Difference between revisions of "Pancreas"
(→Solid pseudopapillary tumour: +images) |
(→Mucinous cystadenoma: +images) |
||
| Line 510: | Line 510: | ||
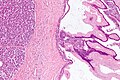
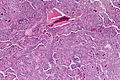
*"Ovarian-type stroma" under epithelium. | *"Ovarian-type stroma" under epithelium. | ||
**Ovarin-type stroma: high density of small (non-wavy) spindle cells with eosinophilic cytoplasm. | **Ovarin-type stroma: high density of small (non-wavy) spindle cells with eosinophilic cytoplasm. | ||
Notes: | Notes: | ||
*Appearance similar to ''mucinous cystadenoma'' in the [[ovarian tumours|ovary]]. | *Appearance similar to ''mucinous cystadenoma'' in the [[ovarian tumours|ovary]]. | ||
*Mucin stains +ve (intracytoplasmic). | *Mucin stains +ve (intracytoplasmic). | ||
=====Images===== | |||
<gallery> | |||
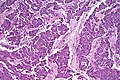
Image:Benign_pancreatic_mucinous_cystic_neoplasm_-_intermed_mag.jpg | Benign mucinous cystic neoplasm - intermed. mag. (WC) | |||
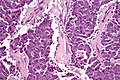
Image:Benign_pancreatic_mucinous_cystic_neoplasm_-_high_mag.jpg | Benign mucinous cystic neoplasm - should stroma (WC) | |||
<gallery> | |||
www: | |||
*[http://radiology.uchc.edu/eAtlas/Images/GYN/5705b.gif Mucinous cystadenoma - ovary (uchc.edu)]. | |||
====Borderline mucinous cystic tumour==== | ====Borderline mucinous cystic tumour==== | ||
Revision as of 23:55, 9 July 2013
The pancreas hangs-out in the upper abdomen. It occasionally is afflicited by cancers, the most common of which is very fatal.
Pancreatic cytopathology is dealt with in the gastrointestinal cytopathology article.
A general introduction to gastrointestinal pathology is in the gastrointestinal pathology article.
Introduction
Normal anatomy
Divided into three portions: head, body & tail:[1]
- Head:
- Includes unicate process.
- Extends to the left edge of the superior mesenteric vein (SMV) - by definition.
- All of the SMV is with the head.
- Body:
- Right edge of the superior mesenteric vein to the left edge of aorta - by definition.
- All of the aorta is with the body.
- Right edge of the superior mesenteric vein to the left edge of aorta - by definition.
- Tail:
- Remainder of pancreas.
Pancreatic surgeries
Common pancreatic surgeries include:
- Whipple procedure (AKA pancreaticoduodenal resection) - includes duodenum +/- stomach.
- Distal pancreatectomy.
- Removal of tail +/- body.
- Specimen usually comes with a spleen.
- Typically done form islet cell tumours.
- Total pancreatectomy.
- Specimen usually comes with a spleen.
Whipple procedure
- Proximal mucosal margin (stomach or duodenum).
- Distal mucosal margin (duodenum or jejunum).
- Bile duct margin.
- Pancreatic retroperitoneal (uncinate process) margin.
- At SB done on edge (not en face).
- Pancreatic neck transection margin (AKA distal pancreatic resection margin);[3] usu. en face and in toto.[4]
- Sometimes superior mesenteric vein (SMV).
- Rarely superior mesenteric artery (SMA) margin.
General classification of pancreatic tumours
- Metstatses.
- Most common = renal cell carcinoma.
- Primary.
- Endocrine.
- Usually small as hormonally active.
- Exocrine.
- Endocrine.
Pancreas neoplasms in a table
| Type | Key feature | Subtypes | Image | IHC | Detailed microscopic | Usual location | Other | DDx |
|---|---|---|---|---|---|---|---|---|
| Serous tumours | cuboidal cells, clear cytoplasm | cystadenoma, borderline t., cystadenocarcinoma | [1], (WC), (WC) | IHC? | cuboidal cells, clear cytoplasm, central nucleus | body or tail | cystadenoma may be assoc. with von Hippel-Lindau syndrome | clear cell RCC, oligomucinous mucinous tumours |
| Intraductal papillary mucinous tumour (IPMT) | mucin, no ovarian-like stroma | clear cell variant | (wjso.com), (upmc.edu) | IHC? | papillae, tall columnar mucin-producing cells | head | - | mucious neoplasms (other pancreatic, duodenal), intra-ampullary papillary-tubular neoplasm (see ampullary carcinoma) |
| Mucinous tumour | mucin, ovarian-like stroma | cystadenoma, borderline t., cystadenocarcinoma | (WC), (WC) | IHC? | tall columnar mucin-producing cells, ovarian-like stroma | body or tail | - | IPMT, metastatic mucinous tumours |
| Solid pseudopapillary tumour |
eosinophilic intracytoplasmic globules | clear cell variant (cytoplasm clear) | (WC), (bmj.com) | beta-catenin +ve, E-cadherin +ve, synaptophysin +ve, chromogranin -ve |
sheets of cells, focally loosely cohesive, eosinophilic cytoplasm, uniform nuclei with grooves | none (head, body or tail) | usu. younger women | ductal adenocarcinoma, neuroendocrine tumours |
| Ductal adenocarcinoma | irregular shaped glands, cytologic atypia | mucinous, spindle cell, mixed ductal-endocrine | (WC), (WC) | IHC? | glands, sheets, single cells, nuc. atypia, +/-mitoses, +/-necrosis | head | arises from the precursor PanIN | ampullary carcinoma, chronic pancreatitis |
| Pancreatoblastoma | squamoid nests, whorling | - | (nature.com) | CK7 (acinar comp.), CK8, CK18, CK19 | squamoid nests of cells, whorling, nested growth, +/-keratinization | none | usu. paediatric population | acinar cell carcinoma |
| Acinar cell carcinoma | acinar arch. | - | (WC), (histopathology-india.net) | trypsin, lipase | nests or trabeculae, nucleolus, mod. basophilic granular cytoplasm | head (slight predilection) | - | pancreatoblastoma |
| Undifferentiated carcinoma with osteoclast-like giant cells | giant cells | - | Image? | IHC? | giant cells, usu. with AIS or inv. ductal adenocarcinoma | head | - | anaplastic carcinoma |
| Chronic pancreatitis | fibrosis, loss of acinar tissue, preservation of lobular arch. | - | [2] | IHC? | loss of acinar tissue with preservation of islets, fibrosis | ? | not a neoplasm, included here as it is in the (clinical) DDx | ductal adenocarcinoma |
WHO classification
Benign epithelial:
Borderline epithelial:
- Mucinous cystic neoplasm with moderate dysplasia.
