Difference between revisions of "Prostate cancer grading"
Jump to navigation
Jump to search
| Line 1: | Line 1: | ||
This article deals with '''prostate cancer grading'''. It covers the '''Gleason System''' and the proposed '''Contemporary Prostate Cancer Grading System'''. | This article deals with '''prostate cancer grading'''. | ||
It covers the '''Gleason System''' and the proposed '''Contemporary Prostate Cancer Grading System'''. | |||
==Gleason grading system== | ==Gleason grading system== | ||
*[[AKA]] ''modified Gleason grading system''. | *[[AKA]] ''modified Gleason grading system''. | ||
**It is could be called the ''modified modified Gleason grading system'', as it has be tweaked twice. | |||
===Overview=== | ===Overview=== | ||
Revision as of 07:30, 30 December 2015
This article deals with prostate cancer grading.
It covers the Gleason System and the proposed Contemporary Prostate Cancer Grading System.
Gleason grading system
- AKA modified Gleason grading system.
- It is could be called the modified modified Gleason grading system, as it has be tweaked twice.
Overview
- There is consensus on how it is done.[1]
- Score range: 6-10.
- Technically 2-10... but almost no one uses 2-5.
- Reported on biopsy (and TURP) as: (primary pattern) + (highest non-primary pattern) = sum.
- Gleason score 3+4=7 means: pattern 3 is present and dominant, pattern 4 is the remainder of the tumour - but present in a lesser amount than pattern 3.
- Gleason score 4+5=9 means: pattern 4 is present and dominant, pattern 5 is present in a lesser amount that pattern 4. Pattern 3 may be present in a quantity less than pattern 4 or is absent.
- Reported as on prostatectomies as: (primary pattern) + (secondary pattern) = sum, (tertiary pattern)
- Tertiary Gleason pattern - definition: a pattern that is seen in less than 5% of the tumour (volume), that is higher grade than the two dominant patterns.[2]
- The presence of a tertiary patterns adversely affect the prognosis; however, the prognosis is not as bad as when the tertiary pattern is the secondary pattern, i.e. 3+4 tertiary 5 has a better prognosis than 3+5 (with some small amount of pattern 4).[2]
Examples
- A biopsy with 80% pattern 4, 16% pattern 3 and 4% pattern 5... would be reported as: 4+5=9.
- A biopsy with 92% pattern 4, and 8% pattern 3... would be reported as: 4+3=7.
- A biopsy with 98% pattern 4, and 2% pattern 3... would be reported as: 4+4=8.
- A prostatectomy with 80% pattern 4, 16% pattern 3 and 4% pattern 5... would be reported as: 4+3=7 with tertiary pattern 5.
Gleason patterns (modified)
Gleason pattern 1 & 2
- Use strongly discouraged by a number of GU pathology experts.
Notes:
- Gleason pattern 1 - probably represents what today would be called adenosis.
- Should never be used.
- Gleason pattern 2 - used by few GU pathology experts occasionally.
- Generally, should not be diagnosed on core biopsies.[3]
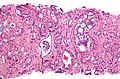
Gleason pattern 3
- Glands smaller than normal prostate glands + loss of epithelial folding.
- Can draw a line around each gland.
- May have gland branching.
- Glands have a X, U, V or Y shape.
Notes:
- Gland lumina should be seen.
- All cribriform is now, generally, classified as Gleason pattern 4.[3]
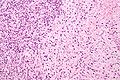
Gleason pattern 4
- Loss of gland lumina.
- Gland fusion.
- Benign looking cords ('hypernephroid pattern').
- Cribriform.
- Glomeruloid pattern - resembles a glomerulus.
Notes:
- One gland is not enough to call Gleason 4.
Images
www:
Gleason pattern 5
- Sheets.
- Must be differentiated from intraductal growth (which like in the breast are well circumscribed nests).
- Single cells.
- May be confused with stromal/lymphocytic infiltration.
- Look for nucleoli, cells should be round (prostatic stroma cells are spindle cells).
