Medical lung diseases
The medical lung diseases are a huge topic. Most pathologists have little to do with 'em. They are the domain of respirology. An introduction to lung pathology is in the lung article, along with a general approach. Interstitial lung disease is dealt with in the diffuse lung diseases article.
Infectious pneumonia
Includes:
Asthma
Emphysema
- Chronic obstructive pulmonary disease, abbreviated COPD, is dealt with in the emphysema article.
Chronic bronchitis
General
- Often seen together with emphysema with which it is lumped together with in the term COPD.
- It's a clinical diagnosis - criteria:[1]
- Cough with sputum for thee months in at least two consecutive years.
- No other cause identified.
Clinical:[1]
- Blue bloater (carbon dioxide retainers)
- Develop cor pulmonale.
Microscopic
Features:[1]
- Mucous gland hypertrophy + mucinous secretions in airway.
- Goblet cell metaplasia.
- Bronchiolar inflammation and fibrosis.
Pulmonary edema
General
- Seen in a number of conditions, e.g. congestive heart failure.
Gross
Features - autopsy:
- Bubbles - when squeezed (due to surfactant).
- Heavy.
Microscopic
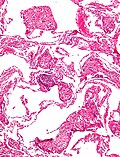
Features:[2]
- Dilated capillaries.
- Blood in airspace, focal.
- Plasma proteins in airspace - light pink acellular junk.
- +/-Hemosiderin-laden macrophages (known as heart failure cells in this context).
DDx:
- Pulmonary alveolar proteinosis.
- Pulmonary hemorrhage - abundant blood.
Images:
Bronchiectasis
General
- Benign.
- Uncommon.
- Predisposes for infection.[3]
- Usually a mixed flora.
- May be predominantly fungal, e.g. allergic bronchopulmonary aspergillosis (ABPA).
- Multitude of causes - including:
- Cystic fibrosis - typically diffusely involvement, unlike other causes.[4]
- Primary ciliary dyskinesia.
Gross
- Large airways at the periphery of the lung.
- Central airways larger than the adjacent arteries.
- Typically focal.
Radiologic:
- Central airways larger than the adjacent arteries.
- Airway wall-thickening.[5]
- "Tree-in-bud" abnormalities.
Images
www:
Microscopic
Features:
- Dilated airways.
- Airways larger than arteries.
Image
www:
Pulmonary hemorrhage
General
- Many causes.
A few causes:
- Trauma.
- Acute bronchopneumonia.
- Lung cancer, e.g. lung adenocarcinoma.
- Pulmonary hypertension.
- Infection, e.g. tuberculosis.
- Bronchiectasis.
Pulmonary hemorrhage syndromes:[6]
- Goodpasture syndrome.
- Idiopathic pulmonary hemosiderosis.
- Vasculitis-associated hemorrhage (hypersensitivity angiitis, Wegener's granulomatosis).
- Systemic lupus erythematosus.
Radiology
- Airspace opacity.
Microscopic
Features:
- Red blood cells in the airspaces - abundant.
- +/-Siderophages (hemosiderin-laden macrophages).
- Can count (distinct) granules (unlike in smoker's macrophages).
DDx:
- Decomposition.
Constrictive bronchiolitis
- AKA bronchiolitis obliterans, AKA obliterative broncholitis,[7] AKA bronchiolitis obliterans syndrome (BOS).[8]
General
- Not the same as (idiopathic) bronchiolitis obliterans organizing pneumonia (BOOP) - in short:
- BOOP: clogs the airway, has Masson bodies, treated with steroids - good prognosis.
- Constrictive bronchiolitis: fibrosis around airways, crappy prognosis.
- No good treatment.
- Progressive.
Etiology/associations:[7]
- Post-infectious.
- Viral, e.g. Adenovirus.
- Mycoplasma.
- Post-lung transplant.[9]
- Post-hematopoietic stem cell transplantation
- Associated with GVHD.[9]
- Connective tissue disease, mostly rheumatoid arthritis.
- Ulcerative colitis.
- Drugs - penicillamine.
- Toxins.
- Idiopathic.
Microscopic
Features:[7]
- Bronchiolitis - mononuclear and neutrophilic.
- May be minimal late in the disease.
- Fibrosis - submucosal and peribronchiolar.
