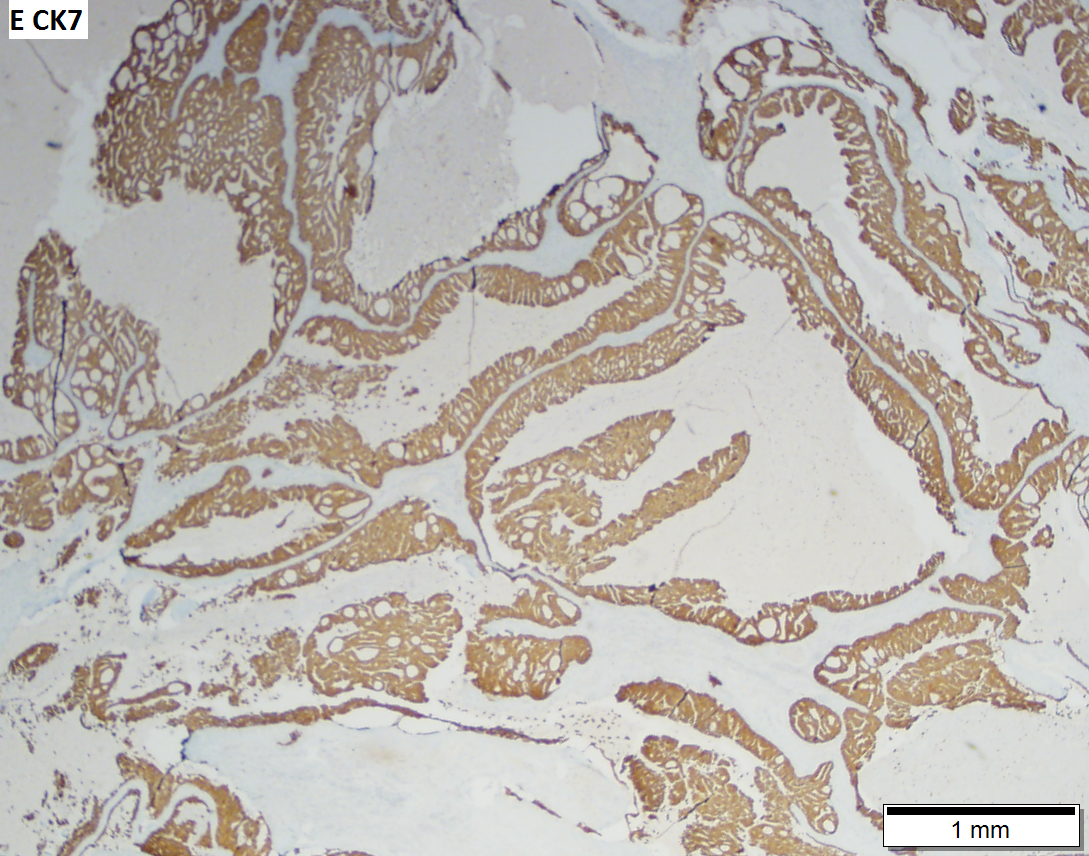
| IHC | LMWK, EMA, CK7, CK19 +ve, AR +ve, BRST2 (GCDFP-15) +ve, HER2 -ve/+ve, p63 -ve |
| Site | salivary gland - usu. parotid gland |
|
| |
| Clinical history | typically male, usu. >50 years old |
| Prevalence | rare |
| Prognosis | poor |
| Clin. DDx | other salivary gland tumours |
Salivary duct carcinoma, abbreviated SDC, is a rare salivary gland tumour that typically has an aggressive course.
General
- Malignant counterpart of salivary duct adenoma.
- Male:female ~= 4:1.
- Dismal prognosis.[1]
- Typically >50 years old.
- Mostly in the parotid.
Microscopic
Features - resembles ductal breast carcinoma:[1]
- Architecture: sheets, nests, cords, cribriform, micropapillary.
- Neoplastic cells line-up around cystic spaces "Roman bridges".
- Nuclear atypia (variation in size, shape, staining).
- Apocrine snouts - pseudopod-like/lollipop-like undulations of the cell membrane.
- Decapitation secretions - apocrine snouts (membrane bound blobs of cytoplasm) that have separated from its mother cell.
Notes:
- Similar to ductal breast carcinoma - key to remember.
DDx:
- Carcinoma ex pleomorphic adenoma with SDC component.
- Intraductal carcinoma of the salivary gland - previously referred to as low-grade salivary duct carcinoma.
