Difference between revisions of "Amyloid"
Jensflorian (talk | contribs) (→General: new treatment options in TTR amyloidosis) |
|||
| Line 44: | Line 44: | ||
*May have a "cracked" appearance.{{fact}} | *May have a "cracked" appearance.{{fact}} | ||
DDx - ''ABCs'' of pink: | Classic DDx - ''ABCs'' of pink: | ||
*Amyloid. | *Amyloid. | ||
*Blood (fibrin). | *Blood (fibrin). | ||
*Collagen. | *Collagen. | ||
*Smooth muscle. | *Smooth muscle. | ||
Other considerations: | |||
*Foreign material (lifting agent "O'rise").<ref name=pmid31934919>{{cite journal |authors=Pezhouh MK, Burgart LJ, Chiu K, Cohen DA, Hutchings DA, Sanderson SO, Shirazi M, Stanich PP, VandenBussche CJ, Voltaggio L, Willhoit ED, Xue Y, Arnold CA |title=Characterization of Novel Injectable Lifting Agents Used in Colonic Polyp Removal: An Emerging Amyloid Mimic |journal=Am J Surg Pathol |volume=44 |issue=6 |pages=793–798 |date=June 2020 |pmid=31934919 |doi=10.1097/PAS.0000000000001435 |url=}}<ref> | |||
====Images==== | ====Images==== | ||
Revision as of 18:12, 25 March 2022
| Amyloid | |
|---|---|
| Diagnosis in short | |
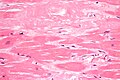
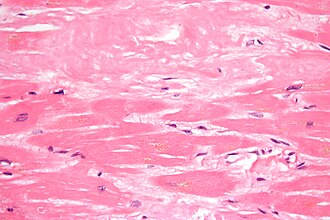 Cardiac amyloidosis. H&E stain. | |
|
| |
| LM | typically extracellular, amorphous (no specific shape), acellular and pink (on H&E stain) -- cotton candy like, classically has a "cracked" appearance |
| Subtypes | multiple subclassifications: Robbins (AL amyloidosis, AA amyloidosis, non-AA and non-AL), set of six subtypes (primary (AL amyloidosis), secondary (AA amyloidosis, hemodialysis-related, localized), hereditary, senile systemic amyloidosis) |
| LM DDx | fibrin, collagen, smooth muscle |
| Stains | Congo red +ve |
| EM | non-branching fine fibrils - usually 8-12 nm in diameter (accepted range 8-15 nm) |
| Molecular | beta sheet |
| Gross | waxy appearance |
| Site | pretty much anywhere, blood vessels |
|
| |
| Associated Dx | very many |
| Clinical history | variable |
| Prevalence | uncommon |
| Prognosis | dependent on subtype |
Amyloid is one of those things clinicians can put in many differential diagnoses. The pathologist can diagnose it.
This article is a general overview of the topic. Links are provided to articles that deal with amyloidosis at specific sites, see site specific section below.
Overview
Definition
- Disorder of protein folding - structure: beta sheet.[1]
Appearance
Light microscopy
Features:[2]
- Pink (on H&E stain).
- Extracellular location.
- Amorphous - no specific shape.
- May have a "cracked" appearance.[citation needed]
Classic DDx - ABCs of pink:
- Amyloid.
- Blood (fibrin).
- Collagen.
- Smooth muscle.
Other considerations:
- Foreign material (lifting agent "O'rise").Cite error: Closing
</ref>missing for<ref>tag - Fine fibrils, non-branching.
- Usually 8-12 nm in diameter; accepted range 8-15 nm.[3]
Images:
DDx
- CADASIL (cerebral autosomal dominant arteriopathy with subcortical infarcts and leukoencephalopathy).
- Typically has basophilic granularity in the blood vessels.[5]
Stains
- Congo red +ve.
- Positive:[6]
- Orange/light red (non-polarized light).