- Intraductal papillary mucinous neoplasm with moderate dysplasia.
- Solid pseudopapillary neoplasm
Malignant epithelial:
- Ductal adenocarcinoma.
- Mucinous noncystic carcinoma.
- Signet ring cell carcinoma.
- Adenosquamous carcinoma.
- Undifferentiated carcinoma.
- Undifferentiated carcinoma with osteoclast-like giant cells.
- Mixed ductal-endocrine carcinoma.
- Serous cystadenocarcinoma.
- Mucinous cystadenocarcinoma.
- Invasive.
- Noninvasive.
- Intraductal papillary mucinous carcinoma.
- Invasive.
- Noninvasive.
- Acinar cell carcinoma.
- Pancreatoblastoma.
- Solid pseudopapillary carcinoma.
Soft tissue tumours:
- See soft tissue lesions.
Ectopic pancreatic tissue
It comes in two flavours:[5]
- Pancreatic ectopia.
- Pancreatic (acinar) metaplasia.
Pancreatic acinar metaplasia
General
- Common in the GI tract.
- Found in ~ 20% of eosphageal biopsies above the GEJ.[7]
Gross
- May be a single lesion or a cluster of lesions.[6]
Microscopic
Features:
- Pancreatic acini - only.
- Intensely eosinophilic cytoplasm.
Negatives:
- No pancreatic ducts.
- No islets of Langerhans (pancreatic islets).
Images:
IHC
Features:[8]
- Trypase +ve.
- Lipase +ve.
Pancreatic ectopia
General
- May be confused with something pathologic.
Microscopic
Features:
- Consists of pancreatic acini and pancreatic ducts.
- +/-Islets of Langerhans.
Inflammatory
Pancreatitis
Classification
Etiology
Mnemonic I GET SMASHED:
- Idiopathic.
- Gallstones ~45%.
- Ethanol ~35%.
- Tumours (pancreas, ampulla).
- Scorpion bites, snake bites.
- Microbial - mumps (paramyxovirus), Epstein-Barr virus (EBV), cytomegalovirus (CMV), mycoplasma.
- Autoimmune - Crohn's disease, polyarteritis nodosa (PAN), systemic lupus erythematosus (SLE).
- Surgery/trauma, e.g. ERCP, motor vehicle collision.
- Hypercalcemia, hyperlipidemia/hypertriglyceridemia, hypothermia.
- Emboli, e.g. post-CABG.
- Drugs - SAND = steroids & sulfonamides, azathioprine, NSAIDs, diuretics, such as furosemide.
Acute pancreatitis
General
- Rarely comes to pathology.
- Usually diagnosed by abdominal CT, blood work (amylase, lipase).
Microscopic
Features:[9]
- Loss of acini.
- Neutrophils.
- Hemorrhage.
- +/-Loss of pancreatic islets.
Chronic pancreatitis
General
- May be confused with ductal adenocarcinoma radiologically... and pathologically.
- Often due to ethanol abuse.
Complications:[10]
- Malabsorption.
- Diabetes mellitus.
- Pseudocysts.
Autoimmune pancreatitis
Histologic subtypes of autoimmune pancreatitis:[11]
- Lymphoplasmacytic sclerosing pancreatitis (LPSP).
- Typically IgG4 positive -- one of the IgG4-related systemic diseases.
- Approximately 80% of cases.[12]
- Idiopathic duct-centric chronic pancreatitis (IDCP).
- Typically IgG4 negative.
- Approximately 20% of cases.
Lymphoplasmacytic sclerosing pancreatitis
General:
- Serum IgG4 +ve.[14]
Microscopic:
- Lymphoplasmacytic infiltrate.
IHC:
- Plasma cells IgG4 +ve.
Radiology
Plain film findings:
- Calcifications.
Microscopic
Features of chronic pancreatitis:[15]
- Preservation of lobular architecture - evenly spaced ductal units.
- Uniformly sized ductal elements.
- Smooth ductal contours.
- Ducts surrounded by acini or islets.