- Can be patchy.
Notes:
- Bronchioles = noncartilagenous airways usu. < 2 mm in diameter.[7]
Images:
Stains
- Elastic trichrome - useful for delineation of obliterated bronchioles.
Diffuse lung diseases
These are also known as idiopathic interstitial pneumonias.
Fibrosis
Histomorphological classification
- Hyaline membranes - glassy pink material lining airways & alveoli.
- Microscopic honeycombing - "holes" in the lung.
- Bronchiolization - ciliated (respiratory) epithelium in distal airway.
- Uniform alveolar septal thickening - septae look similar at low power.
- Peripheral lobular fibrosis - septae thickening peripheral, HRCT shows: irregular peripheral reticular opacities.[10]
- Reticular = net-like.[11]
- Siderophages in alveoli - macrophages with hemosiderin the alveoli.
- Fibrinous pleuritis - peripheral only (based on imaging).
- Granulomata, non-necrotizing.
- Abundance of vacuolated cells.
- Chronic inflammation.
- Bronchiolocentric scarring - fibrosis concentrated around airway/assoc. with airway.
Radiologic/gross pathologic DDx by location
Causes of lower lung fibrosis BAD RASH:[12]
- Bronchiolitis obliterans organizing pneumonia (BOOP).
- Asbestosis.
- Drugs (nitrofurantoin, hydralazine, isoniazid (INH), amiodarone).
- Rheumatologic disease.
- Aspiration.
- Scleroderma.
- Hamman-Rich syndrome (really should be -- idiopathic pulmonary fibrosis).
Note:
- Hamman-Rich syndrome is another name for acute interstitial pneumonia.[13]
Causes of upper lung fibrosis FASSTEN:[12]
- Farmer's lung.
- Ankylosing spondylitis.
- Sarcoidosis.
- Silicosis.
- Tuberculosis (miliary).
- Eosinophilic granuloma.
- Neurofibromatosis.
Prognosis
- The pattern and severity of fibrosis seems to be the most important factors prognostically - more important than the underlying cause (ILD, CVD, drug reaction etc.).[14][15]
Patterns of fibrosis:
- "Linear" - follows alveolar walls, no architectural distortion.
- UIP-like (honeycombing).
Disease with fibrosis
There are many of 'em.
Fibrosing pleuritis
- AKA cryptogenic bilateral fibrosing pleuritis.
- Fibrous pleurisy redirect here.
General
- Benign.
- No asbestos exposure.[16]
Clinical:[16]
- Pleural thickening on imaging.
- Pleural effusion.
Microscopic
Features:[17]
DDx:[18]
- Mesothelioma, desmoplastic.
- Mesothelioma should not be diagnosed on core biopsy.[17]
Lymphocytic lesions of the lung
| Diagnosis | Key histologic feature | Radiology | Other diagnostic |
|---|---|---|---|
| Lymphocytic interstitial pneumonia | interstitial lymphoid cells, usu. no nodules | interstitial pattern | |
| Follicular bronchiolitis/bronchitis | lymphoid cell around bronchioles / bronchus, normal parenchyma | interstitial pattern | |
| Nodular lymphoid hyperplasia | abundant lymphoid cells in nodules | nodules /interstitial pattern | stains to exclude lymphoma; germinal centres do not exclude lymphoma |
| Lymphoma (BALToma) | abundant lymphoid cells usu. in nodules | nodules / interstitial pattern | may require stains to prove, germinal centres may be present |
Lymphocytic interstitial pneumonia
Follicular bronchitis/bronchiolitis
General
- Similar to lymphocytic interstitial pneumonia (LIP).
- Overlaps with LIP.[19]
- Associated with the things seen in LIP;[20] however, associations may be less clear in children.[21]
Gross/radiology
- No distinct nodule or mass.
- Classically: increased reticular marking, i.e. interstitial pattern.
Images: Intersitial pattern - radiographs (ucsf.edu).
Microscopic
Features:[22]
- Peribronchiolar/peribronchial lymphoid nodules with:
- Reactive germinal centres.
- Lack of these should raise suspicion for lymphoma.
- Plasma cells.
- Reactive germinal centres.
- +/-Lymphoid nodules in the interlobular septa.
Notes:
- Lung parenchyma distant from nodule = normal; no lymphocytic infiltrate.