- Apple green birefringence (polarized light).
- Negative:
- Blue birefringence (polarized light) = collagen fibers.[7]
- Positive:[6]
- Thioflavin T stain.[8]
- Sodium sulphate-Alcian Blue stain +ve.[9]
Sign out
BONE LESION, RIGHT ILIAC, BIOPSY: - AMYLOID ASSOCIATED WITH HISTOCYTES, GIANT CELLS AND A FEW LYMPHOCYTES AND PLASMA CELLS. COMMENT: The presence of amyloid is confirmed with congo red staining and polarization. There are no histomorphologic findings suggestive of a plasma cell neoplasm in this biopsy. Clinical correlation with serum protein electrophoresis, urine protein electrophoresis and bone marrow sampling is suggested.
Associations - DDx
- Infections:[10][11]
- Tuberculosis.
- Leprosy.
- Chronic osteomyelitis.
- Bronchiectasis.
- Idiopathic conditions:
- Rheumatoid arthritis - relatively common (compared to others below).
- Anklyosing spondylitis - renal amyloidosis.
- Crohn's disease.[10]
- Familial Mediterranean fever.[10]
- Malignancy.
- Plasmacytoma.
- 5-15% of patients with multiple myeloma develop amyloidosis[12] - some say 10-20%.[10]
- Medullary thyroid carcinoma.
- Renal cell carcinoma.
- Plasmacytoma.
- Many other conditions...
Classification
Amyloidosis can be classified a number of different ways.
Six subtypes classification
Amyloid classified into six groups:[6]
- Primary (AL amyloidosis).
- Monoclonal light chains in serum and/or urine, may be due to plasma cell dyscrasia.
- Secondary (AA amyloidosis).
- Infections (osteomyelitis), neoplasia (Hodgkin's lymphoma).
- Hemodialysis-related.
- Beta-2 microglobulin.[13]
- Localized.
- Abeta amyloid found in Alzheimer's disease.
- Pancreatic amyloid deposition associated with diabetes mellitus type 2.[14]
- Image: Amyloid in DM (med.utah.edu).[15]
- Hereditary.
- Senile systemic amyloidosis.
How to remember: Two As = secondary amyloidosis.
Three main types - Robbins classification
Amyloid classified into three groups:[1]
- AL amyloidosis - "AL" = Amyloid Light chain.[16]
- AA amyloidosis - "AA" = Amyloid Associated.[18]
- Secondary amyloidosis.
- Abeta amyloid - found in Alzheimer's disease.[19]
Additional types:
- ATTR = Amyloid Transthyretin (TTR)
- Transthyretin - serum protein that transport thyroxine and retinol; transthyretin AKA prealbumin.
Treatment
The very short version:
Classification of amyloid - differentiation
Biochemical techniques
- Pre-treated with potassium permanganate, to obliterate congo red reactivity, was though be definitive for AA amyloidosis;[20] this is now generally considered to be unreliable.[21]
Immunohistochemistry
Possibly useful immunostains:
- Kappa.
- Lambda.
- Transthyretin.
- The name transthyretin is from transports thyroxine and retinol (previous unknown as prealbumin).
Mass spectroscopy
- Can be typed using mass spectroscopy.[25]
- Considered to be the definitive test.[24][26]
- High specificity and sensitivity vis-à-vis clinicopathologic correlation.[27]
- May be done on formalin-fixed paraffin embedded (FFPE) material.[27]
- Considered to be the definitive test.[24][26]
Types
Secondary amyloidosis
- AKA AA amyloidosis.
- Pathophysiology: acute-phase reactant serum amyloid A (SAA) - degraded + deposits.[10][28]
Cerebral amyloid angiopathy
A common cause of lobar hemorrhage (cerebral cortex, cerebellar cortex) in the elderly.
Senile systemic amyloidosis
- Abbreviated SSA.
