Difference between revisions of "Dermatologic neoplasms"
m (→Invasive SCC) |
m (→Invasive SCC) |
||
| Line 89: | Line 89: | ||
-- TUMOUR GREATEST DIMENSION: ___ CM. | -- TUMOUR GREATEST DIMENSION: ___ CM. | ||
-- TUMOUR THICKNESS: ___ MM. | -- TUMOUR THICKNESS: ___ MM. | ||
-- LATERAL MARGINS: | -- LATERAL MARGINS: NEGATIVE FOR IN SITU CARCINOMA AND INVASIVE CARCINOMA. | ||
-- DEEP MARGIN: | -- DEEP MARGIN: NEGATIVE FOR INVASIVE CARCINOMA. | ||
-- NEAREST MARGIN: 1 MM, LATERAL MARGIN. | |||
-- NEGATIVE FOR LYMPHOVASCULAR INVASION. | -- NEGATIVE FOR LYMPHOVASCULAR INVASION. | ||
-- NEGATIVE FOR PERINEURAL INVASION. | -- NEGATIVE FOR PERINEURAL INVASION. | ||
Revision as of 08:01, 28 August 2013
This article deals with dermatologic neoplasms. It includes dermatologic cancer, which can be deadly. Collectively, dermatologic cancers are the most common form of cancer.
An introduction to dermatopathy is found in the dermatopathology article. Non-malignant disease is covered in the non-malignant skin disease article.
The Big Three malignant
Basal cell carcinoma
Squamous cell carcinoma of the skin
- Abbreviated skin SCC, SCC of the skin, and SCC of skin.
General
Precursor:[1]
- Actinic keratosis (solar keratosis).
- Clinical: yellow-brown scaly, patches, sandpaper sensation.
Risk factors:[1]
- Sun exposure.
- Immune suppression (e.g. organ transplant recipients).
Notes:
- Keratoacanthoma.
- Some don't believe this entity exists.
- These people sign this entity as low grade squamous cell carcinoma, keratoacanthoma type.[2]
- Some don't believe this entity exists.
Microscopic
High risk features - for SCC of the skin:[3]
- Primary site is ear or lip.†
- Clark level IV/V = reticular dermis or deeper.
- >=2 mm thickness -- measured from granular layer (stratum granulosum) or ulcer base to deepest aspect.
- Lymphovascular invasion.
- Perineural invasion.
- Poorly differentiated.
Note:
- † The words used are "hair-bearing lip" - but there is considerable confusion about this as the AJCC manual contradicts itself.[4]
DDx:
- Inverted follicular keratosis.
- Bowen disease.
- Malignant melanoma.
- Paget disease of the breast.
- Eccrine carcinoma
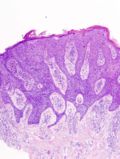
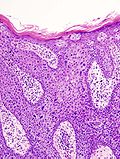
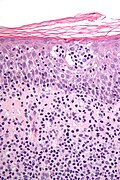
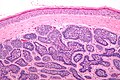
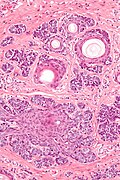
Bowen disease
Bowen disease is squamous cell carcinoma in situ of the skin.
- Its histomorphologic appearance may be similar to Paget disease of the breast/Extramammary Paget disease, Toker cell hyperplasia and melanoma.
- IHC is used to separate the entities definitively.
Histologic DDx of Bowen disease:
- Benign Toker cell hyperplasia.
- Malignant melanoma.
- Paget disease of the breast.
- Eccrine carcinoma.
Images
IHC
Bowen's disease panel:
- CK5/6 +ve.[5]
- Usu. -ve in Paget disease of the breast/Extramammary Paget disease.
- S100 -ve, HMB-45 -ve.
- Both typically +ve in melanoma.
- CEA -ve[6] (+ve in Paget disease of the breast/Extramammary Paget disease, -ve in Toker cells).
- CK7 -ve.
- Toker cells CK7 +ve.[7]
Sign-out
Invasive SCC
SKIN, SITE, BIOPSY: - MODERATELY-DIFFERENTIATED INVASIVE SQUAMOUS CELL CARCINOMA, SEE COMMENT. - NEGATIVE FOR LYMPHOVASCULAR INVASION. - NEGATIVE FOR PERINEURAL INVASION. COMMENT: The nearest margin (lateral margin) is 1 mm. The tumour is 9 mm in maximal dimension.
SKIN LESION, SITE, EXCISION: - INVASIVE SQUAMOUS CELL CARCINOMA, MODERATELY-DIFFERENTIATED. -- TUMOUR GREATEST DIMENSION: ___ CM. -- TUMOUR THICKNESS: ___ MM. -- LATERAL MARGINS: NEGATIVE FOR IN SITU CARCINOMA AND INVASIVE CARCINOMA. -- DEEP MARGIN: NEGATIVE FOR INVASIVE CARCINOMA. -- NEAREST MARGIN: 1 MM, LATERAL MARGIN. -- NEGATIVE FOR LYMPHOVASCULAR INVASION. -- NEGATIVE FOR PERINEURAL INVASION. - EXTENSIVE SOLAR ELASTOSIS.
