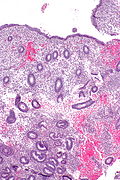
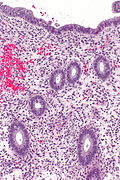
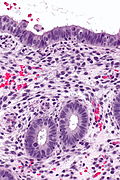
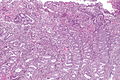
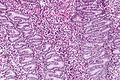
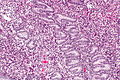
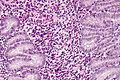
Proliferative phase endometrium
| Proliferative phase endometrium | |
|---|---|
| Diagnosis in short | |
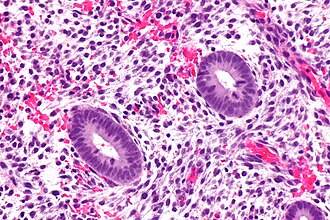 Proliferative endometrium. H&E stain. | |
|
| |
| LM | round spaced pseudostratified glands, mitoses (stroma and glands), normal gland-to-stroma ratio, no glandular dilation |
| LM DDx | disordered proliferative phase, simple endometrial hyperplasia, complex endometrial hyperplasia, early secretory phase endometrium |
| Site | endometrium |
|
| |
| Other | normal finding |
Proliferative phase endometrium, abbreviated PPE, is a very common diagnosis in endometrial specimens.
It is also known as proliferative endometrium.
General
- Day 1-13 in the protypical menstrual cycle of 28 days.
- May be day 5-13 - if the menstruation is not included.
- "Exodus" pattern is a term used to describe exfoliation of endometrial cells during the proliferative phase.
- On pap tests this is associated with the classic double contoured balls of endometrial epithelium and stroma.
- Proliferative activity is relatively common in postmenopausal women ~25% and probably associated with a small increased risk of malignancy.[1]
- ~17% of asymptomatic postmenopausal women have proliferative endometrium.[2]
Note:
- Proliferative phase = follicular phase.
- Gynecologists prefer the ovarian descriptor, i.e. follicular phase; pathologists go by what they see, i.e. proliferative endometrium.
- When the patient is >40 years, some advocate the use of the term proliferative type endometrium (instead of the term proliferative endometrium).[3]
Gross
- Thickened endometrium.
Microscopic
Features:[4]
- Glands:
- Straight, tubular, composed of tall pseudostratified columnar cells - key feature.
- Mitotic figures - key feature. †
- Stroma:
- Cellular stroma (spindle cells).
- Mitoses.
- Usually harder to find than in the glands.
Notes:
- † McCluggage says one shouldn't call PPE without mitoses, as some pseudostratification can be seen in atrophic endometrium.[4]
- There is no guidance on how hard one should look. Perhaps ~ 10 mm2 with the 20x objective? Ten millimetres squared represents approximately ~ 10 fields of view with a microscope that has a 22 mm eye piece.
- Significant negatives:
- No vacuolation.
- No mucus secretion.
- Inflammation (neutrophils, rare plasma cell) & stromal breakdown common early in the proliferative phase.[5]
DDx:
- Endometrial polyp.
- Disordered proliferative endometrium.
- Endometrial hyperplasia:
- Secretory phase endometrium, early - >=50% of gland have subnuclear vacuoles and >=50% of cells in the glands have subnuclear vacuoles.[6]
Images
Case 1
Case 2
Case 3
Coiled proliferative endometrium - low mag. (WC)
www
Sign out
Endometrium, Curettage: - Proliferative endometrium. - Scant benign endocervical mucosa present. - NEGATIVE for hyperplasia and NEGATIVE for malignancy.
ENDOMETRIUM, BIOPSY: - PROLIFERATIVE PHASE ENDOMETRIUM.
ENDOMETRIUM, ASPIRATION: - PROLIFERATIVE PHASE ENDOMETRIUM.
ENDOMETRIUM, BIOPSY: - PROLIFERATIVE PHASE ENDOMETRIUM. - ENDOCERVICAL MUCOSA AND STRIPPED ENDOCERVICAL EPITHELIUM WITHIN NORMAL LIMITS.
ENDOMETRIUM, BIOPSY: - PROLIFERATIVE ENDOMETRIUM, FOCALLY WITH A FIBROTIC STROMA. - BENIGN STRIPPED ENDOCERVICAL EPITHELIUM. - NEGATIVE FOR HYPERPLASIA AND NEGATIVE FOR MALIGNANCY.