General
- Previously known as senile cardiac amyloidosis.[29]
- May be referred to as ATTR = amyloidosis TTR; in SSA the TTR is not mutated, some call it: wt transthyretin amyloidosis (ATTR).
- There is a hereditary form of amyloidosis with mutated TTR deposition known as ATTR type FAP = ATTR type Familial Amyloid Polyneuropathy.
- Hereditary TTR: deposits in the heart, nerves and leptomeningeal amyloidosis.
- There is a hereditary form of amyloidosis with mutated TTR deposition known as ATTR type FAP = ATTR type Familial Amyloid Polyneuropathy.
Epidemiology:
- Common in the elderly, as the word senile suggests.
- Found in approx. 25% of elderly over 80 years old,[29] and in upto 65% of patients over 90 years old.[30]
Treatment:
- Liver transplantation, RNAi therapy (patisiran) and antisense oligonucleotides (inotersen).[31]
Gross pathology
- Grey/black "peppering" of left atrial endocardium - in fixed specimens.[32]
- "Peppering" should be present if severe.
Microscopic
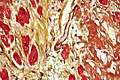
Features:
- Heart most commonly involved, followed by lungs and then by kidney (renal papilla).
- DDx of pink of H&E is important to remember: amyloid, muscle, collagen, clotted blood.
- Amyloid vs. Fibrosis? Subendocardial fibrosis may have rim of (diffusion) preserved myocytes. (???)
- Amyloid often present in the subepicardial tissue[30] - less commonly affected by ischemia.
Images
Site specific
Abdomen
- Abdominal fat pad biopsy redirects here.
General
- Abdominal fat pad biopsy - common screen for amyloidosis.
- May be done with FNA.
- Suffers for poor sensitivity.[7]
- May be done with FNA.
Microscopic
Features:
- Small-to-intermediate sized arteries with a thickened amorphous eosinophilic media.
- Thickening classically nodular.
- Apple green-birefringence -- with polarization.
Note:
- Evaluation of at least 15 small blood vessels is recommended.[7]
Sign out
SOFT TISSUE, ABDOMEN, BIOPSY: - AMYLOIDOSIS.
Negative
SOFT TISSUE, ABDOMEN, BIOPSY: - BENIGN FIBROADIPOSE TISSUE. - NEGATIVE FOR AMYLOIDOSIS WITH CONGO RED STAINING AND POLARIZED LIGHT. COMMENT: Correlation with serum protein electrophoresis, urine protein electrophoresis and bone marrow sampling should be considered within the clinical context.
Cardiac amyloidosis
General
- Common cause of restrictive cardiomyopathy.[33]
Cardiac amyloidosis - subtypes:
- AL amyloidosis - associated with plasma cell dyscrasia - most common cardiac amyloidosis.[30]
- Senile systemic amyloidosis - TTR-related amyloidosis (unmutated TTR).
- Hereditary amyloidosis.
- AA amyloidosis is uncommon.
Clinical:
- CHF, conduction abnormalities.
- Kidney disease (proteinuria) - associated with AL amyloidosis.
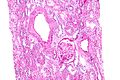
Pulmonary amyloidosis
- Very rare.
Renal amyloidosis
General
- Both AL and AA amyloidosis can affect the kidney.[8]
Clinical:
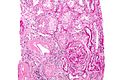
Microscopic
Features:
- Paucicellular mesangial expansion.
- Fluffy hyaline material in medium-sized blood vessels.
DDx:
- Diabetic nephropathy.
- Idiopathic nodular glomerulosclerosis.
- Light chain deposition disease.
- Fibrillary glomerulopathy.
- Immunotactoid glomerulopathy.
Images
www:
Urinary bladder amyloidosis
GI amyloidosis
- GI amyloidosis can lead to obstruction and usually is greatest in the small bowel.[6]
Liver amyloidosis
Features:
- Parenchymal deposition (common).
- Portal triad deposition (less common).
