Difference between revisions of "Glycogenic acanthosis of the esophagus"
Jump to navigation
Jump to search
(+infobox) |
|||
| Line 35: | Line 35: | ||
*Uncommon - seen 3.5% of consecutive 2328 upper endoscopies.<ref name=pmid8409304>{{Cite journal | last1 = Vadva | first1 = MD. | last2 = Triadafilopoulos | first2 = G. | title = Glycogenic acanthosis of the esophagus and gastroesophageal reflux. | journal = J Clin Gastroenterol | volume = 17 | issue = 1 | pages = 79-83 | month = Jul | year = 1993 | doi = | PMID = 8409304 }}</ref> | *Uncommon - seen 3.5% of consecutive 2328 upper endoscopies.<ref name=pmid8409304>{{Cite journal | last1 = Vadva | first1 = MD. | last2 = Triadafilopoulos | first2 = G. | title = Glycogenic acanthosis of the esophagus and gastroesophageal reflux. | journal = J Clin Gastroenterol | volume = 17 | issue = 1 | pages = 79-83 | month = Jul | year = 1993 | doi = | PMID = 8409304 }}</ref> | ||
*Benign.<ref name=pmid25632181>{{Cite journal | last1 = Tsai | first1 = SJ. | last2 = Lin | first2 = CC. | last3 = Chang | first3 = CW. | last4 = Hung | first4 = CY. | last5 = Shieh | first5 = TY. | last6 = Wang | first6 = HY. | last7 = Shih | first7 = SC. | last8 = Chen | first8 = MJ. | title = Benign esophageal lesions: endoscopic and pathologic features. | journal = World J Gastroenterol | volume = 21 | issue = 4 | pages = 1091-8 | month = Jan | year = 2015 | doi = 10.3748/wjg.v21.i4.1091 | PMID = 25632181 }}</ref> | *Benign.<ref name=pmid25632181>{{Cite journal | last1 = Tsai | first1 = SJ. | last2 = Lin | first2 = CC. | last3 = Chang | first3 = CW. | last4 = Hung | first4 = CY. | last5 = Shieh | first5 = TY. | last6 = Wang | first6 = HY. | last7 = Shih | first7 = SC. | last8 = Chen | first8 = MJ. | title = Benign esophageal lesions: endoscopic and pathologic features. | journal = World J Gastroenterol | volume = 21 | issue = 4 | pages = 1091-8 | month = Jan | year = 2015 | doi = 10.3748/wjg.v21.i4.1091 | PMID = 25632181 }}</ref> | ||
*May be associated with [[GERD]];<ref name=pmid8409304/> however, lesions do not resolve with [[Proton pump inhibitor|PPI]] treatment.<ref name=pmid25632181/> | *May be associated with [[GERD]];<ref name=pmid8409304/><ref name=pmid22798107>{{Cite journal | last1 = Nazligül | first1 = Y. | last2 = Aslan | first2 = M. | last3 = Esen | first3 = R. | last4 = Yeniova | first4 = AÖ. | last5 = Kefeli | first5 = A. | last6 = Küçükazman | first6 = M. | last7 = Dülger | first7 = AC. | last8 = Celik | first8 = Y. | title = Benign glycogenic acanthosis lesions of the esophagus. | journal = Turk J Gastroenterol | volume = 23 | issue = 3 | pages = 199-202 | month = Jun | year = 2012 | doi = | PMID = 22798107 }}</ref> however, lesions do not resolve with [[Proton pump inhibitor|PPI]] treatment.<ref name=pmid25632181/> | ||
*Possible association with ingestion of hot liquids.<ref name=pmid20524767/> | *Possible association with ingestion of hot liquids.<ref name=pmid20524767/> | ||
Revision as of 10:24, 16 May 2015
| Glycogenic acanthosis of the esophagus | |
|---|---|
| Diagnosis in short | |
|
| |
| LM | squamous epithelium with (1) superficial clearing of the cytoplasm, and (2) thickening |
| Site | esophagus |
|
| |
| Associated Dx | gastroesophageal reflux disease (???) |
| Clinical history | ingestion of hot liquids (???) |
| Prevalence | uncommon |
| Endoscopy | raised grey/white lesions |
| Prognosis | benign |
Glycogenic acanthosis of the esophagus is an uncommon benign change of the esophagus with a distinctive endoscopic appearance.
General
- Uncommon - seen 3.5% of consecutive 2328 upper endoscopies.[1]
- Benign.[2]
- May be associated with GERD;[1][3] however, lesions do not resolve with PPI treatment.[2]
- Possible association with ingestion of hot liquids.[4]
Gross/endoscopic
- Distinctive endoscopic appearance - grey/white raised lesion.[4]
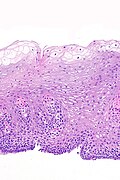
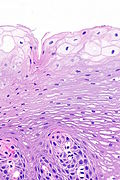
Image
Microscopic
Features:[4]
- Squamous epithelium with:
- Superficial clearing of the cytoplasm.
- Thickening.
Images
www
See also
References
- ↑ 1.0 1.1 Vadva, MD.; Triadafilopoulos, G. (Jul 1993). "Glycogenic acanthosis of the esophagus and gastroesophageal reflux.". J Clin Gastroenterol 17 (1): 79-83. PMID 8409304.
- ↑ 2.0 2.1 2.2 Tsai, SJ.; Lin, CC.; Chang, CW.; Hung, CY.; Shieh, TY.; Wang, HY.; Shih, SC.; Chen, MJ. (Jan 2015). "Benign esophageal lesions: endoscopic and pathologic features.". World J Gastroenterol 21 (4): 1091-8. doi:10.3748/wjg.v21.i4.1091. PMID 25632181.
- ↑ Nazligül, Y.; Aslan, M.; Esen, R.; Yeniova, AÖ.; Kefeli, A.; Küçükazman, M.; Dülger, AC.; Celik, Y. (Jun 2012). "Benign glycogenic acanthosis lesions of the esophagus.". Turk J Gastroenterol 23 (3): 199-202. PMID 22798107.
- ↑ 4.0 4.1 4.2 Lopes, S.; Figueiredo, P.; Amaro, P.; Freire, P.; Alves, S.; Cipriano, MA.; Gouveia, H.; Sofia, C. et al. (May 2010). "Glycogenic acanthosis of the esophagus: an unusually endoscopic appearance.". Rev Esp Enferm Dig 102 (5): 341-2. PMID 20524767.