ENDOMETRIUM, ASPIRATION: - EARLY PROLIFERATIVE PHASE ENDOMETRIUM WITH SOME SHEDDING (APOPTOTIC CELLS, INFILTRATING NEUTROPHILS, BALLS OF CONDENSED ENDOMETRIAL STROMA). - SCANT STRIPPED ENDOCERVICAL EPITHELIUM WITHIN NORMAL LIMITS. - NEGATIVE FOR HYPERPLASIA.
Not quite normal
ENDOMETRIUM, BIOPSY: - EARLY SECRETORY PHASE ENDOMETRIUM. - FOCUS OF CROWDED PROLIFERATIVE GLANDS, SEE COMMENT. COMMENT: There is a small focus of crowded and irregular proliferative glands without cytologic atypia. The possibility of a polyp is considered but the vessels and polyp-type stroma are lacking. Suggest clincal follow up with a consideration of a repeat biopsy in 3 to 6 months to rule out a hyperplastic lesion.
Post-menopausal
ENDOMETRIUM, BIOPSY: - PROLIFERATIVE TYPE ENDOMETRIUM. -- NEGATIVE FOR HYPERPLASIA. -- NEGATIVE FOR MALIGNANCY.
ENDOMETRIUM, BIOPSY: - PROLIFERATIVE-TYPE ENDOMETRIUM, LIMITED STROMA PRESENT. - STRIPPED ENDOCERVICAL EPITHELIUM WITHIN NORMAL LIMITS. - NO EVIDENCE OF HYPERPLASIA.
Mostly atrophic
ENDOMETRIUM, ASPIRATION: - FRAGMENTS OF PREDOMINANT INACTIVE, VERY WEAKLY PROLIFERATIVE ENDOMETRIAL EPITHELIUM ATTACHED TO A VERY SMALL AMOUNT OF UNREMARKABLE STROMA. - AMOUNT OF STROMA NOT SUFFICIENT TO ASSESS GLAND-TO-STROMA RATIO. - NO EVIDENCE OF HYPERPLASIA.
Micro
The sections show endometrium with proliferative glands without significant dilation or irregularity of shape. The gland-to-stroma ratio is within normal limits. Mitotic activity is mild. No nuclear atypia is apparent.
Compression artifact present
The sections show endometrium with proliferative glands without significant dilation or irregularity of shape. An increased gland density is seen focally, at the edge of one tissue fragment, in association with tearing of the stroma (compression artifact). The gland-to-stroma ratio is otherwise within normal limits. Mitotic activity is present. No nuclear atypia is apparent. Benign endocervical epithelium is present.
Minimal dilation and irregularity
- Used when it is a bit funny looking but not enough for disordered proliferative endometrium.
The sections show endometrium with proliferative glands. Rare mildly dilated glands (~2x surrounding) with minimal irregularity of shape are present. The gland-to-stroma ratio is within normal limits. Mitotic activity is present. No nuclear atypia is apparent.
See also
References
- ↑ Sivridis, E.; Giatromanolaki, A. (Aug 2004). "Proliferative activity in postmenopausal endometrium: the lurking potential for giving rise to an endometrial adenocarcinoma.". J Clin Pathol 57 (8): 840-4. doi:10.1136/jcp.2003.014399. PMID 15280405.
- ↑ Archer, DF.; McIntyre-Seltman, K.; Wilborn, WW.; Dowling, EA.; Cone, F.; Creasy, GW.; Kafrissen, ME. (Aug 1991). "Endometrial morphology in asymptomatic postmenopausal women.". Am J Obstet Gynecol 165 (2): 317-20; discussion 320-2. PMID 1872332.
- ↑ Gardiner G. January 2009.
- ↑ 4.0 4.1 McCluggage, WG. (Aug 2006). "My approach to the interpretation of endometrial biopsies and curettings.". J Clin Pathol 59 (8): 801-12. doi:10.1136/jcp.2005.029702. PMC 1860448. PMID 16873562. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1860448/.
- ↑ Nucci, Marisa R.; Oliva, Esther (2009). Gynecologic Pathology: A Volume in Foundations in Diagnostic Pathology Series (1st ed.). Churchill Livingstone. pp. 197. ISBN 978-0443069208.
- ↑ Mazur, Michael T.; Kurman, Robert J. (2005). Diagnosis of Endometrial Biopsies and Curettings: A Practical Approach (2nd ed.). Springer. pp. 14. ISBN 978-0387986159.
- ↑ URL: http://www.cytochemistry.net/microanatomy/medical_lectures/oviduct_and_uterus.htm. Accessed on: 23 October 2012.