Gastric amyloidosis
Bone
Amyloid is reported in association with:
- Multiple myeloma ~40% of patients in one series.[35]
- Chronic osteomyelitis ~10% of patients in one series.[36]
- Diabetes (one case).[37]
See also
References
- ↑ 1.0 1.1 Lachmann HJ, Hawkins PN (2006). "Amyloidosis and the lung". Chron Respir Dis 3 (4): 203-14. PMID 17190124. http://crd.sagepub.com/cgi/pmidlookup?view=long&pmid=17190124.
- ↑ Cotran, Ramzi S.; Kumar, Vinay; Fausto, Nelson; Nelso Fausto; Robbins, Stanley L.; Abbas, Abul K. (2005). Robbins and Cotran pathologic basis of disease (7th ed.). St. Louis, Mo: Elsevier Saunders. pp. 259. ISBN 0-7216-0187-1.
- ↑ Alpers, CE.; Kowalewska, J. (Jan 2008). "Fibrillary glomerulonephritis and immunotactoid glomerulopathy.". J Am Soc Nephrol 19 (1): 34-7. doi:10.1681/ASN.2007070757. PMID 18045849.
- ↑ Cite error: Invalid
<ref>tag; no text was provided for refs namedfondazionedamico - ↑ Kleinschmidt-DeMasters BK, Prayson RA (November 2006). "An algorithmic approach to the brain biopsy--part I". Arch. Pathol. Lab. Med. 130 (11): 1630–8. PMID 17076524.
- ↑ 6.0 6.1 6.2 6.3 6.4 Ebert EC, Nagar M (March 2008). "Gastrointestinal manifestations of amyloidosis". Am. J. Gastroenterol. 103 (3): 776-87. doi:10.1111/j.1572-0241.2007.01669.x. PMID 18076735.
- ↑ 7.0 7.1 7.2 Devata, S.; Hari, P.; Markelova, N.; Li, R.; Komorowski, R.; Shidham, VB. (2011). "Detection of amyloid in abdominal fat pad aspirates in early amyloidosis: Role of electron microscopy and Congo red stained cell block sections.". Cytojournal 8: 11. doi:10.4103/1742-6413.82278. PMID 21760829.
- ↑ 8.0 8.1 Nishi S, Alchi B, Imai N, Gejyo F (April 2008). "New advances in renal amyloidosis". Clin. Exp. Nephrol. 12 (2): 93-101. doi:10.1007/s10157-007-0008-3. PMID 18175051.
- ↑ Pomerance, A.; Slavin, G.; McWatt, J. (Jan 1976). "Experience with the sodium sulphate-Alcian Blue stain for amyloid in cardiac pathology.". J Clin Pathol 29 (1): 22-6. PMID 55419.
- ↑ 10.0 10.1 10.2 10.3 10.4 10.5 Amyloidosis. Merck Manual. URL: http://www.merck.com/mmpe/sec12/ch160/ch160a.html. Accessed on: 3 December 2009.
- ↑ Cotran, Ramzi S.; Kumar, Vinay; Fausto, Nelson; Nelso Fausto; Robbins, Stanley L.; Abbas, Abul K. (2005). Robbins and Cotran pathologic basis of disease (7th ed.). St. Louis, Mo: Elsevier Saunders. pp. 261. ISBN 0-7216-0187-1.
- ↑ Cotran, Ramzi S.; Kumar, Vinay; Fausto, Nelson; Nelso Fausto; Robbins, Stanley L.; Abbas, Abul K. (2005). Robbins and Cotran pathologic basis of disease (7th ed.). St. Louis, Mo: Elsevier Saunders. pp. 261. ISBN 0-7216-0187-1.
- ↑ Cotran, Ramzi S.; Kumar, Vinay; Fausto, Nelson; Nelso Fausto; Robbins, Stanley L.; Abbas, Abul K. (2005). Robbins and Cotran pathologic basis of disease (7th ed.). St. Louis, Mo: Elsevier Saunders. pp. 260. ISBN 0-7216-0187-1.