DDx:
- Lymphoma, specifically MALTomas/BALTomas.
- Lymphocytic interstitial pneumonia.
- Nodular lymphoid hyperplasia.
- This is determined in part by radiology; it has nodules radiographically.
Pulmonary nodular lymphoid hyperplasia
General
- Definition - reactive lymphoid cells.
Gross/radiology
- Has nodules radiographically.
Microscopic
Features:[22]
- Reactive lymphoid nodules.
Notes:[23]
- Presence of germinal centres do not exclude lymphoma - may still be a BALToma.
- BALT = bronchial/bronchus associated lymphoid tissue.
DDx:
- Lymphoma, specifically MALTomas/BALTomas.
- Lymphocytic interstitial pneumonia.
- Follicular bronchiolitis.
Smoking associated disease
- RB = respiratory bronchiolitis.
- RBILD = respiratory bronchiolitis interstitial lung disease.
- DIP = desquamative interstitial pneumonia.
- Eosinophilic granuloma (of lung) - AKA pulmonary langerhans cell histiocytosis.
All of the above are assoc. with smoking. RBILD & DIP are considered by many to be on a continuum, i.e. RBILD is early DIP.
Respiratory bronchiolitis
- Diagnosis is based on clinical criteria.
Microscopic
Features:
- Inflammation.
- No interstitial lung disease, i.e. no fibrosis.
Respiratory bronchiolitis interstitial lung disease
Desquamative interstitial pneumonia
Pulmonary Langerhans cell histiocytosis
- AKA eosinophilic granuloma of the lung.
General
- Associated with smoking.[24]
- Not associated with systemic diseases of Langerhans cells (AKA Hand-Schueller-Christian disease).
Subtypes:[24]
- Cellular form.
- Fibrotic form.
One form usually predominates.
Radiology
- Upper lung zones.
Microscopic
Features:[25]
- Cellular peribronchiolar nodules with:
- Langerhans cells - key feature:
- Pale staining nucleus (H&E) with nuclear infolding - "crumpled tissue paper" appearance.
- +/-Smoker's macrophages (brown pigmented airspace macrophages).
- +/-Eosinophilia (may be rare) - significantly narrow DDx.
- Chronic inflammatory cells (lymphocytes). (???)
- Langerhans cells - key feature:
Images:
IHC
- Langerhans cells: S100+ and CD1a+.[25]
Granulomatous lung disease
- See: Granulomas for an introduction to the general topic.
Most common:
- Infectious - mycobacterial and fungal.[26]
Noninfectious causes:[26]
- Aspiration pneumonia.
- Hypersensitivity pneumonitis.
- Hot tub lung.
- Talc granulomatosis.
- Sarcoidosis.
- Wegener granulomatosis.
Sarcoidosis
General
- Diagnosis of exclusion - infection must be excluded.
- Radiologic differential diagnosis includes carcinomatosis.[27]
Microscopic
Features:
- Granulomata, well-formed, non-necrotizing.
Image(s):
Pulmonary talcosis
General
- Associated with herion use.[28]
- Seen in drug users that intravenously inject crushed pills intended to be taken PO.[29]
- X-ray findings similar to asbestosis.
Microscopic
Features:
- Granulomas with foreign material.
- Foreign material often polarizes.
Images
www:
Miscellaneous diseases
Pneumoconioses
Pneumocytoma
General
Epidemiology
- Female in 40s.[33]
- Considered benign; excision is curative.
- Rare case reports of metastases.
Gross
- Peripheral, solitary.
- Well-circumscribed.
Microscopic
Features:[33]
- Mixed cell population.
- Variable architecture:
- Papillary.
- Sclerotic.
- Solid.
- Hemorrhagic.
- +/-Granulomas.
DDx:[34]
- Papillary adenoma.
- Neuroendocrine tumour (carcinoid).
Image:
IHC
Features:[36]
- EMA +ve.
- PR +ve.[32]
Negative stains:[36]
- SMA -ve.
- CEA -ve.
- CD34 -ve.
- S100 -ve.
- Chromogranin A -ve.
Others:[31]
- TTF-1 +ve.
- HNF-3 alpha +ve.
- HNF-3 beta +ve.
Lymphangioleiomyomatosis
- Abbreviated LAM.