SKIN, SITE, BIOPSY: - INVASIVE SQUAMOUS CELL CARCINOMA, SEE TUMOUR SUMMARY. TUMOUR SUMMARY: Histologic type: squamous cell carcinoma, type not otherwise specified. Histologic grade: moderately differentiated. Greatest dimension: ___ cm. Tumour thickness: ___ mm. Peripheral margin: negative for invasive carcinoma and in situ carcinoma. Deep margin (invasive component): negative for invasive carcinoma. Closest margin: deep margin, ___ mm. Lymphovascular invasion: not identified. Perineural invasion: not identified.
Bowen's disease
SKIN LESION, RIGHT EAR, BIOPSY: - SQUAMOUS CELL CARCINOMA IN SITU (BOWEN'S DISEASE), INCOMPLETELY EXCISED. COMMENT: Complete excision of the lesion is recommended.
Melanoma
General
- Known as the great mimicker in pathology; it may look like many things.
Microscopic
Features:
- Classic appearance of melanoma:
- Loosely cohesive; mix of small nests of cells, single cells.
- Usu. mixed of spindle and ovoid cell morphology.
- +/-Occasional large binucleated cells.
- +/-Cytoplasm: brown pigment (melanin).
- +/-Prominent (large) red nucleoli (like in serous carcinoma of the ovary).
- Often marked nuclear pleomorphism - variation in cell size, shape & staining (like in serous carcinoma of the ovary).
- Nuclear pseudoinclusions (like in papillary thyroid carcinoma).
Less common malignant
Dermatofibrosarcoma protuberans
- Abbreviated DFSP.
General
- Dermal location.
- Destroys adnexal structures.
- Occasionally transforms to a (more aggressive) fibrosarcoma.[8]
Treatment:[9]
- Wide excision.
- May include imatinib (Gleevec).
Gross
Features:[10]
- Firm plaque, often bosselated, usually on the trunk.
- +/-Ulceration.
Images:
- Protuberant DFSP (dermatlas.med.jhmi.edu).
- Huge DFSP on back (dermatlas.med.jhmi.edu).
- Protuberant DFSP - gross and histology (dermatlas.med.jhmi.edu).
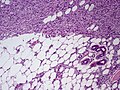
Microscopic
Features:[9]
- Dermal spindle cell lesion with storiform pattern.
- Spokes of the wheel-pattern.
- Contains adipose tissue within the tumour -- key feature.
- Described as "honeycomb pattern" and "Swiss cheese pattern".
Notes:
- Adnexal structure within tumour are preserved -- this is unusual for a malignant tumour -- important.
DDx:
- Dermatofibroma - main DDx - has entrapment of collagen bundles at the edge of the lesion.
- Dermatomyofibroma.[11]
DDx of storiform pattern:
- DFSP.
- Dermatofibroma.
- Solitary fibrous tumour.
- Undifferentiated pleomorphic sarcoma.
Images
www:
IHC
Panel:[12]
- CD34 +ve.
- Factor XIIIa -ve.
- S100 -ve (screen for melanoma).
- Caldesmin -ve (screen for muscle differentiation).
- Beta-catenin. (???)
- MIB1 (proliferation marker).
- Should not be confused with MIB-1 a gene that regulates apoptosis.
Molecular
A characteristic translocation is seen:[15] t(17;22)(q22;q15) COLA1/PDGFB.
Cutaneous B-cell lymphoma
- Abbreviated CBCL.
General
- CBCL is less common than cutaneous T-cell lymphoma (CTCL).[16]
Microscopic
Features:
- Dermal lymphoid infiltrate.
- "Grenz zone" - space between the epidermis and the dermal infiltrate - key feature.
IHC
- B cell and T cell markers.
Cutaneous T-cell lymphoma
- Abbreviated CTCL.
General
- Mycosis fungoides - is a subtype (???).
- CTCL is more common than cutaneous B-cell lymphoma (CBCL).[17][18]
Stages - like Kaposi sarcoma:
- Patch.
- Plaque.
- Nodular.
Microscopic
- Atypical lymphocytes:
- Have folded "cerebriform" nuclei; Sezary-Lutzner cells.[19]
- Grouping:
- Nests in the epidermis - known as "Pautrier microabscesses".
- Single lymphocytes in epidermis - without accompanying edema.
- Short linear arrays of lymphocytes along the basal layer of the epidermis; "epidermotropism".[19]
DDx:
Images
www:
IHC
Key stain:
- CD4 +ve.[20]
Other stains:
- CD3 +ve.
- CD8 -ve.
- CD20 -ve (to r/o significant B cell population).
- CD30 -ve.
- CD5 +ve.
- CD7 -ve (often lost first in T cell lymphomas).
- Ki-67 high.
- CD56 -ve.
Merkel cell carcinoma
Eccrine carcinoma
General
- Arises from the proximal sweat duct.
Microscopic
Features:
- Pleomorphic nuclei with nucleoli.
- Duct-like structures - key feature.
- Extends from dermis into epidermis (follows path of a benign sweat duct).
Notes:
- May resemble Extramammary Paget's disease/Paget's disease of the breast.
Kaposi sarcoma
- See Kaposi sarcoma.