- Islets usu. preserved better than acini.[16]
- Intraluminal mucoprotein plugs.
Images:
Adenocarcinoma versus pancreatitis
This contrasts with the features of adenocarcinoma:[15]
- Ductal architecture:
- Random distribution of ductal structures.
- Irregular ductal contours.
- "Naked ducts in fat"; ducts without surrounding pancreatic elements or fibrous tissue.
- Ducts adjacent to arterioles.
- Nuclear atypia:
- Enlargement (>3 times the size of a lymphocyte).
- Pleomorphism.
- Distinct nucleoli.
- Hyperchromatic raisinoid nucleoli.
- Generally assoc. with malignancy:
- Perineural and vascular invasion (rare).
- Mitosis.
- Necrotic cellular debris (intraluminal).
Notes:
- Memory device: give 'em a fair chance at a benign diagnosis. Features suggestive of malignant:
- Fat, adjacent to.
- Arteriole, adjacent to.
- Irregular ducts.
- Random distribution of ducts/non-lobular arrangement.
IHC
- IgG4 +ve plasma cells -- IgG4 sclerosing disease.
Positive in pancreatic carcinoma:[17]
- p53.
- Mesothelin.
Cystic lesions - overview
General
- True cystic lesions are uncommon.
- A true cystic lesion: must have an epithelial lining.
- Only 10% of cystic lesions are true cystic lesions, i.e. 90% of cystic lesions are really pseudocysts.
- A true cystic lesion: must have an epithelial lining.
- It is hard to differentiate pseudocysts & cysts.
Cystic tumours - clinical
General:
- Usually diagnosed by imaging (CT/MRI, ERCP, Endoscopic ultrasound).
- 50% incidental finding.
- Vague symptoms
- Abdominal mass.
- Weight loss.
- Jaundice.
- Usually favourable prognosis - mostly benign.
Most important cystic lesions
- Serous.
- Mucinous.
- Ovarian-like stroma.
- Solid pseudopapillay tumours.
- Intraductal papillary mucinous tumour (IPMT).
- No ovarian-like stroma.
Mnemonic SIMS: Serous, IPMT, Mucinous, Solid pseudopapillary tumour.
Useful stains
- PAS-D.
Mucinous vs. IMPT
IMPT:
- No ovarian-like stroma.
- Usually has total pancreatectomy.
Cystic tumours of the pancreas
Khalifa's table of cystic tumours:
| Tumour | Usual sex | Age (years) | Usual site | Typical size (cm) |
Gross pathology |
|---|---|---|---|---|---|
| Serous microcystic adenoma |
female | 66 | body & tail | 11 | (joplink.net[18], (jhmi.edu)[19] |
| Intraductal papillary mucinous tumour (IPMT) |
male | 62 | head | 4 | (jhmi.edu)[19] |
| Mucinous tumour | female | 49 | body & tail | 10 | (rsna.org) |
| Solid pseudopapillary tumour |
female | 35 | any | 7.5 | (ajronline.org), (flickr.com/humpath) |
Cystic lesions
Serous tumours - overview
General
- Cell of origin: intralobular duct cells (ductular cells).
- Glycogen rich - but do not produce mucin.
Subclassication
- Serous microcystic adenoma (AKA serous cystadenoma[20]).
- Many small cysts.
- Serous oligocystic adenoma.
- Large cysts.
- Serous cystadenocarcinoma - very rare.[21]
Note:
- If one mucin +ve cell, tumour = a mucinous tumour.
Serous cystadenoma of the pancreas
General
- 1-2% of all exocrine pancreatic tumours.
- Female > male.
- Mean age 66 years.
- Truly benign with no malignant potenial.
- May be part of von Hippel-Lindau syndrome.
Management:
- Observe or resect.
Gross
Features:
- Classically has a characteristic central scar.[22]
- Bosulated surface.
- Lobulated.
- No (macroscopic) cysts apparent on gross.
- Location: 50-70% occur in the body and tail.
- Size: average size 11 cm.
Radiologic appearance:
- Honey comb-like appearance.
- Well demarcated border - may be described as a "coin lesion".
Image:
Microscopic
Features:
- Cystic spaces lined by cuboidal cells.
- Glycogen rich.
- Cilia. (???)
DDx:
- Renal cell carcinoma.
- Lymphangioma.
- Hemangioma.
- Oligocystic mucinous cystic tumors and pseudocysts.
- Have mucin; PAS-D could be used to demonstrate its presence.
Notes:
- Serous adenoma my coexist with aggressive tumours.
Images:
Stains
- PAS +ve.
- PASD -ve.
Mucinous cystic neoplasms of the pancreas
- Gastro-entero-pancreatic cell differentiation with hypercellular ovarian-type stroma.
- Stroma --> cellular.
- 2-2.5% of all exocrine pancreatic tumours.
- Almost exclusively in women.
- Mean age - 49 years.
- >80% in body and tail.
- Average size ~10 cm.
Note:
- Looks different than serous tumour.
Subclassification
- Mucinous cystadenoma.
- Borderline mucinous cystic tumour.
- Mucinous cystadenocarcinoma.
Borderline vs. Carcinoma
- Few mitoses in borderline.
Radiology
- Mucinous tumours: multilocular.
- Generally larger than serous.
- Often partially solid and cystic.
- Often calcified.
- Calcification rare in serous.
- Usually tail & body.
