Difference between revisions of "Radiation changes"
Jump to navigation
Jump to search
| Line 26: | Line 26: | ||
| Prognosis = benign | | Prognosis = benign | ||
| Other = | | Other = | ||
| ClinDDx = | | ClinDDx = cancer recurrence, infection, new malignancy, post-surgical changes | ||
}} | }} | ||
'''Radiation changes''', also '''radiation effect''', are seen occasionally by [[pathologist]]s. They are usually a result of prior (radiation) treatments. The history is important in making this diagnosis | '''Radiation changes''', also '''radiation effect''', are seen occasionally by [[pathologist]]s. They are usually a result of prior (radiation) treatments. The history is important in making this diagnosis | ||
==General== | |||
*History of radiation treatment/exposure. | |||
*Clinical symptoms dependent on site. | |||
==Gross== | ==Gross== | ||
Revision as of 21:00, 19 March 2015
| Radiation changes | |
|---|---|
| Diagnosis in short | |
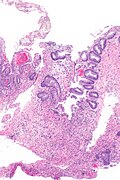
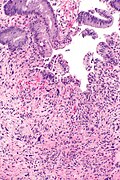
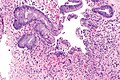
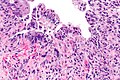
 Radiation changes. H&E stain. | |
|
| |
| LM | cytoplasmic vacuolation (usually abundant), enlarged nuclei - but usu. normal NC ratio, no nuclear membrane irregularies, chromatin "smudgy", +/-multinucleation, +/-fibrosis (chronic change), +/-edema (acute change) |
| LM DDx | pleomorphic tumours - esp. sarcomas, poorly differentiated carcinomas, drug/toxin effect |
| IHC | Ki-67 low, pankeratin -ve (usu.) |
| Site | pretty much anywhere |
|
| |
| Clinical history | history of radiation treatment/exposure - important for the diagnosis |
| Prognosis | benign |
| Clin. DDx | cancer recurrence, infection, new malignancy, post-surgical changes |
Radiation changes, also radiation effect, are seen occasionally by pathologists. They are usually a result of prior (radiation) treatments. The history is important in making this diagnosis
General
- History of radiation treatment/exposure.
- Clinical symptoms dependent on site.
Gross
- +/-Erythema (early)
- +/-Fibrotic appearing tissue (late).
Microscopic
Features:[1]
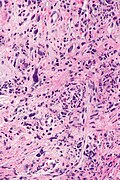
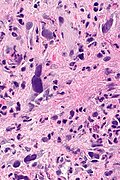
- Cytoplasmic vacuolation - usually abundant.
- Nucleus:
- Enlarged nucleus - but normal NC ratio.
- No nuclear membrane irregularies.
- Chromatin: "smudgy".
- +/-Multinucleation.
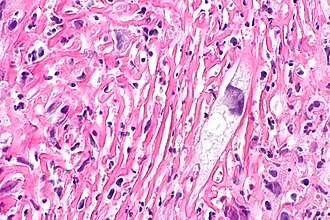
- +/-Fibrosis (chronic change).
- +/-Edema (acute change).
Important note:
- The atypical cells are stromal cells; these survive the radiation. The epithelium is usually normal in the context of chronic changes.
- Pleomorphism is often suggestive of malignancy. Paradoxically, in the context of radiation, less pleomorphic (clonal-appearing) cells may be malignant!
DDx:
Images
Radiation proctitis - low mag. (WC)
IHC
- Pankeratin -ve.
- KI-67 low.
Sign out
RECTUM, BIOPSY: - SQUAMOUS MUCOSA WITH MARKED ACUTE INFLAMMATION AND REACTIVE CHANGES. - GRANULATION TISSUE. - LARGE ATYPICAL STROMAL CELLS AND FIBROSIS, COMPATIBLE WITH THE HISTORY OF RADIATION TREATMENT. - NEGATIVE FOR DYSPLASIA AND NEGATIVE FOR MALIGNANCY.
URINARY BLADDER, TRIGONE, BIOPSY: - INFLAMED UROTHELIAL MUCOSA WITH SQUAMOUS METAPLASIA, ULCERATION AND GRANULATION TISSUE FORMATION. - RADIATION CHANGES (STROMA). - NEGATIVE FOR DYSPLASIA AND NEGATIVE FOR MALIGNANCY.
Urinary bladder, biopsy: - Urothelial mucosa with evidence of ulceration (fibrin, necroinflammatory debris), mild stromal atypia and chronic inflammation, compatible with radiation cystitis - Negative for dysplasia - Negative for malignancy
Micro
Scattered rare large atypical cells with a preserved nucleus-to-cytoplasm ratio are present. Fibrosis is present.
See also
- Radiation colitis.
- Radiation changes in cervical cytology.
- Radiation changes of the endocervical epithelium.
- Radiation oncology.