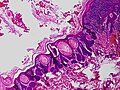
Sebaceous carcinoma
- AKA sebaceous cell carcinoma.
General
- Malignant.
- May arise in a salivary gland.[21]
- Can be part of Muir-Torre syndrome.
Notes:
- Sebaceous lesions (from benign to malignant): sebaceous hyperplasia, sebaceous adenoma, sebaceoma, sebaceous carcinoma.
Gross
Features:[22]
- Classically head and neck tumour.
- Yellow or red (ulcerated) nodule.
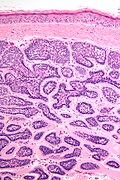
Microscopic
Features:[23]
- Sebaceous differentiation - may be a minor component - key feature.
- Sebocytes = abundant pale fluffy cytoplasm with vacuolization.
- Basaloid cells - often dominant.
- May lead to confusion with basaloid tumours.
- Nodular or diffuse growth pattern surrounded by a dense fibrous stroma.
- Infiltrative border - important.
- The key difference with sebaceous adenoma in cases where there isn't significant nuclear atypia.
- +/-Nuclear atypia.
- +/-Squamous differentiation.
- +/-Foreign body-type giant cells.
DDx:
- Sebaceous adenoma - non-infiltrative border.
- Squamous cell carcinoma, clear cell variant.
- Malignant melanoma.
- Extramammary Paget disease.
- Trichoblastoma.
- Basal cell carcinoma.
- Sweat gland carcinoma.
Images
www:
Grading
Three tier system:[23]
- Well-differentiated - sebocytes predominant.
- Moderately differentiated - sebocytes are easily recognized but a minor component.
- Poorly differentiated - sebocytes are rare.
IHC
Features:[23]
- CK7 +ve[24] - often weak.
- EMA +ve -- only sebaceous component.[25]
- CEA -ve.
- Positive in extramammary Paget disease, sweat duct tumours.
Images:
Sign out
SKIN LESION, NOSE, BIOPSY: - SEBACEOUS CARCINOMA, WELL-DIFFERENTIATED, COMPLETELY EXCISED IN THE PLANE OF SECTION. COMMENT: EMA staining marks the sebocytes. The lesion is negative for Ber-EP4. Sebaceous carcinoma may be seen in the context of Muir-Torre syndrome.
Micro
Well differentiated
The sections show well-circumscribed dermal nests of basaloid cells with peripheral palisading, surrounded by a dense fibrous stroma. The basaloid cells have distinct nucleoli. Focally, the basaloid nests contain small clusters of cells with abundant pale, vacuolated, fluffy-appearing cytoplasm (sebocytes). Mitotic activity is minimal.
There is no artefactual clefting between the stroma and basaloid cell nests. The epidermis matures to the surface and does not have basal atypia.
The lesion is completely excised in the plane of section.
Poor differentiated
The sections show well-circumscribed dermal nests of basaloid cells with peripheral palisading, surrounded by a dense fibrous stroma, that extend from the skin surface almost to the adipose tissue. The basaloid cells have moderate nuclear atypia with occasional monstrous cells. Mitotic activity is abundant and atypical mitoses are present. The nests contain rare cells with pale, fluffy-appearing cytoplasm, suggestive of sebocytes.
Microcystic adnexal carcinoma
General
- Low-grade tumour.
- Adults.
Microscopic
Features:[27]
- Small basaloid cells - often forming small cystic spaces - key feature.
- Very bland cytology.
- Fibrotic stroma.
DDx:
- Sclerosing basal cell carcinoma.
- Desmoplastic trichoepithelioma (DTE).[28]
- Infiltrative squamous cell carcinoma.
Image:
IHC
Features:[29]
- BerEP4 -ve.
- Positive in sclerosing basal cell carcinoma.
- CK15 -ve.
- Positive in DTE.
- Negative in sclerosing BCC.
Trichilemmal carcinoma
General
- Super rare.
- Not well-described.
Microscopic
Features:[30]
- Clear (glycogen-rich) cytoplasm in center of lesion.
- Peripheral palisading at edge of lesion - root sheath differentiation (hair follicle).
- Contiguous with hair follicle or assoc. with trichilemmoma.
DDx:
- Squamous cell carcinoma, clear cell variant.
- Basal cell carcinoma, clear cell variant.
- Trichilemmoma.
Lymphomatoid papulosis
General
- Rare.
- Benign behaviour.
Microscopic
Features:
- Dermal lymphocytosis.
- No epidermal lymphocytes.
- Focal nuclear atypia.
DDx:
IHC
- CD30 +ve.[31]
Rare malignant
Basosquamous carcinoma
- Should not be confused with basaloid squamous cell carcinoma (AKA squamous cell carcinoma, basaloid variant).
General
- Very rare.
- Largest case series, as of 2000, 35 cases.[32]
- May be considered an aggressive variant of basal cell carcinoma.[32]
- Aggressive behaviour.[33]
Microscopic
Features:
- Has features of both basal cell carcinoma and squamous cell carcinoma.[33]
- BCC component usually predominant.[34]
Note:
- Busam notes that there is disagreement about what defines this tumour;[35] however, he goes on the describe it as a collision tumour.[34]
DDx:
- Basaloid squamous cell carcinoma.