- AKA lymphangiomyomatosis.
Pulmonary alveolar proteinosis
- Abbreviated PAP.
Diffuse panbronchiolitis
- Abbreviated DPB.
General
- Rare lung disease predominantly found among asians.[37]
- Has been likened to cystic fibrosis - but doesn't really share any features with it.
Gross
Features:[37]
- Bronchiectasis.
- Hyperinflation.
- Small nodules (~2-3 mm) around the small airways.
- Diffuse involvement of both lungs.
Microscopic
Features:[37]
- Transmural inflammation of bronchioles - esp. respiratory bronchioles.
- Lymphocytes, plasma cells, histiocytes.
- Neutrophils within the airway.
Images:
Pulmonary amyloidosis
General
- Rare.[38]
Microscopic
Features:
- Interstitial cotton candy-like material - see amyloidosis.
DDx:
Images:
Drug reactions
- Effects are often non-specific.
Website: http://www.pneumotox.com
Pulmonary hypertension
General classification:
- Primary, i.e. primary pulmonary hypertension, or
- Secondary, e.g. due to congenital heart disease (like ventricular septal defect), interstitial pulmonary fibrosis.
Non-secondary pulmonary hypertension
Causes:[39]
- Primary pulmonary hypertension.
- Pulmonary embolic disease (thromboembolism, and non-thrombotic embolism).
- Pulmonary capillary haemangiomatosis (PCH).
- Pulmonary veno-occlusive disease (PVOD).
Severity
- Heath-Edwards classification - see pulmonary hypertension.
Eosinophilic pneumonia
Specific entities:[40]
- Churg-Strauss syndrome.
- Acute eosinophilic pneumonia.
- Chronic eosinophilic pneumonia.
- Eosinophilic granuloma (pulmonary histiocytosis X, Langerhans cell granulomatosis).
Entities which may have eosinophilia as prominent feature:
- AIDS.
- Lymphoma.
- Collagen vascular disease.
Churg-Strauss syndrome
Microscopic
Features:
- Small vessel vasculitis.
- Abundant eosinophils.
- Granulomas.
Eosinophilic pleural effusions
Causes - mnemonic I'M PAID:[42]
- Infection, e.g. tuberculosis.
- Malignancy - uncommon.
- Pulmonary emboli.
- Asbestos exposure.
- Inflammatory diseases.
- Drug reactions.
Lung transplant pathology
This subspecialty is dealt with in its own article.
See also
References
- ↑ 1.0 1.1 1.2 Mitchell, Richard; Kumar, Vinay; Fausto, Nelson; Abbas, Abul K.; Aster, Jon (2011). Pocket Companion to Robbins & Cotran Pathologic Basis of Disease (8th ed.). Elsevier Saunders. pp. 370. ISBN 978-1416054542.
- ↑ Klatt, Edward C. (2006). Robbins and Cotran Atlas of Pathology (1st ed.). Saunders. pp. 102. ISBN 978-1416002741.
- ↑ Kumar, Vinay; Abbas, Abul K.; Fausto, Nelson; Aster, Jon (2009). Robbins and Cotran pathologic basis of disease (8th ed.). Elsevier Saunders. pp. 693. ISBN 978-1416031215.
- ↑ URL: http://library.med.utah.edu/WebPath/LUNGHTML/LUNG053.html. Accessed on: 21 February 2012.
- ↑ Stockley, RA. (Jun 1998). "Commentary: bronchiectasis and inflammatory bowel disease.". Thorax 53 (6): 526-7. PMID 9713456.
- ↑ Cotran, Ramzi S.; Kumar, Vinay; Fausto, Nelson; Nelso Fausto; Robbins, Stanley L.; Abbas, Abul K. (2005). Robbins and Cotran pathologic basis of disease (7th ed.). St. Louis, Mo: Elsevier Saunders. pp. 745. ISBN 0-7216-0187-1.
- ↑ 7.0 7.1 7.2 7.3 Visscher, DW.; Myers, JL. (2006). "Bronchiolitis: the pathologist's perspective.". Proc Am Thorac Soc 3 (1): 41-7. doi:10.1513/pats.200512-124JH. PMID 16493150. http://pats.atsjournals.org/cgi/content/full/3/1/41.