Microscopic
Mucinous cystadenoma
Features:[24]
- Simple tall columnar epithelium with large mucin vacuole on apical aspect.
- "Ovarian-type stroma" under epithelium.
- Ovarin-type stroma: high density of small (non-wavy) spindle cells with eosinophilic cytoplasm.
Notes:
- Appearance similar to mucinous cystadenoma in the ovary.
- Mucin stains +ve (intracytoplasmic).
Images
- Www:
- ====Borderline mucinous cystic tumour====
- Features:
- *May have finger like projections.
- *Pseudostratification of epithelium.
- Notes:
- * Surgery does not change based on diagnosis on frozen section.
- ** Only question is "Is the margin clear?".
- * Borderline tumours are rare.
- ====Carcinoma====
- *Cells floating in mucin.
- ====Mucinous tumour versus pseudocyst====
- ! Mucinous tumour
- ! Pseudocyst
- Prognosis:
- *Benign looking tumours have the potential to transform into carcinoma.
- *No report of assoc. pseudomyxoma peritonei.
- **US boards question -- it is an exception ... others one cause it.
- *Prognosis of m. cystadenocarcinoma is slightly better than that of ductal adenocarcinoma.
- ==Intraductal papillary mucinous tumour==
- *Abbreviated ''IPMT''.
- ===General===
- *Morphologically and biologically distinct from ductal adenocarcinoma, mucinous cystic tumour and ductal papillary hyperplasia.
- *Prognosis:
- ***Main duct (bad prognosis).
- ***Branch (good prognosis).
- Clinical:
- *Patient usually not jaundiced... as no obstruction.
- *Often diabetes... as pancreas is destroyed.
- *Patients may get a total pancreatectomy - as the disease is often multifocal.
- ====Epidemiology====
- *~1% of all exocrine pancreatic tumours.
- *More common in males.
- *Mean age at presentation 62 years.
- *60-80% occur in the head of the pancreas.
- *Average size 4 cm.
- ===Gross===
- *May be patchy/multifocal.
- *Multiple cystic spaces.
- ===Microscopic===
- Features:
- *Pancreatic duct lining cells jut into the duct lumen - papillomatous growth pattern.
- *Cytology:
- **Cell enlargement.
- ***Increased mucin production.
- **Nuclear changes:
- **Mitotic activity.
- Note:
- *No ovarian type stroma underneath (as seen in mucinous tumours).
- DDx:
- ====Classification of IMPT====
- =====Behaviour - Khalifa=====
- *Adenoma.
- *Borderline mucinous tumour.
- *Carcinoma.
- Notes:
- *Borderline tumours are rare.
- *If intralobular dilated ducts... carcinoma.
- *Any margin with mucin cells in thought to be badness!
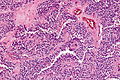
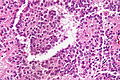
- ==Solid pseudopapillary tumour==
- ===General===
- *Obscure cell of origin.
- *Considered low grade, i.e. prognosis is usually good.
- ====Epidemiology====
- *Usually females (M:F=1:9).
- *Mean age of presentation third decade (20s).
- ====Management====
- May be followed radiologically.
- ===Microscopic===
- *Solid sheets of cells, focally dyscohesive.
- *Eosinophilic cytoplasm.
- **Focal eosinophilic (intracytoplasmic) globules - '''key feature'''.
- *Uniform nuclei with occasional nuclear grooves.
- *+/-Necrosis - creating spaces/cavities.
- ====Images====
www:
DDx
- Pancreatic pseudocyst.
- Cystadenoma.
- Cystadenocarcinoma.
- Pancreatic neuroendocrine tumour - may have cytoplasmic vacuolation, hyaline globules.[25]
IHC
Features:[25]
- Beta-catenin +ve ~100% (cytoplasmic & nuclear).
- E-cadherin +ve ~100% (cytoplasmic), -ve (membrane); antibody dependent.
- CD10 +ve ~ 80% (cytoplasmic + dot-like) key.
- Synaptophysin +ve (weak cytoplasmic) ~70%.
- Progesterone receptor +ve (nuclear) key.
Others:
- CD56 +ve.
- Chromogranin -ve.
Memory device PCB: PR (nuclear), CD10 (cytoplasmic), beta-catenin (cytoplasmic & nuclear).
Pre-malignant lesions
Pancreatic intraepithelial neoplasia
- Abbreviated PanIN.
General
- PanIN is thought to be the precursor lesion for pancreatic carcinoma.[26]
Overview
Putative preneoplasm-neoplasm-carcinoma sequence:
- PanIN1a.
- Not neoplastic, i.e. clonal.
- PanIN1b.
- Not neoplastic, i.e. clonal.
- PanIN2.
- Can be thought of as low-grade dysplasia, e.g. a (colonic) tubular adenoma without high-grade dysplasia.
- PanIN3.
- Can be thought of as high-grade dysplasia, e.g. (colonic) villous adenoma.
- May be referred to as carcinoma in situ.[27]
Microscopic
Features:[26]
- PanIN1a - increased amount of cytoplasm.
- Nuclear size & stratification perserved, arch. perserved.
- PanIN1b - increased amount of cytoplasm, folding of epithelium/moderated arch. distortion.
- Nuclear size & stratification perserved.
- PanIN2 - increased cell size, and nuclear enlargement (increased NC ratio), moderate nuclear atypia with loss of (basal) nuclear polarization.