- Basal cell carcinoma with squamous differentiation.
Intermediate
Atypical fibroxanthoma
- Abbreviated AFX.
General
- Typically head & neck region.[36]
- Thought to be related to pleomorphic undifferentiated sarcoma;[37] some say it is the same thing.[38]
- Usually benign.
- May metastasize - case report-type of occurrence.[39]
Clinical:
- Rapid growth.
- Elderly.
- Good prognosis.[40]
Microscopic
Features:[41]
- Dermal lesion - key point.
- Marked nuclear atypia.
- Mitoses.
- Mulitnucleated cells.
- Foamy cytoplasm - key feature.
DDx:
- Melanoma.
- Pleomorphic undifferentiated sarcoma (MFH).
- Leiomyosarcoma.
- Sarcomatoid squamous carcinoma.
Notes:
- No Grenz zone. (???)
Image:
IHC
Features:[41]
- S100 -ve (done to r/o melanoma).
- 34betaE12 -ve.
- p63 -ve (done to exclude SCC)
- Scant staining not considered +ve.
- Desmin -ve (done to r/o leiomyosarcoma).
Benign
Syringoma
General
- Benign sweat duct tumour.
- Eccrine differentiation.
- Usually close to lower eyelid.[43]
Microscopic
Features:[44]
- Proliferation of benign ducts with lined by a bilayer (as in normal sweat ducts) with abnormal architecture:
- Tadpole like appearing ducts.
DDx:
- Syringomatous adenomas of nipple (AKA syringoma of the nipple).[45]
- Chondroid syringoma. (???)
Images:
Chondroid syringoma
- Used to be called mixed tumour of skin.[47]
General
- Mixed apocrine & eccrine tumour of skin, usually in the head & neck[47], especially nose and cheek.[48]
- May be in major and minor salivary glands.[48]
Microscopic
Features:
- Mix tumour with:[47]
- Epithelial component:
- Nests of cells with:
- Moderate dull eosinophilic cytoplasm.
- Round/ovoid nuclei with nucleoli.
- Nests of cells with:
- Mesenchymal component - key feature:
- Epithelial component:
Images:
Dermal cylindroma
General
- Benign skin lesion.
- Occasionally malignant.[50]
- Should not be confused with cylindroma (adenoid cystic carcinoma).
- May be related to eccrine spiradenoma.[51][52]
May be familial:[50]
- Familial cylindromatosis (autosomal dominant).
- Brook–Spiegler syndrome.
Gross
- Classically scalp - usually head and neck or face.
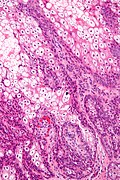
Microscopic
Features:[50]
- Nests of cells that fit together like a jigsaw puzzle - the borders of the nests are opposed and undulate.
- Basaloid cells with scant cytoplasm and dark nuclei palisade around the edge of the nests.
- Larger cells with moderate eosinophilic cytoplasm and lighter staining nuclei are at the centre of the nests.
- Cells nests surrounded by a band of hyaline (i.e. glassy, eosinophilic, acellular) material ~ 2X thickness of a basilar cell - key feature.
- This is basement membrane.
DDx:
Images
www:
Stains
- PAS +ve (basement membrane).[50]
Keratoacanthoma
Sebaceous adenoma
General
- Seen in Muir-Torre syndrome - a variant of Lynch syndrome (hereditary non-polyposis colon cancer).
Notes:
- Sebaceous lesions (from benign to malignant): sebaceous hyperplasia, sebaceous adenoma, sebaceoma, sebaceous carcinoma.
Microscopic
Features:
- Abnormal sebaceous glands (pale fluffy cytoplasm):
- Increased basal epithelium.
- Multiple dilated glands - opening to the surface.
Images
www:
Trichilemmoma
- May be spelled tricholemmoma.
General
- Benign neoplasm with features of the pilosebaceous follicular epithelium.[53]
- Associated with nevus sebaceous.[54]
- Muliple trichilemmomas associated with Cowden syndrome.[55]
Microscopic
Features:[55]
- Superficial dermal lesion contiguous with the epidermis:
- Core of lesion:
- Cuboidal cells with round nuclei, eosinophilic-clear cytoplasm.
- Periphery of lesion:
- Surrounded by hyaline band.
- Peripheral palisading.
- Core of lesion:
DDx:
Images:
- Trichilemmoma - low mag. (cancer.gov).[56]
- Trichilemmoma - high mag. (cancer.gov).[56]
- Trichilemmoma (jhmi.edu).[57]
- Trichilemmoma - low mag. (flickr.com/Irlam).
- Trichilemmoma - intermed. mag. (flickr.com/Irlam).
- Trichilemmoma - high mag. (flickr.com/Irlam).
Eccrine poroma
General
- Benign tumour arising from the distal sweat duct.
- Erythematous - gross.
Microscopic
Features:[58]
- Broad sheets of basaloid cells - attached to the epidermis - containing ductal structures - key feature.
- Biphasic stroma:
- Edematous stroma.
- Sclerotic stroma.
- Moderate nuclear pleomorphism.