- ↑ Sato, M.; Keshavjee, S. (2008). "Bronchiolitis obliterans syndrome: alloimmune-dependent and -independent injury with aberrant tissue remodeling.". Semin Thorac Cardiovasc Surg 20 (2): 173-82. doi:10.1053/j.semtcvs.2008.05.002. PMID 18707652.
- ↑ 9.0 9.1 Chien, JW.; Duncan, S.; Williams, KM.; Pavletic, SZ. (Jan 2010). "Bronchiolitis obliterans syndrome after allogeneic hematopoietic stem cell transplantation-an increasingly recognized manifestation of chronic graft-versus-host disease.". Biol Blood Marrow Transplant 16 (1 Suppl): S106-14. doi:10.1016/j.bbmt.2009.11.002. PMID 19896545.
- ↑ http://www.rsna.org/Publications/rsnanews/may06/jrnl_may06.cfm
- ↑ http://dictionary.reference.com/browse/reticular
- ↑ 12.0 12.1 Yeung, J.C.; Leonard, Blair J. N. (2005). The Toronto Notes 2005 - Review for the MCCQE and Comprehensive Medical Reference (2005 ed.). The Toronto Notes Inc. for Medical Students Inc.. pp. R13. ISBN 978-0968592854.
- ↑ Humphrey, Peter A; Dehner, Louis P; Pfeifer, John D (2008). The Washington Manual of Surgical Pathology (1st ed.). Lippincott Williams & Wilkins. pp. 90. ISBN 978-0781765275.
- ↑ Bjoraker JA, Ryu JH, Edwin MK, et al. (January 1998). "Prognostic significance of histopathologic subsets in idiopathic pulmonary fibrosis". Am. J. Respir. Crit. Care Med. 157 (1): 199-203. PMID 9445300. http://ajrccm.atsjournals.org/cgi/content/full/157/1/199.
- ↑ AC UBC S.425.
- ↑ 16.0 16.1 16.2 Buchanan, DR.; Johnston, ID.; Kerr, IH.; Hetzel, MR.; Corrin, B.; Turner-Warwick, M. (Apr 1988). "Cryptogenic bilateral fibrosing pleuritis.". Br J Dis Chest 82 (2): 186-93. PMID 3166932.
- ↑ 17.0 17.1 URL: http://www.ultrapath.org/oldsite/uscap/uscap05/meso1.html. Accessed on: 20 February 2012.
- ↑ Corson, JM. (Nov 2004). "Pathology of mesothelioma.". Thorac Surg Clin 14 (4): 447-60. doi:10.1016/j.thorsurg.2004.06.007. PMID 15559051.
- ↑ Nicholson AG (August 2001). "Lymphocytic interstitial pneumonia and other lymphoproliferative disorders in the lung". Semin Respir Crit Care Med 22 (4): 409–22. doi:10.1055/s-2001-17384. PMID 16088689.
- ↑ Aerni MR, Vassallo R, Myers JL, Lindell RM, Ryu JH (February 2008). "Follicular bronchiolitis in surgical lung biopsies: clinical implications in 12 patients". Respir Med 102 (2): 307–12. doi:10.1016/j.rmed.2007.07.032. PMID 17997299.
- ↑ Kinane BT, Mansell AL, Zwerdling RG, Lapey A, Shannon DC (October 1993). "Follicular bronchitis in the pediatric population". Chest 104 (4): 1183–6. PMID 8404188.
- ↑ 22.0 22.1 22.2 AFIP atlas of nontumour pathology. 2002. Vo. 2. P.277. ISBN 1-881041-79-4.
- ↑ AFIP atlas of nontumour pathology. 2002. Vo. 2. P.281. ISBN 1-881041-79-4.
- ↑ 24.0 24.1 Leslie, Kevin O.; Wick, Mark R. (2004). Practical Pulmonary Pathology: A Diagnostic Approach (1st ed.). Churchill Livingstone. pp. 234. ISBN 978-0443066313.
- ↑ 25.0 25.1 Leslie, Kevin O.; Wick, Mark R. (2004). Practical Pulmonary Pathology: A Diagnostic Approach (1st ed.). Churchill Livingstone. pp. 237. ISBN 978-0443066313.
