Difference between revisions of "Gangliocytic paraganglioma"
Jump to navigation
Jump to search
(split out) |
(+infobox) |
||
| Line 1: | Line 1: | ||
{{ Infobox diagnosis | |||
| Name = {{PAGENAME}} | |||
| Image = Gangliocytic_paraganglioma_-_intermed_mag.jpg | |||
| Width = | |||
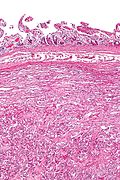
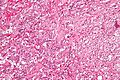
| Caption = Gangliocytic paraganglioma. [[H&E stain]]. | |||
| Synonyms = | |||
| Micro = | |||
| Subtypes = | |||
| LMDDx = | |||
| Stains = | |||
| IHC = | |||
| EM = | |||
| Molecular = | |||
| IF = | |||
| Gross = | |||
| Grossing = | |||
| Site = [[duodenum]] usually | |||
| Assdx = | |||
| Syndromes = | |||
| Clinicalhx = | |||
| Signs = +/-GI bleed | |||
| Symptoms = +/-abdominal pain | |||
| Prevalence = extremely rare | |||
| Bloodwork = | |||
| Rads = | |||
| Endoscopy = | |||
| Prognosis = | |||
| Other = | |||
| ClinDDx = | |||
| Tx = | |||
}} | |||
'''Gangliocytic paraganglioma''', abbreviated '''GP''', is an extremely rare tumour most often found in the [[duodenum]]. | '''Gangliocytic paraganglioma''', abbreviated '''GP''', is an extremely rare tumour most often found in the [[duodenum]]. | ||
Revision as of 19:14, 12 April 2014
| Gangliocytic paraganglioma | |
|---|---|
| Diagnosis in short | |
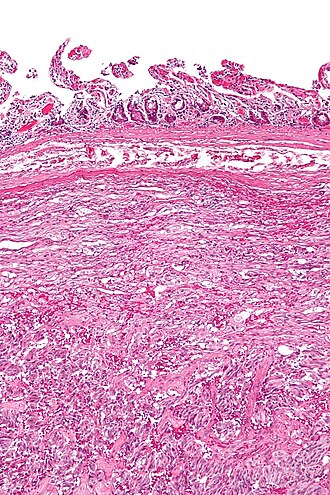 Gangliocytic paraganglioma. H&E stain. | |
| Site | duodenum usually |
|
| |
| Signs | +/-GI bleed |
| Symptoms | +/-abdominal pain |
| Prevalence | extremely rare |
Gangliocytic paraganglioma, abbreviated GP, is an extremely rare tumour most often found in the duodenum.
General
- Extremely rare.[1]
- May be associated with neurofibromatosis type 1.[2]
- Classified a neuroendocrine tumour.[3]
- Usually has a mix of the features seen in: neuroendocrine tumours, paragangliomas and ganglioneuromas.
Clinical - presentation:[4]
- GI bleed ~ 45% of cases.
- Abdominal pain ~ 43% of cases.
- Anemia ~ 15% of cases.
Gross
- Classically in the duodenum ~90% of cases.[4]
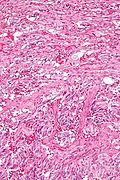
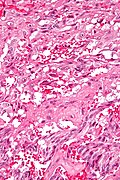
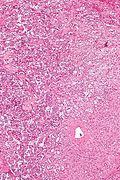
Microscopic
Features - three components:[5][6]
- Ganglion cells = large cells with:
- Round large nucleus.
- Prominent nucleolus.
- Moderate or abundant cytoplasm.
- Epithelioid cells (neuroendocrine component):
- Arranged in nests or cords.
- Stippled chromatin.
- Spindle cells (schwannian component):
- Moderate or abundant cytoplasm.
- Nucleus spindle-shaped or ellipsoid.
DDx:[5]
- Poorly differentiated carcinoma.
- Neuroendocrine tumour.
- Paraganglioma.
Images
www:
- Epithelioid cells of a GP (wjso.com).
- Ganglion cell in a GP (wjso.com).
- Ganglion cells in a GP (pubcan.org).[7]
- GP (surgicalpathologyatlas.com).
IHC
- Synaptophysin +ve.
- CD56 +ve.
- Chromogranin A +ve.
- HU +ve in ganglion-like cells.
- S100 +ve in spindle cells & sustentacular cells.
See also
References
- ↑ Wu, GC.; Wang, KL.; Zhang, ZT. (Jan 2012). "Gangliocytic paraganglioma of the duodenum: a case report.". Chin Med J (Engl) 125 (2): 388-9. PMID 22340577.
- ↑ Castoldi, L.; De Rai, P.; Marini, A.; Ferrero, S.; De Luca, V.; Tiberio, G. (2001). "Neurofibromatosis-1 and Ampullary Gangliocytic Paraganglioma Causing Biliary and Pancreatic Obstruction.". Int J Gastrointest Cancer 29 (2): 93-98. PMID 12754392.
- ↑ URL: http://www.cap.org/apps/docs/committees/cancer/cancer_protocols/2011/SmallbowelNET_11protocol.pdf. Accessed on: 29 March 2012.
- ↑ 4.0 4.1 Okubo, Y.; Wakayama, M.; Nemoto, T.; Kitahara, K.; Nakayama, H.; Shibuya, K.; Yokose, T.; Yamada, M. et al. (2011). "Literature survey on epidemiology and pathology of gangliocytic paraganglioma.". BMC Cancer 11: 187. doi:10.1186/1471-2407-11-187. PMID 21599949.
- ↑ 5.0 5.1 Wong, A.; Miller, AR.; Metter, J.; Thomas, CR. (Mar 2005). "Locally advanced duodenal gangliocytic paraganglioma treated with adjuvant radiation therapy: case report and review of the literature.". World J Surg Oncol 3 (1): 15. doi:10.1186/1477-7819-3-15. PMID 15740625.
- ↑ URL: http://surgpathcriteria.stanford.edu/gitumors/gangliocytic-paraganglioma/printable.html. Accessed on: 31 May 2012.
- ↑ URL: http://www.pubcan.org/printicdotopo.php?id=5028. Accessed on: 15 April 2012.