Images
www:
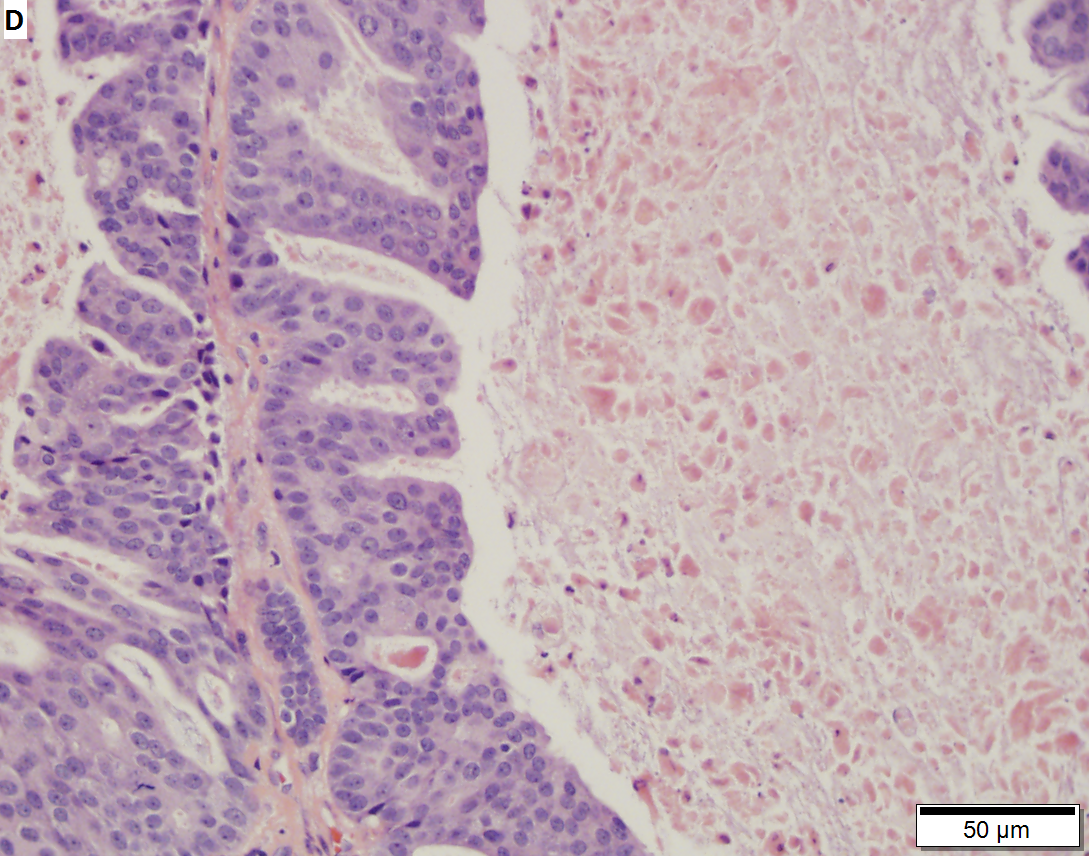
Salivary duct carcinoma. 59 y man with a 3 cm right superficial parotid mass. A. Low power shows a predominance of patterns similar to in situ, micropapillary (white arrow), Roman bridge (green arrow), cribriform (blue arrow) patterns. B. Careful search reveals occasional invasive bars (arrow). C. The bar comprises the usual invasive pattern of adenocarcinoma, with cancerous cell clusters, isolated glands, incomplete glands, and adjoined/fused glands. Note the lighter color of stromal desmoplasia (arrows). D. The in situ component has more uniform nuclei than the invasive component. Note the comedo necrosis. E. Cancer cells expressed CK7. F. Cancer cell nuclei were positive for androgen receptor. Not shown: tumor was negative for SOX10 and P63.
Subtypes
- Conventional.
- Mucinous - worse prognosis; opposite of what would one expect from the outcomes in breast cancer.
- Micropapillary - assoc. with a poor prognosis.
- Sarcomatoid/spindle cell.
IHC
- LMWK, EMA, CK7, CK19 +ve.
- p63 -ve.
- Androgen receptor +ve (~90% of cases).[2]
- BRST2 (GCDFP-15) +ve.
- HER2 +ve ~21%; use of trastuzumab (Herceptin) not systematically studied.
Curiosity:
See also
References
- ↑ 1.0 1.1 Rajesh, NG.; Prayaga, AK.; Sundaram, C.. "Salivary duct carcinoma: correlation of morphologic features by fine needle aspiration cytology and histopathology.". Indian J Pathol Microbiol 54 (1): 37-41. doi:10.4103/0377-4929.77321. PMID 21393874. http://www.ijpmonline.org/text.asp?2011/54/1/37/77321.
- ↑ Fan, CY.; Wang, J.; Barnes, EL. (Apr 2000). "Expression of androgen receptor and prostatic specific markers in salivary duct carcinoma: an immunohistochemical analysis of 13 cases and review of the literature.". Am J Surg Pathol 24 (4): 579-86. PMID 10757407.
- ↑ URL: http://www.cap.org/apps/docs/committees/cancer/cancer_protocols/2011/MajorSalGlands_11protocol.pdf. Accessed on: 3 April 2012.