- ↑ 26.0 26.1 Mukhopadhyay S, Gal AA (May 2010). "Granulomatous lung disease: an approach to the differential diagnosis". Arch. Pathol. Lab. Med. 134 (5): 667–90. PMID 20441499.
- ↑ URL: http://www.radiologyassistant.nl/en/46b480a6e4bdc. Accessed on: 23 May 2010.
- ↑ Davis, LL. (Dec 1983). "Pulmonary "mainline" granulomatosis: talcosis secondary to intravenous heroin abuse with characteristic x-ray findings of asbestosis.". J Natl Med Assoc 75 (12): 1225–8. PMC 2561715. PMID 6655726. http://www.ncbi.nlm.nih.gov/pmc/articles/PMC2561715/.
- ↑ Marchiori, E.; Lourenço, S.; Gasparetto, TD.; Zanetti, G.; Mano, CM.; Nobre, LF. (Apr 2010). "Pulmonary talcosis: imaging findings.". Lung 188 (2): 165-71. doi:10.1007/s00408-010-9230-y. PMID 20155272.
- ↑ Chan, KW.; Gibbs, AR.; Lo, WS.; Newman, GR. (Jun 1982). "Benign sclerosing pneumocytoma of lung (sclerosing haemangioma).". Thorax 37 (6): 404-12. PMID 6291188.
- ↑ 31.0 31.1 Yamazaki, K. (Jul 2004). "Type-II pneumocyte differentiation in pulmonary sclerosing hemangioma: ultrastructural differentiation and immunohistochemical distribution of lineage-specific transcription factors (TTF-1, HNF-3 alpha, and HNF-3 beta) and surfactant proteins.". Virchows Arch 445 (1): 45-53. doi:10.1007/s00428-004-1023-3. PMID 15138814.
- ↑ 32.0 32.1 Einsfelder, BM.; Müller, KM. (Sep 2005). "["Pneumocytoma" or "sclerosing hemangioma": histogenetic aspects of a rare tumor of the lung]". Pathologe 26 (5): 367-77. doi:10.1007/s00292-005-0751-8. PMID 15731902. Cite error: Invalid
<ref>tag; name "pmid15731902" defined multiple times with different content - ↑ 33.0 33.1 Keylock, JB.; Galvin, JR.; Franks, TJ. (May 2009). "Sclerosing hemangioma of the lung.". Arch Pathol Lab Med 133 (5): 820-5. PMID 19415961.
- ↑ URL: http://www.med.muni.cz/biomedjournal/pdf/2004/01/37_42.pdf. Accessed on: 17 June 2010.
- ↑ URL: http://moon.ouhsc.edu/kfung/jty1/Com/Com309-1-Diss.htm. Accessed on: 14 April 2012.
- ↑ 36.0 36.1 Rodriguez-Soto, J.; Colby, TV.; Rouse, RV. (Mar 2000). "A critical examination of the immunophenotype of pulmonary sclerosing hemangioma.". Am J Surg Pathol 24 (3): 442-50. PMID 10716159.
- ↑ 37.0 37.1 37.2 Poletti, V.; Casoni, G.; Chilosi, M.; Zompatori, M. (Oct 2006). "Diffuse panbronchiolitis.". Eur Respir J 28 (4): 862-71. doi:10.1183/09031936.06.00131805. PMID 17012632.
- ↑ Hagmeyer, L.; Stieglitz, S.; Röcken, C.; Randerath, W. (Jun 2012). "[Amyloidosis in Pneumology.]". Pneumologie. doi:10.1055/s-0032-1309811. PMID 22692971.
- ↑ Bush A (December 2000). "Pulmonary hypertensive diseases". Paediatr Respir Rev 1 (4): 361-7. doi:10.1053/prrv.2000.0077. PMID 16263465.
- ↑ http://emedicine.medscape.com/article/301070-overview
- ↑ Matthai, SM.; Kini, U. (Feb 2003). "Diagnostic value of eosinophils in pleural effusion: a prospective study of 26 cases.". Diagn Cytopathol 28 (2): 96-9. doi:10.1002/dc.10227. PMID 12561030.
- ↑ 42.0 42.1 Kalomenidis, I.; Light, RW. (Jul 2004). "Pathogenesis of the eosinophilic pleural effusions.". Curr Opin Pulm Med 10 (4): 289-93. PMID 15220754.