- PanIN3 - marked nuclear atypia with increased NC ratio.
- No invasion identified.
- Pancreatic carcinoma - cytologic features of PanIN3 with definite invasion.
Images
www:
Solid tumours
Invasive ductal carcinoma of the pancreas
General
- Most common type of pancreatic cancer.[28]
- Location: usually in the head ~60%.
- 15% in the body, 5% tail, 20% diffuse (head, body & tail).[29]
- Abysmal prognosis.
Risk factors:[30]
- Smoking (RR ~ 2).
- Pancreatitis.
- Family history, esp. BRCA2.
- Diabetes mellitus - modest risk increase.
Molecular characteristics:[31][32]
- KRAS (oncogene) mutation in ~ 90% of cases.
- CDKN2A[33] (AKA p16) inactivation ~ 95% of cases.
- TP53 (AKA p53).
- SMAD4.
Microscopic
Features:[34]
- Often glandular, may be solid.
- Nuclei.
- May be bland - little pleomorphism.
- Often small nuclei.
- Sometimes coffee-bean appearance.
- Cytoplasm - granular, abundant.
- Quasi endocrine look.
- May stain positive for endocrine markers.
Other features:
- +/-Necrosis.
- +/-Myxoid degeneration.
- +/-Cells around vessels.
DDx:
Images:
- Pancreatic adenocarcinoma (WC).
- Pancreatic adenocarcinoma (WC).
- Normal pancreas, pancreatic intraepithelial neoplasia and pancreatic carcinoma (WC).
- Pancreatic adenocarcinoma - cytopathology (WC).
- Pancreatic adenocarcinoma - several images (upmc.edu).
IHC
Features:[35]
- CD7 +ve.
- CD20 +ve.
- SMAD4 -ve ~55% of cases -- stomach usually +ve.
- CDX2 -ve/+ve.
- CEA +ve.[36]
Pancreatic neuroendocrine tumour
- Abbreviated PanNET.[37]
- AKA pancreatic islet cell tumour[37] - considered to be an outdated term.
- AKA islet cell tumour - considered to be an outdated term.
General
- Rare.
- Presentation depends on subtype, e.g. for insulinoma the typical presentation is hypoglycemia.
- May be part of a syndrome:
Classification
Based on peptide produced in the pancreatic islets:
- Glucagon from alpha cells (glucagonoma).
- Insulin from beta cells (insulinoma) - most common ~ 50% of islet cell tumours.
- Somatostatin from D cells (somatostatinoma).
- Pancreatic polypeptide from PP cells.
Others:
- Vasoactive intestinal peptide (VIPoma).
- Gastrin (gastrinoma).
- May be seen in Zollinger-Ellison syndrome.
- Triad: pancreatic gastrinoma, gastric acid hypersecretion, marked peptic ulcers in the small bowel.[40]
- May be seen in Zollinger-Ellison syndrome.
Gross
Microscopic
Features:
- Nests of cells.
- Stippled chromatin.
- +/-Hyaline globules.
DDx:
Images:
- Islet cell tumour (upmc.edu).
- Pancreatic NET with features of SPT (upmc.edu).
- Pancreatic NET - another case (upmc.edu).
IHC
- CK19 +ve -- should be done as a routine in pancreatic NETs; poor prognostic factor.[42]
Note:
- CK19 should not be confused with CA19-9.
Acinar cell carcinoma of the pancreas
- Not to be confused with acinic cell carcinoma.
General
- Rare.
- Solid epithelial exocrine tumour.[44]
- Poor prognosis; mean survival of 18 months in one series.[45]
Clinical:[45]
- Increased serum lipase.
- Associated with arthralgias (joint pain).
- Classic presentation - Schmid triad:[46]
- Subcutaneous fat necrosis.
- Polyarthritis.
- Eosinophilia.
Gross
- Usually head of pancreas.
Microscopic
Features:[45]
- Cells reminiscent of pancreatic acinus cells:
- Granular, basophilic cytoplasm - usu. abundant.
- Round/oval nucleus.
- Nucleolus prominent.
- Architecture:
- Nests, sheets, trabecular, glandular.
DDx:
Images
www:
- Acinar cell carcinoma - several images (upmc.edu).
- Acinar cell carcinoma - several images (harvard.edu).
- Acinar cell carcinoma - 1 (nature.com).
- Acinar cell carcinoma - 2 (nature.com).[47]
Stains
Features:[45]
- PAS +ve (granular).
- PASD +ve.
IHC
- Trypsin +ve -- key stain.
- Lipase +ve.
- Chromogranin +ve (scattered, focal).
- CD56 -ve. (?)
Pancreatoblastoma
General
- Very rare.
- Tumour of childhood - age of diagnosis ~5 years old.[48]
- Prognosis ~80% year survival in children[49] more aggressive in adults.
- May be seen in adults.[50]
Associations:[51]
Microscopic
- Acinar-like structures.
- Squamoid corpuscles.
- Undifferentiated component.
Image:
IHC
Features:[52]
- CK7 +ve -- acinar, undifferentiated component.
- CK8 +ve -- squamous component.
- CK18 +ve -- squamous component.
- CK19 +ve -- squamous component.
See also
- Duodenum.
- Gallbladder.
- Gastrointestinal pathology.
- Von Hippel-Lindau syndrome.
- IgG4-related systemic disease.