- May be confused with stromal/lymphocytic infiltration.
- Cords (strands).
- Line of cells.
- Should not be intermixed with clumps of cells (pattern 4).
- Nests of cells with necrosis (at the centre) (comedonecrosis) or (intraluminal) necrosis in a cribriform pattern.[1]
- Necrosis:
- Nuclear changes:
- Karyorrhexis (nuclear fragmentation).
- Pynosis (nuclear shrinkage).
- Karyolysis (nuclear dissolution).
- Cell ghosts (cells without a nucleus).
- Nuclear changes:
- Necrosis:
Notes:
- Pattern 5 may be under-diagnosed.
- Single cells is the most commonly missed pattern.[4]
Images
www:
Gleason pattern for special types
Special types of prostate cancer have suggested Gleason patterns:[5]
| Special type | Gleason pattern | Comment |
|---|---|---|
| Ductal carcinoma | 4 | may be graded 3 or 5[6] |
| Mucinous carcinoma | 3 or 4 - dependent on morphology[7][8] | some advocate grade 4[5] |
| Sarcomatoid carcinoma | 5 | glands graded separately |
| Signet ring cell carcinoma | 5 | |
| Small cell carcinoma | not graded (ISUP 2005 consensus[1]) | may be graded 5[6] |
| Adenosquamous and squamous carcinoma | not graded | |
| Lymphoepithelioma-like carcinoma | not graded | |
| Adenoid cystic carcinoma | not graded | |
| Urothelial carcinoma | not graded | |
| Undifferentiated carcinoma, NOS | not graded |
How to remember the ones that aren't graded - think of Ur Lung carcinomas (Urothelial carcinoma, Lymphoepithelioma-like carcinoma):
- Small cell carcinoma.
- Squamous cell carcinoma.
- Adenosquamous carcinoma.
- Adenoid cystic carcinoma.
Biopsy-prostatectomy concordance of Gleason score
- Discordance is common.
- Upgrade on prostatectomy: 25-40%.
- Downgrade on prostatectomy: 5-15%.
Selected studies on concordance:
| Study | Upgrade | Downgrade | Notes |
|---|---|---|---|
| Sfoungaristos et al.[9] | 42.1% | 13.7% | high volume of tumour predicts upgrade |
| Thomas et al.[10] | 38.1% | 4.7% | |
| Truesdale et al.[11] | 23% | 11% |
Sign out
Upgrading
Gleason score upgrading on prostatectomy is considered relatively common; it is reported to occur in 23% to 42.1% of cases.[1][2] 1. BJU Int. 2011 107 (5): 749-54. 2. Can Urol Assoc J. 2012 Jan 24:1-5.
Downgrading
Gleason score downgrading on prostatectomy is considered uncommon; however, it is reported in 4.7% to 13.7% of cases.[1][2] 1. BJU Int. 2012 Jan; 109(2):214-9. 2. Can Urol Assoc J. 2012 Jan; 24;1-5.
Order of Gleason score components changed
COMMENT: The change in the order of the Gleason score components (3+4 on prostatectomy versus 4+3 on core biopsy) may be explained by sampling.
Grade groupings
Proposed new system and old (modified) Gleason score:[12][13]
| Prognostic group | Gleason score |
|---|---|
| I | 3+3 |
| II | 3+4 |
| III | 4+3 |
| IV | 8 (4+4, 3+5, 5+3) |
| V | 9 or 10 (4+5, 5+4, 5+5) |
Rationale:
- Patients won't be told they have a 6 out of 10 cancer, and then think it is an intermediate grade cancer that is worrisome. Instead, they will be told they have a 1 out of 5 cancer.[12]
See also
References
- ↑ 1.0 1.1 1.2 Epstein, JI.; Allsbrook, WC.; Amin, MB.; Egevad, LL. (Sep 2005). "The 2005 International Society of Urological Pathology (ISUP) Consensus Conference on Gleason Grading of Prostatic Carcinoma.". Am J Surg Pathol 29 (9): 1228-42. PMID 16096414.