- +/-Occasional mitoses.
Notes:
- Area above gland appears crusted.
DDx:
Images:
Nodular hidradenoma
General
- Benign adnexal tumour.[60]
Typical locations:[59]
- Scalp.
- Face.
- Trunk, anterior.
Microscopic
Features:[60]
- Well-circumscribed dermal lesions with:
- Back-to-back nests with a whorled appearance.
- Spaces between cells.
- Nuclei ovoid and centrally placed in the cell.
- No nucleolus.
- Cystic spaces with degenerated cells.
DDx:
Images
IHC
Features:[60]
- CAM5.2 +ve.
- AE1/AE3 +ve.
- EMA +ve.
- S100 -ve.
- Desmin -ve.
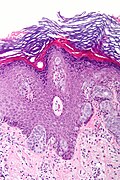
Trichoblastoma
- AKA trichoepithelioma.
- Trichoepithelioma is considered a superficial version of trichoblastoma; WHO lumps the two entities together.[61]
General
- Benign.
- Maligant counterpart of trichoepithelioma: trichilemmal carcinoma.
- May be familial:
- Multiple familial trichoepithelioma.[62]
- Brooke-Spiegler syndrome.
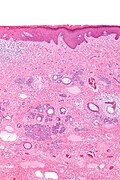
Microscopic
Features:[63]
- Well-circumscribed cell nest in the superficial dermis.
- Surrounding by a fibrous stroma.
- Basaloid cells with peripheral palisading.
- +/-Surround keratin-filled cysts.
- Fibroblasts-like cell aggregate, similar to a follicular papillae (papillary-mesenchymal body).
Notes:
- Very rarely an artefactual cleft - as in basal cell carcinoma.
Variants:
- Desmoplastic trichoblastoma.
DDx:
- Basal cell carcinoma - usu. mitoses, myxoid stroma and no papillary-mesenchymal bodies.
- Dermal cylindroma - has hyaline stroma.
- Trichofolliculoma.
- Sebaceous carcinoma, well-differentiated - has some cells with clear vacuolated cytoplasm.
Images
www:
- Papillary-mesenchymal body (medscape.com).[64]
- Papillary-mesenchymal body (skinpathologyatlas.com).[65]
- Trichoepithelioma (dermnetnz.org).
Sign out
SKIN LESION, NOSE, BIOPSY: - TRICHOBLASTOMA, COMPLETELY EXCISED.
Micro
The sections show well-circumscribed dermal nests of basaloid cells with peripheral palisading surrounded by a dense fibrous stroma. There is no artefactual clefting between the stroma and basaloid cell nests. Mitotic activity is minimal. Smaller hyperchromatic spindled-to-epithelioid cells in clusters (papillary-mesenchymal bodies) are found within the basaloid cells nests.
The epidermis show maturation to the surface and does not have basal atypia.
The lesion is completely excised in the plane of section.
Trichofolliculoma
General
- Benign.
Microscopic
Features:[66]
- Irregular hair follicle (basilar nest of cells with an acellular hair shaft) with:
- Smaller satellites (follicles) consisting of well-circumscribed basilar cells.
Note:
- Lack artificial clefting between the (basilar) nests and stroma (seen in BCC).
- Surrounding stroma does not have a basophilic tingle (seen in BCC).
DDx:
Images
www:
Apocrine carcinoma of the skin
General
Microscopic
Features:[67]
- Nests.
- Apocrine snouts - "decapitation secretion"
DDx:
Images
Stains
Features:[67]
- PAS +ve.
- PASD +ve.
IHC
- GCDFP-15 (gross cystic disease fluid protein-15) +ve.[67]
Dermatomyofibroma
- Should not be confused with dermatofibroma.
- Abbreviated DMF.
General
- Uncommon.
Microscopic
Features:[11]
- Poorly formed fasicles parallel to the skin surface, usu. restricted to the superficial dermis.
- Moderate cellular density - less cellular than DFSP.
- Eosinophilic cytoplasm.
DDx:
Images:
IHC
Features:[11]
- CD10 +ve.
- Vimentin +ve.
Others:[11]
- CD34 -ve.
- Factor XIIIa -ve.
- S-100 -ve.
Papillary eccrine adenoma
- Abbreviated PEA.
General
- Uncommon.
- Benign.[68]
Treatment:
- Excision.[69]
Gross
- Central location.
Note:
- The digital papillary adenoma is considered malignant; the AFIP says these are best classified as adenocarcinomas, i.e. digital papillary adenocarcinoma.[70]
Microscopic
- Well-circumscribed lesions consisting of multiple cystic spaces lined by a bilayered epithelium with:
- Papillary projections into the lumen.
- Amorphous eosinophilic material in the cystic spaces.
- Surrounded by a fibrous stroma.[73]
Note:
- May appear to have more than two cell layers.
DDx:
- Digital papillary adenocarcinoma - location important.
- Tubular apocrine adenoma (tubulopapillary hidradenoma[74]) - a related tumour.[75]
Image:
IHC
Outer layer of epithelium:[73]
- SMA-alpha +ve.
- Keratin 14 +ve.
Inner layer of epithelium:[73]
- Keratin 8 +ve.