References
- ↑ URL: http://www.cap.org/apps/docs/committees/cancer/cancer_protocols/2011/PancreasEndo_11protocol.pdf. Accessed on: 29 March 2012.
- ↑ URL: http://www.cap.org/apps/docs/committees/cancer/cancer_protocols/2011/SmallbowelNET_11protocol.pdf. Accessed on: 29 March 2012.
- ↑ Jamieson, NB.; Foulis, AK.; Oien, KA.; Going, JJ.; Glen, P.; Dickson, EJ.; Imrie, CW.; McKay, CJ. et al. (Jun 2010). "Positive mobilization margins alone do not influence survival following pancreatico-duodenectomy for pancreatic ductal adenocarcinoma.". Ann Surg 251 (6): 1003-10. doi:10.1097/SLA.0b013e3181d77369. PMID 20485150.
- ↑ URL: http://www.cap.org/apps/docs/committees/cancer/cancer_protocols/2011/PancreasEndo_11protocol.pdf. Accessed on: 6 April 2012.
- ↑ URL: http://test.pathologyportal.org/newindex.htm?92nd/specgasth2.htm. Accessed on: 14 March 2011.
- ↑ 6.0 6.1 Stachura, J.; Konturek, JW.; Urbanczyk, K.; Bogdal, J.; Mach, T.; Domschke, W. (Mar 1996). "Endoscopic and histological appearance of pancreatic metaplasia in the human gastric mucosa: a preliminary report on a recently recognized new type of gastric mucosal metaplasia.". Eur J Gastroenterol Hepatol 8 (3): 239-43. PMID 8724024.
- ↑ Johansson J, Håkansson HO, Mellblom L, et al. (March 2010). "Pancreatic acinar metaplasia in the distal oesophagus and the gastric cardia: prevalence, predictors and relation to GORD". J. Gastroenterol. 45 (3): 291–9. doi:10.1007/s00535-009-0161-4. PMID 20012917.
- ↑ Doglioni, C.; Laurino, L.; Dei Tos, AP.; De Boni, M.; Franzin, G.; Braidotti, P.; Viale, G. (Nov 1993). "Pancreatic (acinar) metaplasia of the gastric mucosa. Histology, ultrastructure, immunocytochemistry, and clinicopathologic correlations of 101 cases.". Am J Surg Pathol 17 (11): 1134-43. PMID 8214258.
- ↑ Klatt, Edward C. (2006). Robbins and Cotran Atlas of Pathology (1st ed.). Saunders. pp. 223. ISBN 978-1416002741.
- ↑ Mitchell, Richard; Kumar, Vinay; Fausto, Nelson; Abbas, Abul K.; Aster, Jon (2011). Pocket Companion to Robbins & Cotran Pathologic Basis of Disease (8th ed.). Elsevier Saunders. pp. 469. ISBN 978-1416054542.
- ↑ URL: http://path.upmc.edu/cases/case651/dx.html. Accessed on: 28 January 2012.
- ↑ 12.0 12.1 Kamisawa, T.; Takuma, K.; Tabata, T.; Inaba, Y.; Egawa, N.; Tsuruta, K.; Hishima, T.; Sasaki, T. et al. (Jan 2011). "Serum IgG4-negative autoimmune pancreatitis.". J Gastroenterol 46 (1): 108-16. doi:10.1007/s00535-010-0317-2. PMID 20824290.
- ↑ Ikeura, T.; Takaoka, M.; Uchida, K.; Shimatani, M.; Miyoshi, H.; Kusuda, T.; Kurishima, A.; Fukui, Y. et al. (2012). "Autoimmune pancreatitis with histologically proven lymphoplasmacytic sclerosing pancreatitis with granulocytic epithelial lesions.". Intern Med 51 (7): 733-7. PMID 22466829.
- ↑ Krasinskas, AM.; Raina, A.; Khalid, A.; Tublin, M.; Yadav, D. (Jun 2007). "Autoimmune pancreatitis.". Gastroenterol Clin North Am 36 (2): 239-57, vii. doi:10.1016/j.gtc.2007.03.015. PMID 17533077.
- ↑ 15.0 15.1 15.2 Adsay, NV.; Bandyopadhyay, S.; Basturk, O.; Othman, M.; Cheng, JD.; Klöppel, G.; Klimstra, DS. (Nov 2004). "Chronic pancreatitis or pancreatic ductal adenocarcinoma?". Semin Diagn Pathol 21 (4): 268-76. PMID 16273946.
- ↑ Klatt, Edward C. (2006). Robbins and Cotran Atlas of Pathology (1st ed.). Saunders. pp. 225. ISBN 978-1416002741.
- ↑ Hornick, JL.; Lauwers, GY.; Odze, RD. (Mar 2005). "Immunohistochemistry can help distinguish metastatic pancreatic adenocarcinomas from bile duct adenomas and hamartomas of the liver.". Am J Surg Pathol 29 (3): 381-9. PMID 15725808.
- ↑ URL: http://www.joplink.net/prev/200905/25.html. Accessed on: 15 February 2012.
- ↑ 19.0 19.1 URL: http://oac.med.jhmi.edu/cpc/cases/cpc5/cpc5_answer.html. Accessed on: 15 February 2012.
- ↑ 20.0 20.1 Mills, Stacey E; Carter, Darryl; Greenson, Joel K; Oberman, Harold A; Reuter, Victor E (2004). Sternberg's Diagnostic Surgical Pathology (4th ed.). Lippincott Williams & Wilkins. pp. 1630. ISBN 978-0781740517.