- ↑ URL: http://www.umm.edu/altmed/articles/amyloidosis-000007.htm. Accessed on: 23 October 2010.
- ↑ URL: http://library.med.utah.edu/WebPath/EXAM/IMGQUIZ/enfrm.html. Accessed on: 6 December 2010.
- ↑ Comenzo, RL.; Vosburgh, E.; Falk, RH.; Sanchorawala, V.; Reisinger, J.; Dubrey, S.; Dember, LM.; Berk, JL. et al. (May 1998). "Dose-intensive melphalan with blood stem-cell support for the treatment of AL (amyloid light-chain) amyloidosis: survival and responses in 25 patients.". Blood 91 (10): 3662-70. PMID 9573002.
- ↑ Cotran, Ramzi S.; Kumar, Vinay; Fausto, Nelson; Nelso Fausto; Robbins, Stanley L.; Abbas, Abul K. (2005). Robbins and Cotran pathologic basis of disease (7th ed.). St. Louis, Mo: Elsevier Saunders. pp. 261. ISBN 0-7216-0187-1.
- ↑ Cotran, Ramzi S.; Kumar, Vinay; Fausto, Nelson; Nelso Fausto; Robbins, Stanley L.; Abbas, Abul K. (2005). Robbins and Cotran pathologic basis of disease (7th ed.). St. Louis, Mo: Elsevier Saunders. pp. 259. ISBN 0-7216-0187-1.
- ↑ Cotran, Ramzi S.; Kumar, Vinay; Fausto, Nelson; Nelso Fausto; Robbins, Stanley L.; Abbas, Abul K. (2005). Robbins and Cotran pathologic basis of disease (7th ed.). St. Louis, Mo: Elsevier Saunders. pp. 259. ISBN 0-7216-0187-1.
- ↑ van Rijswijk MH, van Heusden CW (October 1979). "The potassium permanganate method. A reliable method for differentiating amyloid AA from other forms of amyloid in routine laboratory practice". Am. J. Pathol. 97 (1): 43–58. PMC 2042379. PMID 495695. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2042379/.
- ↑ Picken, MM. (Apr 2010). "Amyloidosis-where are we now and where are we heading?". Arch Pathol Lab Med 134 (4): 545-51. doi:10.1043/1543-2165-134.4.545. PMID 20367306.
- ↑ Röcken C (December 2009). "[Update on immunohistological classification of amyloidoses]" (in German). Pathologe 30 Suppl 2: 121–3. doi:10.1007/s00292-009-1183-7. PMID 19756621.
- ↑ Solomon, A.; Murphy, CL.; Westermark, P. (Jan 2008). "Unreliability of immunohistochemistry for typing amyloid deposits.". Arch Pathol Lab Med 132 (1): 14; author reply 14-5. doi:10.1043/1543-2165(2008)132[14b:IR]2.0.CO;2. PMID 18181665. http://www.archivesofpathology.org/doi/pdf/10.1043/1543-2165%282008%29132%5B14b%3AIR%5D2.0.CO%3B2.
- ↑ 24.0 24.1 Murphy CL, Eulitz M, Hrncic R, et al. (July 2001). "Chemical typing of amyloid protein contained in formalin-fixed paraffin-embedded biopsy specimens". Am. J. Clin. Pathol. 116 (1): 135–42. doi:10.1309/TWBM-8L4E-VK22-FRH5. PMID 11447744.
- ↑ Chee, CE.; Lacy, MQ.; Dogan, A.; Zeldenrust, SR.; Gertz, MA. (Jun 2010). "Pitfalls in the diagnosis of primary amyloidosis.". Clin Lymphoma Myeloma Leuk 10 (3): 177-80. doi:10.3816/CLML.2010.n.027. PMID 20511161.