Other stains:[72]
- Vimentin +ve.
- CEA +ve.
- EMA +ve.
- S-100 +ve.
Sign out
SKIN LESION, LEFT PARIETAL SCALP, BIOPSY: - PAPILLARY ECCRINE ADENOMA.
Micro
The sections show a well-circumscribed multi-locular superficial dermal lesion with a bilayered epithelium and intracystic papillary projections. The cystic spaces contain amorphous eosinophilic material. The cystic component is surrounded by a dense fibrous stroma with a mixed inflammatory infiltrate, consisting primary of plasma cells and lymphocytes.
There is no significant nuclear atypia and no mitotic activity is appreciated. The overlying epidermis matures appropriately. A granular layer is present.
See also
References
- ↑ 1.0 1.1 Kumar, Vinay; Abbas, Abul K.; Fausto, Nelson; Aster, Jon (2009). Robbins and Cotran pathologic basis of disease (8th ed.). Elsevier Saunders. pp. 1180. ISBN 978-1416031215.
- ↑ RS. 17 May 2010.
- ↑ URL: http://www.cap.org/apps/docs/committees/cancer/cancer_protocols/2011/SkinSquamousCell_11protocol.pdf. Accessed on: 29 March 2012.
- ↑ Buethe, D.; Warner, C.; Miedler, J.; Cockerell, CJ. (2011). "Focus Issue on Squamous Cell Carcinoma: Practical Concerns Regarding the 7th Edition AJCC Staging Guidelines.". J Skin Cancer 2011: 156391. doi:10.1155/2011/156391. PMC 2990020. PMID 21151529. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2990020/.
- ↑ RS. May 2010.
- ↑ URL: http://emedicine.medscape.com/article/1101235-workup#a0721. Accessed on: 2 September 2011.
- ↑ Nofech-Mozes, S.; Hanna, W.. "Toker cells revisited.". Breast J 15 (4): 394-8. doi:10.1111/j.1524-4741.2009.00743.x. PMID 19601945.
- ↑ Stacchiotti, S.; Pedeutour, F.; Negri, T.; Conca, E.; Marrari, A.; Palassini, E.; Collini, P.; Keslair, F. et al. (Oct 2011). "Dermatofibrosarcoma protuberans-derived fibrosarcoma: clinical history, biological profile and sensitivity to imatinib.". Int J Cancer 129 (7): 1761-72. doi:10.1002/ijc.25826. PMID 21128251.
- ↑ 9.0 9.1 Kumar, Vinay; Abbas, Abul K.; Fausto, Nelson; Aster, Jon (2009). Robbins and Cotran pathologic basis of disease (8th ed.). Elsevier Saunders. pp. 1183. ISBN 978-1416031215.
- ↑ Mitchell, Richard; Kumar, Vinay; Fausto, Nelson; Abbas, Abul K.; Aster, Jon (2011). Pocket Companion to Robbins & Cotran Pathologic Basis of Disease (8th ed.). Elsevier Saunders. pp. 600. ISBN 978-1416054542.
- ↑ 11.0 11.1 11.2 11.3 Busam, Klaus J. (2009). Dermatopathology: A Volume in the Foundations in Diagnostic Pathology Series (1st ed.). Saunders. pp. 504. ISBN 978-0443066542.
- ↑ AP. May 2009.
- ↑ 13.0 13.1 Abenoza P, Lillemoe T (October 1993). "CD34 and factor XIIIa in the differential diagnosis of dermatofibroma and dermatofibrosarcoma protuberans". Am J Dermatopathol 15 (5): 429–34. PMID 7694515.
- ↑ 14.0 14.1 Goldblum JR, Tuthill RJ (April 1997). "CD34 and factor-XIIIa immunoreactivity in dermatofibrosarcoma protuberans and dermatofibroma". Am J Dermatopathol 19 (2): 147–53. PMID 9129699.
- ↑ Kumar, Vinay; Abbas, Abul K.; Fausto, Nelson; Aster, Jon (2009). Robbins and Cotran pathologic basis of disease (8th ed.). Elsevier Saunders. pp. 1249. ISBN 978-1416031215.
- ↑ URL: http://emedicine.medscape.com/article/1099540-overview. Accessed on: 24 August 2010.
- ↑ URL: http://emedicine.medscape.com/article/1099540-overview. Accessed on: 24 August 2010.
- ↑ URL: http://emedicine.medscape.com/article/1098342-overview. Accessed on: 24 August 2010.
- ↑ 19.0 19.1 Klatt, Edward C. (2006). Robbins and Cotran Atlas of Pathology (1st ed.). Saunders. pp. 385. ISBN 978-1416002741.
- ↑ Kumar, Vinay; Abbas, Abul K.; Fausto, Nelson; Aster, Jon (2009). Robbins and Cotran pathologic basis of disease (8th ed.). Elsevier Saunders. pp. 1185. ISBN 978-1416031215.
- ↑ 21.0 21.1 URL: http://www.ispub.com/journal/the_internet_journal_of_otorhinolaryngology/volume_9_number_2_11/article/sebaceous_adenocarcinoma_of_the_parotid_gland_a_case_report_and_literature_review.html. Accessed on: 8 September 2011.