- ↑ 2.0 2.1 Zhou, Ming; Magi-Galluzzi, Cristina (2006). Genitourinary Pathology: A Volume in Foundations in Diagnostic Pathology Series (1st ed.). Churchill Livingstone. pp. 72. ISBN 978-0443066771.
- ↑ 3.0 3.1 Epstein, JI. (Feb 2010). "An update of the Gleason grading system.". J Urol 183 (2): 433-40. doi:10.1016/j.juro.2009.10.046. PMID 20006878. Cite error: Invalid
<ref>tag; name "pmid20006878" defined multiple times with different content - ↑ Fajardo, DA.; Miyamoto, H.; Miller, JS.; Lee, TK.; Epstein, JI. (Nov 2011). "Identification of Gleason pattern 5 on prostatic needle core biopsy: frequency of underdiagnosis and relation to morphology.". Am J Surg Pathol 35 (11): 1706-11. doi:10.1097/PAS.0b013e318228571d. PMID 21997691.
- ↑ 5.0 5.1 Grignon DJ (March 2004). "Unusual subtypes of prostate cancer". Mod. Pathol. 17 (3): 316–27. doi:10.1038/modpathol.3800052. PMID 14976541.
- ↑ 6.0 6.1 URL: https://www.bostwicklaboratories.com/global/physicians/medical-library/articles/gleason-grading.aspx. Accessed on: 26 November 2011.
- ↑ Osunkoya, AO.; Adsay, NV.; Cohen, C.; Epstein, JI.; Smith, SL. (Jul 2008). "MUC2 expression in primary mucinous and nonmucinous adenocarcinoma of the prostate: an analysis of 50 cases on radical prostatectomy.". Mod Pathol 21 (7): 789-94. doi:10.1038/modpathol.2008.47. PMID 18487999.
- ↑ Osunkoya, AO.; Nielsen, ME.; Epstein, JI. (Mar 2008). "Prognosis of mucinous adenocarcinoma of the prostate treated by radical prostatectomy: a study of 47 cases.". Am J Surg Pathol 32 (3): 468-72. doi:10.1097/PAS.0b013e3181589f72. PMID 18300802.
- ↑ Sfoungaristos, S.; Perimenis, P. (Jan 2012). "Clinical and pathological variables that predict changes in tumour grade after radical prostatectomy in patients with prostate cancer.". Can Urol Assoc J: 1-5. doi:10.5489/cuaj.11067. PMID 22277633.
- ↑ Thomas, C.; Pfirrmann, K.; Pieles, F.; Bogumil, A.; Gillitzer, R.; Wiesner, C.; Thüroff, JW.; Melchior, SW. (Jan 2012). "Predictors for clinically relevant Gleason score upgrade in patients undergoing radical prostatectomy.". BJU Int 109 (2): 214-9. doi:10.1111/j.1464-410X.2011.10187.x. PMID 21592293.
- ↑ Truesdale, MD.; Cheetham, PJ.; Turk, AT.; Sartori, S.; Hruby, GW.; Dinneen, EP.; Benson, MC.; Badani, KK. (Mar 2011). "Gleason score concordance on biopsy-confirmed prostate cancer: is pathological re-evaluation necessary prior to radical prostatectomy?". BJU Int 107 (5): 749-54. doi:10.1111/j.1464-410X.2010.09570.x. PMID 20840549.
- ↑ 12.0 12.1 URL: http://urology.jhu.edu/newsletter/2014/prostate_cancer_2014_19.php. Accessed on: 28 March 2015.
- ↑ Epstein, JI.; Zelefsky, MJ.; Sjoberg, DD.; Nelson, JB.; Egevad, L.; Magi-Galluzzi, C.; Vickers, AJ.; Parwani, AV. et al. (Jul 2015). "A Contemporary Prostate Cancer Grading System: A Validated Alternative to the Gleason Score.". Eur Urol. doi:10.1016/j.eururo.2015.06.046. PMID 26166626.