Difference between revisions of "Giant cell arteritis"
Jump to navigation
Jump to search
| Line 46: | Line 46: | ||
Treatment: | Treatment: | ||
*Treat right away with high dose steroids. | *Treat right away with high dose steroids. | ||
**Biopsy is confirmatory. | **Biopsy is confirmatory and is still diagnostic if done <7-10 days after treatment starts.<ref name=pmid7921300>{{Cite journal | last1 = Weinberg | first1 = DA. | last2 = Savino | first2 = PJ. | last3 = Sergott | first3 = RC. | last4 = Bosley | first4 = TM. | title = Giant cell arteritis. Corticosteroids, temporal artery biopsy, and blindness. | journal = Arch Fam Med | volume = 3 | issue = 7 | pages = 623-7 | month = Jul | year = 1994 | doi = | PMID = 7921300 }}</ref> | ||
==Microscopic== | ==Microscopic== | ||
Revision as of 18:59, 17 December 2015
| Giant cell arteritis | |
|---|---|
| Diagnosis in short | |
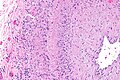
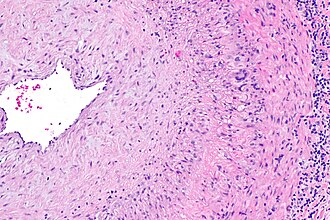 Giant cell arteritis. H&E stain. | |
|
| |
| Synonyms | temporal arteritis |
|
| |
| LM | large artery with intramural inflammatory cells (often granulomatous); intimal thickening; frank destruction of arterial wall common - fibrinoid necrosis |
| Site | large blood vessels - see vasculitides |
|
| |
| Clinical history | typically older than 50 years |
| Signs | loss of vision, weight loss, chills, fever |
| Symptoms | jaw claudication (classic), headache (classic), double vision, scalp tenderness |
| Prevalence | uncommon |
| Blood work | ESR elevated |
| Prognosis | good if treated |
| Clin. DDx | other causes of headache |
| Treatment | steroids |
Giant cell arteritis (abbreviated GCA), also known as temporal arteritis, is a type of large vessel vasculitis.
General
- Classically afflicts the temporal artery.
Clinical features:
- Classic finding: jaw claudication, typically in a patient older than 50 years.
- Other findings: headache (very common),[1] vision loss or diplopia, scalp tenderness, polymyalgia, weight loss, chills, fever.
Work-up:
- CRP, ESR, temporal artery biopsy.
- ESR normal (>50 years old): <20 mm/hr males, <30 mm/hr females.[2]
Treatment:
- Treat right away with high dose steroids.
- Biopsy is confirmatory and is still diagnostic if done <7-10 days after treatment starts.[3]
Microscopic
Features - as per Le et al.:[1]
- Artery with intimal thickening.
- Transmural inflammatory cells.
- Giant cells.
Notes:
- Inflammation classically granulomatous.
- Granulomas not required for the diagnosis!
- Often accompanied by frank destruction of the arterial wall, e.g. fibrinoid necrosis (pink anucleate arterial wall).
Images
www:
Sign out
Negative
TEMPORAL ARTERY, LEFT, BIOPSY: - MEDIUM SIZE ARTERY WITHOUT PATHOLOGIC DIAGNOSIS, SEE COMMENT. COMMENT: A negative biopsy does not rule out the possibility of giant cell (temporal) arteritis, as this may be a focal disorder. The clinical management is dependent upon the clinical impression.
See also
References
- ↑ 1.0 1.1 Le, K.; Bools, LM.; Lynn, AB.; Clancy, TV.; Hooks, WB.; Hope, WW. (Oct 2014). "The effect of temporal artery biopsy on the treatment of temporal arteritis.". Am J Surg. doi:10.1016/j.amjsurg.2014.07.007. PMID 25457237.
- ↑ URL: http://www.nlm.nih.gov/medlineplus/ency/article/003638.htm. Accessed on: 17 August 2012.
- ↑ Weinberg, DA.; Savino, PJ.; Sergott, RC.; Bosley, TM. (Jul 1994). "Giant cell arteritis. Corticosteroids, temporal artery biopsy, and blindness.". Arch Fam Med 3 (7): 623-7. PMID 7921300.