- ↑ Busam, Klaus J. (2009). Dermatopathology: A Volume in the Foundations in Diagnostic Pathology Series (1st ed.). Saunders. pp. 431. ISBN 978-0443066542.
- ↑ 23.0 23.1 23.2 Busam, Klaus J. (2009). Dermatopathology: A Volume in the Foundations in Diagnostic Pathology Series (1st ed.). Saunders. pp. 431-2. ISBN 978-0443066542.
- ↑ Ansai, S.; Arase, S.; Kawana, S.; Kimura, T. (Oct 2011). "Immunohistochemical findings of sebaceous carcinoma and sebaceoma: retrieval of cytokeratin expression by a panel of anti-cytokeratin monoclonal antibodies.". J Dermatol 38 (10): 951-8. doi:10.1111/j.1346-8138.2011.01274.x. PMID 21592202.
- ↑ 25.0 25.1 Sinard, JH. (Jun 1999). "Immunohistochemical distinction of ocular sebaceous carcinoma from basal cell and squamous cell carcinoma.". Arch Ophthalmol 117 (6): 776-83. PMID 10369589.
- ↑ 26.0 26.1 URL: http://www.dermaamin.com/site/histopathology-of-the-skin/65-m/1926-microcystic-adnexal-carcinoma-.html. Accessed on: 16 September 2011.
- ↑ Busam, Klaus J. (2009). Dermatopathology: A Volume in the Foundations in Diagnostic Pathology Series (1st ed.). Saunders. pp. 412. ISBN 978-0443066542.
- ↑ Kirzhner, M.; Jakobiec, FA.; Borodic, G.. "Desmoplastic trichoepithelioma: report of a unique periocular case.". Ophthal Plast Reconstr Surg 28 (5): e121-3. doi:10.1097/IOP.0b013e318245535a. PMID 22366669.
- ↑ Sellheyer, K.; Nelson, P.; Kutzner, H.; Patel, RM. (Apr 2013). "The immunohistochemical differential diagnosis of microcystic adnexal carcinoma, desmoplastic trichoepithelioma and morpheaform basal cell carcinoma using BerEP4 and stem cell markers.". J Cutan Pathol 40 (4): 363-70. doi:10.1111/cup.12085. PMID 23398472.
- ↑ Busam, Klaus J. (2009). Dermatopathology: A Volume in the Foundations in Diagnostic Pathology Series (1st ed.). Saunders. pp. 399-400. ISBN 978-0443066542.
- ↑ URL: http://path.upmc.edu/cases/case513/dx.html. Accessed on: 25 January 2012.
- ↑ 32.0 32.1 Martin, RC.; Edwards, MJ.; Cawte, TG.; Sewell, CL.; McMasters, KM. (Mar 2000). "Basosquamous carcinoma: analysis of prognostic factors influencing recurrence.". Cancer 88 (6): 1365-9. PMID 10717618.
- ↑ 33.0 33.1 Bowman, PH.; Ratz, JL.; Knoepp, TG.; Barnes, CJ.; Finley, EM. (Aug 2003). "Basosquamous carcinoma.". Dermatol Surg 29 (8): 830-2; discussion 833. PMID 12859383..
- ↑ 34.0 34.1 Busam, Klaus J. (2009). Dermatopathology: A Volume in the Foundations in Diagnostic Pathology Series (1st ed.). Saunders. pp. 397. ISBN 978-0443066542.
- ↑ Busam, Klaus J. (2009). Dermatopathology: A Volume in the Foundations in Diagnostic Pathology Series (1st ed.). Saunders. pp. 372. ISBN 978-0443066542.
- ↑ URL: http://emedicine.medscape.com/article/1056204-overview. Accessed on 2 September 2011.
- ↑ Withers, AH.; Brougham, ND.; Barber, RM.; Tan, ST. (Jun 2011). "Atypical fibroxanthoma and malignant fibrous histiocytoma.". J Plast Reconstr Aesthet Surg. doi:10.1016/j.bjps.2011.05.004. PMID 21664889.
- ↑ Ghazarian, Danny; 16 September 2011.
- ↑ New, D.; Bahrami, S.; Malone, J.; Callen, JP. (Dec 2010). "Atypical fibroxanthoma with regional lymph node metastasis: report of a case and review of the literature.". Arch Dermatol 146 (12): 1399-404. doi:10.1001/archdermatol.2010.206. PMID 20713774.
- ↑ Beer, TW.; Drury, P.; Heenan, PJ. (Aug 2010). "Atypical fibroxanthoma: a histological and immunohistochemical review of 171 cases.". Am J Dermatopathol 32 (6): 533-40. doi:10.1097/DAD.0b013e3181c80b97. PMID 20526171.
- ↑ 41.0 41.1 Busam, Klaus J. (2009). Dermatopathology: A Volume in the Foundations in Diagnostic Pathology Series (1st ed.). Saunders. pp. 521. ISBN 978-0443066542.
- ↑ Vandergriff, TW.; Reed, JA.; Orengo, IF. (2008). "An unusual presentation of atypical fibroxanthoma.". Dermatol Online J 14 (1): 6. PMID 18319023.