- ↑ Murphy CL, Wang S, Williams T, Weiss DT, Solomon A (2006). "Characterization of systemic amyloid deposits by mass spectrometry". Meth. Enzymol. 412: 48–62. doi:10.1016/S0076-6879(06)12004-2. PMID 17046651.
- ↑ 27.0 27.1 Vrana JA, Gamez JD, Madden BJ, Theis JD, Bergen HR, Dogan A (December 2009). "Classification of amyloidosis by laser microdissection and mass spectrometry-based proteomic analysis in clinical biopsy specimens". Blood 114 (24): 4957–9. doi:10.1182/blood-2009-07-230722. PMID 19797517.
- ↑ Cotran, Ramzi S.; Kumar, Vinay; Fausto, Nelson; Nelso Fausto; Robbins, Stanley L.; Abbas, Abul K. (2005). Robbins and Cotran pathologic basis of disease (7th ed.). St. Louis, Mo: Elsevier Saunders. pp. 260. ISBN 0-7216-0187-1.
- ↑ 29.0 29.1 Ikeda, S. (Dec 2004). "Cardiac amyloidosis: heterogenous pathogenic backgrounds.". Intern Med 43 (12): 1107-14. PMID 15645642.
- ↑ 30.0 30.1 30.2 Sharma, PP.; Payvar, S.; Litovsky, SH.. "Histomorphometric analysis of intramyocardial vessels in primary and senile amyloidosis: epicardium versus endocardium.". Cardiovasc Pathol 17 (2): 65-71. doi:10.1016/j.carpath.2007.05.008. PMID 18329550.
- ↑ Adams, D.; Koike, H.; Slama, M.; Coelho, T. (Jul 2019). "Hereditary transthyretin amyloidosis: a model of medical progress for a fatal disease.". Nat Rev Neurol 15 (7): 387-404. doi:10.1038/s41582-019-0210-4. PMID 31209302.
- ↑ Pomerance, A. (Sep 1965). "Senile cardiac amyloidosis.". Br Heart J 27 (5): 711-8. PMID 5829755. http://www.ncbi.nlm.nih.gov/pmc/articles/PMC469777/pdf/brheartj00340-0085.pdf.
- ↑ Cardiac amyloidosis. Medlineplus.org. URL: http://www.nlm.nih.gov/medlineplus/ency/article/000193.htm. Accessed on: 3 December 2009.
- ↑ Satoskar, AA.; Burdge, K.; Cowden, DJ.; Nadasdy, GM.; Hebert, LA.; Nadasdy, T. (Jun 2007). "Typing of amyloidosis in renal biopsies: diagnostic pitfalls.". Arch Pathol Lab Med 131 (6): 917-22. doi:10.1043/1543-2165(2007)131[917:TOAIRB]2.0.CO;2. PMID 17550319. http://www.archivesofpathology.org/doi/full/10.1043/1543-2165(2007)131%5B917:TOAIRB%5D2.0.CO;2.
- ↑ Petruzziello, F.; Zeppa, P.; Catalano, L.; Cozzolino, I.; Gargiulo, G.; Musto, P.; D'Auria, F.; Liso, V. et al. (May 2010). "Amyloid in bone marrow smears of patients affected by multiple myeloma.". Ann Hematol 89 (5): 469-74. doi:10.1007/s00277-009-0857-9. PMID 19894050.
- ↑ Alabi, ZO.; Ojo, OS.; Odesanmi, WO. (1991). "Secondary amyloidosis in chronic osteomyelitis.". Int Orthop 15 (1): 21-2. PMID 2071276.
- ↑ Miossec, P.; Lormeau, B.; Valensi, P.; Arthuis, F.; Amouroux, J.; Attali, JR. (Sep 1999). "Bone amyloidoma in a diabetic patient with morbid obesity.". Diabetes Metab 25 (3): 261-3. PMID 10499196.
External links
- Amyloidosis - wikipedia.org.