- ↑ Bano, S.; Upreti, L.; Puri, SK.; Chaudhary, V.; Sakuja, P. (Dec 2011). "Imaging of pancreatic serous cystadenocarcinoma.". Jpn J Radiol 29 (10): 730-4. doi:10.1007/s11604-011-0617-3. PMID 22009426.
- ↑ Kim YH, Saini S, Sahani D, Hahn PF, Mueller PR, Auh YH (2005). "Imaging diagnosis of cystic pancreatic lesions: pseudocyst versus nonpseudocyst". Radiographics 25 (3): 671–85. doi:10.1148/rg.253045104. PMID 15888617. http://radiographics.rsna.org/content/25/3/671.abstract.
- ↑ Vernadakis, S.; Kaiser, GM.; Christodoulou, E.; Mathe, Z.; Troullinakis, M.; Bankfalvi, A.; Paul, A. (2009). "Enormous serous microcystic adenoma of the pancreas.". JOP 10 (3): 332-4. PMID 19454830.
- ↑ Iacobuzio-Donahue, Christine A.; Montgomery, Elizabeth A. (2005). Gastrointestinal and Liver Pathology: A Volume in the Foundations in Diagnostic Pathology Series (1st ed.). Churchill Livingstone. pp. 489. ISBN 978-0443066573.
- ↑ 25.0 25.1 Serra S, Chetty R (November 2008). "Revision 2: an immunohistochemical approach and evaluation of solid pseudopapillary tumour of the pancreas". J. Clin. Pathol. 61 (11): 1153–9. doi:10.1136/jcp.2008.057828. PMID 18708424. http://jcp.bmj.com/content/61/11/1153.
- ↑ 26.0 26.1 Cotran, Ramzi S.; Kumar, Vinay; Fausto, Nelson; Nelso Fausto; Robbins, Stanley L.; Abbas, Abul K. (2005). Robbins and Cotran pathologic basis of disease (7th ed.). St. Louis, Mo: Elsevier Saunders. pp. 949. ISBN 0-7216-0187-1.
- ↑ Matthaei, H.; Hong, SM.; Mayo, SC.; dal Molin, M.; Olino, K.; Venkat, R.; Goggins, M.; Herman, JM. et al. (Nov 2011). "Presence of pancreatic intraepithelial neoplasia in the pancreatic transection margin does not influence outcome in patients with R0 resected pancreatic cancer.". Ann Surg Oncol 18 (12): 3493-9. doi:10.1245/s10434-011-1745-9. PMID 21537863.
- ↑ Humphrey, Peter A; Dehner, Louis P; Pfeifer, John D (2008). The Washington Manual of Surgical Pathology (1st ed.). Lippincott Williams & Wilkins. pp. 237. ISBN 978-0781765275.
- ↑ Cotran, Ramzi S.; Kumar, Vinay; Fausto, Nelson; Nelso Fausto; Robbins, Stanley L.; Abbas, Abul K. (2005). Robbins and Cotran pathologic basis of disease (7th ed.). St. Louis, Mo: Elsevier Saunders. pp. 950. ISBN 0-7216-0187-1.
- ↑ Mitchell, Richard; Kumar, Vinay; Fausto, Nelson; Abbas, Abul K.; Aster, Jon (2011). Pocket Companion to Robbins & Cotran Pathologic Basis of Disease (8th ed.). Elsevier Saunders. pp. 471. ISBN 978-1416054542.
- ↑ Mitchell, Richard; Kumar, Vinay; Fausto, Nelson; Abbas, Abul K.; Aster, Jon (2011). Pocket Companion to Robbins & Cotran Pathologic Basis of Disease (8th ed.). Elsevier Saunders. pp. 470-1. ISBN 978-1416054542.
- ↑ Furukawa, T. (Nov 2009). "Molecular pathology of pancreatic cancer: implications for molecular targeting therapy.". Clin Gastroenterol Hepatol 7 (11 Suppl): S35-9. doi:10.1016/j.cgh.2009.07.035. PMID 19896096.
- ↑ Online 'Mendelian Inheritance in Man' (OMIM) 600160
- ↑ Cotran, Ramzi S.; Kumar, Vinay; Fausto, Nelson; Nelso Fausto; Robbins, Stanley L.; Abbas, Abul K. (2005). Robbins and Cotran pathologic basis of disease (7th ed.). St. Louis, Mo: Elsevier Saunders. pp. 951. ISBN 0-7216-0187-1.
- ↑ Lester, Susan Carole (2010). Manual of Surgical Pathology (3rd ed.). Saunders. pp. 94. ISBN 978-0-323-06516-0.
- ↑ Adsay, NV.; Basturk, O.; Cheng, JD.; Andea, AA. (Oct 2005). "Ductal neoplasia of the pancreas: nosologic, clinicopathologic, and biologic aspects.". Semin Radiat Oncol 15 (4): 254-64. doi:10.1016/j.semradonc.2005.04.001. PMID 16183479.
- ↑ 37.0 37.1 Burns, WR.; Edil, BH. (Dec 2011). "Neuroendocrine Pancreatic Tumors: Guidelines for Management and Update.". Curr Treat Options Oncol. doi:10.1007/s11864-011-0172-2. PMID 22198808.
