Prostate cancer grading
Jump to navigation
Jump to search
This article deals with prostate cancer grading. It covers the Gleason System and the proposed Contemporary Prostate Cancer Grading System.
Gleason grading system
- AKA modified Gleason grading system.
Overview
- This system is only one any one talks about and there is consensus on how it is done.[1]
- Score range: 6-10.
- Technically 2-10... but almost no one uses 2-5.
- Reported on biopsy (and TURP) as: (primary pattern) + (highest non-primary pattern) = sum.
- Gleason score 3+4=7 means: pattern 3 is present and dominant, pattern 4 is the remainder of the tumour - but present in a lesser amount than pattern 3.
- Gleason score 4+5=9 means: pattern 4 is present and dominant, pattern 5 is present in a lesser amount that pattern 4. Pattern 3 may be present in a quantity less than pattern 4 or is absent.
- Reported as on prostatectomies as: (primary pattern) + (secondary pattern) = sum, (tertiary pattern)
- Tertiary Gleason pattern - definition: a pattern that is seen in less than 5% of the tumour (volume), that is higher grade than the two dominant patterns.[2]
- The presence of a tertiary patterns adversely affect the prognosis; however, the prognosis is not as bad as when the tertiary pattern is the secondary pattern, i.e. 3+4 tertiary 5 has a better prognosis than 3+5 (with some small amount of pattern 4).[2]
Testing yourself:
- There is a nice test-yourself quiz from Johns Hopkins: http://162.129.103.34/prostate/.
- It was studied in a paper by Kronz et al.[3]
Examples
- A biopsy with 80% pattern 4, 16% pattern 3 and 4% pattern 5... would be reported as: 4+5=9.
- A biopsy with 92% pattern 4, and 8% pattern 3... would be reported as: 4+3=7.
- A biopsy with 98% pattern 4, and 2% pattern 3... would be reported as: 4+4=8.
- A prostatectomy with 80% pattern 4, 16% pattern 3 and 4% pattern 5... would be reported as: 4+3=7 with tertiary pattern 5.
Grade groupings
- AKA prognostic Gleason grade groupings.
Proposed new system and old (modified) Gleason score:[4]
| Prognostic group | Gleason score |
|---|---|
| I | 3+3 |
| II | 3+4 |
| III | 4+3 |
| IV | 8 (4+4, 3+5, 5+3) |
| V | 9 or 10 (4+5, 5+4, 5+5) |
Rationale:
- Patients won't be told they have a 6 out of 10 cancer, and then think it is an intermediate grade cancer that is worrisome. Instead, they will be told they have a 1 out of 5 cancer.[4]
Gleason patterns (modified)
Gleason pattern 1 & 2
- Use strongly discouraged by a number of GU pathology experts.
Notes:
- Gleason pattern 1 - probably represents what today would be called adenosis.
- Should never be used.
- Gleason pattern 2 - used by few GU pathology experts occasionally.
- Generally, should not be diagnosed on core biopsies.[5]
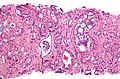
Gleason pattern 3
- Glands smaller than normal prostate glands + loss of epithelial folding.
- Can draw a line around each gland.
- May have gland branching.
- Glands have a X, U, V or Y shape.
Notes:
- Gland lumina should be seen.
- All cribriform is now, generally, classified as Gleason pattern 4.[5]
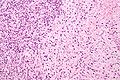
Gleason pattern 4
- Loss of gland lumina.
- Gland fusion.
- Benign looking cords ('hypernephroid pattern').
- Cribriform.
- Glomeruloid pattern - resembles a glomerulus.
Notes:
- One gland is not enough to call Gleason 4.
Images
www:
Gleason pattern 5
- Sheets.
- Must be differentiated from intraductal growth (which like in the breast are well circumscribed nests).
- Single cells.
- May be confused with stromal/lymphocytic infiltration.
- Look for nucleoli, cells should be round (prostatic stroma cells are spindle cells).
- May be confused with stromal/lymphocytic infiltration.
- Cords (strands).
- Line of cells.
- Should not be intermixed with clumps of cells (pattern 4).
- Nests of cells with necrosis (at the centre) (comedonecrosis) or (intraluminal) necrosis in a cribriform pattern.[1]
- Necrosis:
- Nuclear changes:
- Karyorrhexis (nuclear fragmentation).
- Pynosis (nuclear shrinkage).
- Karyolysis (nuclear dissolution).
- Cell ghosts (cells without a nucleus).
- Nuclear changes:
- Necrosis:
Notes:
- Pattern 5 may be under-diagnosed.
- Single cells is the most commonly missed pattern.[6]
Images
www:
Special types
Special types of prostate cancer have suggested Gleason patterns:[7]
| Special type | Gleason pattern | Comment |
|---|---|---|
| Ductal carcinoma | 4 | may be graded 3 or 5[8] |
| Mucinous carcinoma | 3 or 4 - dependent on morphology[9][10] | some advocate grade 4[7] |
| Sarcomatoid carcinoma | 5 | glands graded separately |
| Signet ring cell carcinoma | 5 | |
| Small cell carcinoma | not graded (ISUP 2005 consensus[1]) | may be graded 5[8] |
| Adenosquamous and squamous carcinoma | not graded | |
| Lymphoepithelioma-like carcinoma | not graded | |
| Adenoid cystic carcinoma | not graded | |
| Urothelial carcinoma | not graded | |
| Undifferentiated carcinoma, NOS | not graded |
How to remember the ones that aren't graded - think of Ur Lung carcinomas (Urothelial carcinoma, Lymphoepithelioma-like carcinoma):
- Small cell carcinoma.
- Squamous cell carcinoma.