- ↑ Charlesworth, M.; Verbeke, CS.; Falk, GA.; Walsh, M.; Smith, AM.; Morris-Stiff, G. (Feb 2012). "Pancreatic Lesions in von Hippel-Lindau Disease? A Systematic Review and Meta-synthesis of the Literature.". J Gastrointest Surg. doi:10.1007/s11605-012-1847-0. PMID 22370733.
- ↑ Alexakis, N.; Connor, S.; Ghaneh, P.; Lombard, M.; Smart, HL.; Evans, J.; Hughes, M.; Garvey, CJ. et al. (2004). "Hereditary pancreatic endocrine tumours.". Pancreatology 4 (5): 417-33; discussion 434-5. doi:10.1159/000079616. PMID 15249710.
- ↑ Zollinger RM, Ellison EH (1955). "Primary peptic ulcerations of the jejunum associated with islet cell tumors of the pancreas". Ann. Surg. 142 (4): 709–23; discussion, 724–8. doi:10.1097/00000658-195510000-00015. PMC 1465210. PMID 13259432. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1465210/.
- ↑ 41.0 41.1 Oh, TG.; Chung, MJ.; Park, JY.; Bang, SM.; Park, SW.; Chung, JB.; Song, SY. (Sep 2012). "Prognostic factors and characteristics of pancreatic neuroendocrine tumors: single center experience.". Yonsei Med J 53 (5): 944-51. doi:10.3349/ymj.2012.53.5.944. PMC 3423842. PMID 22869477. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3423842/. Cite error: Invalid
<ref>tag; name "pmid22869477" defined multiple times with different content - ↑ Jain, R.; Fischer, S.; Serra, S.; Chetty, R. (Jan 2010). "The use of Cytokeratin 19 (CK19) immunohistochemistry in lesions of the pancreas, gastrointestinal tract, and liver.". Appl Immunohistochem Mol Morphol 18 (1): 9-15. doi:10.1097/PAI.0b013e3181ad36ea. PMID 19956064.
- ↑ Thomas, PC.; Nash, GF.; Aldridge, MC. (2003). "Pancreatic acinar cell carcinoma presenting as acute pancreatitis.". HPB (Oxford) 5 (2): 111-3. doi:10.1080/13651820310001153. PMID 18332967.
- ↑ URL: http://brighamrad.harvard.edu/Cases/bwh/hcache/380/full.html. Accessed on: 15 January 2012.
- ↑ 45.0 45.1 45.2 45.3 Klimstra, DS.; Heffess, CS.; Oertel, JE.; Rosai, J. (Sep 1992). "Acinar cell carcinoma of the pancreas. A clinicopathologic study of 28 cases.". Am J Surg Pathol 16 (9): 815-37. PMID 1384374.
- ↑ Jang, SH.; Choi, SY.; Min, JH.; Kim, TW.; Lee, JA.; Byun, SJ.; Lee, JW. (Feb 2010). "[A case of acinar cell carcinoma of pancreas, manifested by subcutaneous nodule as initial clinical symptom].". Korean J Gastroenterol 55 (2): 139-43. PMID 20168061.
- ↑ 47.0 47.1 Klimstra, DS. (Feb 2007). "Nonductal neoplasms of the pancreas.". Mod Pathol 20 Suppl 1: S94-112. doi:10.1038/modpathol.3800686. PMID 17486055.
- ↑ Glick, RD.; Pashankar, FD.; Pappo, A.; Laquaglia, MP. (May 2012). "Management of pancreatoblastoma in children and young adults.". J Pediatr Hematol Oncol 34 Suppl 2: S47-50. doi:10.1097/MPH.0b013e31824e3839. PMID 22525406.
- ↑ Bien, E.; Godzinski, J.; Dall'igna, P.; Defachelles, AS.; Stachowicz-Stencel, T.; Orbach, D.; Bisogno, G.; Cecchetto, G. et al. (Oct 2011). "Pancreatoblastoma: a report from the European cooperative study group for paediatric rare tumours (EXPeRT).". Eur J Cancer 47 (15): 2347-52. doi:10.1016/j.ejca.2011.05.022. PMID 21696948.
- ↑ Balasundaram, C.; Luthra, M.; Chavalidthamrong, D.; Chow, J.; Khan, H.; Endres, PJ. (May 2012). "Pancreatoblastoma: a rare tumor still evolving in clinical presentation and histology.". JOP 13 (3): 301-3. PMID 22572137.
- ↑ 51.0 51.1 Saif, MW. (2007). "Pancreatoblastoma.". JOP 8 (1): 55-63. PMID 17228135.
- ↑ 52.0 52.1 Nishimata, S.; Kato, K.; Tanaka, M.; Ijiri, R.; Toyoda, Y.; Kigasawa, H.; Ohama, Y.; Nakatani, Y. et al. (Jun 2005). "Expression pattern of keratin subclasses in pancreatoblastoma with special emphasis on squamoid corpuscles.". Pathol Int 55 (6): 297-302. doi:10.1111/j.1440-1827.2005.01829.x. PMID 15943785.
Further reading
Klimstra, DS.; Pitman, MB.; Hruban, RH. (Mar 2009). "An algorithmic approach to the diagnosis of pancreatic neoplasms.". Arch Pathol Lab Med 133 (3): 454-64. doi:10.1043/1543-2165-133.3.454. PMID 19260750.