- Adenosquamous carcinoma.
- Adenoid cystic carcinoma.
Biopsy-prostatectomy concordance of Gleason score
- Discordance is common.
- Upgrade on prostatectomy: 25-40%.
- Downgrade on prostatectomy: 5-15%.
Selected studies on concordance:
| Study | Upgrade | Downgrade | Notes |
|---|---|---|---|
| Sfoungaristos et al.[11] | 42.1% | 13.7% | high volume of tumour predicts upgrade |
| Thomas et al.[12] | 38.1% | 4.7% | |
| Truesdale et al.[13] | 23% | 11% |
Sign out
Upgrading
Gleason score upgrading on prostatectomy is considered relatively common; it is reported to occur in 23% to 42.1% of cases.[1][2] 1. BJU Int. 2011 107 (5): 749-54. 2. Can Urol Assoc J. 2012 Jan 24:1-5.
Downgrading
Gleason score downgrading on prostatectomy is considered uncommon; however, it is reported in 4.7% to 13.7% of cases.[1][2] 1. BJU Int. 2012 Jan; 109(2):214-9. 2. Can Urol Assoc J. 2012 Jan; 24;1-5.
Order of Gleason score components changed
COMMENT: The change in the order of the Gleason score components (3+4 on prostatectomy versus 4+3 on core biopsy) may be explained by sampling.
See also
References
- ↑ 1.0 1.1 1.2 Epstein, JI.; Allsbrook, WC.; Amin, MB.; Egevad, LL. (Sep 2005). "The 2005 International Society of Urological Pathology (ISUP) Consensus Conference on Gleason Grading of Prostatic Carcinoma.". Am J Surg Pathol 29 (9): 1228-42. PMID 16096414.
- ↑ 2.0 2.1 Zhou, Ming; Magi-Galluzzi, Cristina (2006). Genitourinary Pathology: A Volume in Foundations in Diagnostic Pathology Series (1st ed.). Churchill Livingstone. pp. 72. ISBN 978-0443066771.
- ↑ Kronz, JD.; Silberman, MA.; Allsbrook, WC.; Bastacky, SI.; Burks, RT.; Cina, SJ.; Mills, SE.; Ross, JS. et al. (Sep 2000). "Pathology residents' use of a Web-based tutorial to improve Gleason grading of prostate carcinoma on needle biopsies.". Hum Pathol 31 (9): 1044-50. doi:10.1053/hupa.2000.16278. PMID 11014569.
- ↑ 4.0 4.1 URL: http://urology.jhu.edu/newsletter/2014/prostate_cancer_2014_19.php. Accessed on: 28 March 2015.
- ↑ 5.0 5.1 Epstein, JI. (Feb 2010). "An update of the Gleason grading system.". J Urol 183 (2): 433-40. doi:10.1016/j.juro.2009.10.046. PMID 20006878. Cite error: Invalid
<ref>tag; name "pmid20006878" defined multiple times with different content - ↑ Fajardo, DA.; Miyamoto, H.; Miller, JS.; Lee, TK.; Epstein, JI. (Nov 2011). "Identification of Gleason pattern 5 on prostatic needle core biopsy: frequency of underdiagnosis and relation to morphology.". Am J Surg Pathol 35 (11): 1706-11. doi:10.1097/PAS.0b013e318228571d. PMID 21997691.
- ↑ 7.0 7.1 Grignon DJ (March 2004). "Unusual subtypes of prostate cancer". Mod. Pathol. 17 (3): 316–27. doi:10.1038/modpathol.3800052. PMID 14976541.
- ↑ 8.0 8.1 URL: https://www.bostwicklaboratories.com/global/physicians/medical-library/articles/gleason-grading.aspx. Accessed on: 26 November 2011.
- ↑ Osunkoya, AO.; Adsay, NV.; Cohen, C.; Epstein, JI.; Smith, SL. (Jul 2008). "MUC2 expression in primary mucinous and nonmucinous adenocarcinoma of the prostate: an analysis of 50 cases on radical prostatectomy.". Mod Pathol 21 (7): 789-94. doi:10.1038/modpathol.2008.47. PMID 18487999.
- ↑ Osunkoya, AO.; Nielsen, ME.; Epstein, JI. (Mar 2008). "Prognosis of mucinous adenocarcinoma of the prostate treated by radical prostatectomy: a study of 47 cases.". Am J Surg Pathol 32 (3): 468-72. doi:10.1097/PAS.0b013e3181589f72. PMID 18300802.
- ↑ Sfoungaristos, S.; Perimenis, P. (Jan 2012). "Clinical and pathological variables that predict changes in tumour grade after radical prostatectomy in patients with prostate cancer.". Can Urol Assoc J: 1-5. doi:10.5489/cuaj.11067. PMID 22277633.
- ↑ Thomas, C.; Pfirrmann, K.; Pieles, F.; Bogumil, A.; Gillitzer, R.; Wiesner, C.; Thüroff, JW.; Melchior, SW. (Jan 2012). "Predictors for clinically relevant Gleason score upgrade in patients undergoing radical prostatectomy.". BJU Int 109 (2): 214-9. doi:10.1111/j.1464-410X.2011.10187.x. PMID 21592293.
- ↑ Truesdale, MD.; Cheetham, PJ.; Turk, AT.; Sartori, S.; Hruby, GW.; Dinneen, EP.; Benson, MC.; Badani, KK. (Mar 2011). "Gleason score concordance on biopsy-confirmed prostate cancer: is pathological re-evaluation necessary prior to radical prostatectomy?". BJU Int 107 (5): 749-54. doi:10.1111/j.1464-410X.2010.09570.x. PMID 20840549.