- ↑ Kumar, Vinay; Abbas, Abul K.; Fausto, Nelson; Aster, Jon (2009). Robbins and Cotran pathologic basis of disease (8th ed.). Elsevier Saunders. pp. 1177. ISBN 978-1416031215.
- ↑ URL: http://emedicine.medscape.com/article/1059871-diagnosis. Accessed on: 12 May 2010.
- ↑ Boecker, W.; Junkers, T.; Reusch, M.; Buerger, H.; Korsching, E.; Metze, D.; Decker, T.; Loening, T. et al. (2012). "Origin and differentiation of breast nipple syringoma.". Sci Rep 2: 226. doi:10.1038/srep00226. PMID 22355740.
- ↑ Nosrati, N.; Coleman, NM.; Hsu, S. (2008). "Axillary syringomas.". Dermatol Online J 14 (4): 13. PMID 18627735.
- ↑ 47.0 47.1 47.2 Kumar, B. (Jan 2010). "Chondroid syringoma diagnosed by fine needle aspiration cytology.". Diagn Cytopathol 38 (1): 38-40. doi:10.1002/dc.21159. PMID 19693940.
- ↑ 48.0 48.1 Rauso, R.; Santagata, M.; Tartaro, G.; Filipi, M.; Colella, G.. "Chondroid syringoma: a rare tumor of orofacial region.". Minerva Stomatol 58 (7-8): 383-8. PMID 19633639.
- ↑ 49.0 49.1 URL: http://www.ispub.com/journal/the_internet_journal_of_dermatology/volume_7_number_2_23/article/cutaneous_mixed_tumor.html. Access on: 21 September 2011.
- ↑ 50.0 50.1 50.2 50.3 50.4 Obaidat, NA.; Alsaad, KO.; Ghazarian, D. (Feb 2007). "Skin adnexal neoplasms--part 2: an approach to tumours of cutaneous sweat glands.". J Clin Pathol 60 (2): 145-59. doi:10.1136/jcp.2006.041608. PMC 1860616. PMID 16882695. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1860616/.
- ↑ Gerber, JE.; Descalzi, ME. (Feb 1983). "Eccrine spiradenoma and dermal cylindroma.". J Cutan Pathol 10 (1): 73-8. PMID 6302142.
- ↑ Lee, MW.; Kelly, JW. (Feb 1996). "Dermal cylindroma and eccrine spiradenoma.". Australas J Dermatol 37 (1): 48-9. PMID 8936072.
- ↑ URL: http://emedicine.medscape.com/article/1059940-overview. Accessed on: 2 September 2011.
- ↑ Baykal, C.; Buyukbabani, N.; Yazganoglu, KD.; Saglik, E. (Jan 2006). "[Tumors associated with nevus sebaceous].". J Dtsch Dermatol Ges 4 (1): 28-31. doi:10.1111/j.1610-0387.2006.05855.x. PMID 16503928.
- ↑ 55.0 55.1 Busam, Klaus J. (2009). Dermatopathology: A Volume in the Foundations in Diagnostic Pathology Series (1st ed.). Saunders. pp. 386. ISBN 978-0443066542.
- ↑ 56.0 56.1 URL: http://ccr.cancer.gov/staff/gallery.asp?profileid=12822. Accessed on: 2 September 2011.
- ↑ URL: http://dermatlas.med.jhmi.edu/derm/indexDisplay.cfm?ImageID=667496720. Accessed on: 2 September 2011.
- ↑ URL: http://www.pathconsultddx.com/pathCon/diagnosis?pii=S1559-8675(06)70190-5. Accessed on: 2 July 2010.
- ↑ 59.0 59.1 Punia, RP.; Garg, S.; Bal, A.; Mohan, H. (2008). "Pigmented nodular hidradenoma masquerading as nodular malignant melanoma.". Dermatol Online J 14 (1): 15. PMID 18319032.
- ↑ 60.0 60.1 60.2 Stratigos, AJ.; Olbricht, S.; Kwan, TH.; Bowers, KE. (Mar 1998). "Nodular hidradenoma. A report of three cases and review of the literature.". Dermatol Surg 24 (3): 387-91. PMID 9537017.
- ↑ Busam, Klaus J. (2009). Dermatopathology: A Volume in the Foundations in Diagnostic Pathology Series (1st ed.). Saunders. pp. 383. ISBN 978-0443066542.
- ↑ Salhi, A.; Bornholdt, D.; Oeffner, F.; Malik, S.; Heid, E.; Happle, R.; Grzeschik, KH. (Aug 2004). "Multiple familial trichoepithelioma caused by mutations in the cylindromatosis tumor suppressor gene.". Cancer Res 64 (15): 5113-7. doi:10.1158/0008-5472.CAN-04-0307. PMID 15289313.
- ↑ URL: http://emedicine.medscape.com/article/1060049-workup#a0723. Accessed on: 31 August 2011.
- ↑ URL: http://emedicine.medscape.com/article/1060049-workup#a0723 Papillary-mesenchymal body (emedicine.medscape.com). Accessed on: 22 August 2012.
- ↑ URL: http://skinpathologyatlas.com/tumors/hair/trichofollic.htm. Accessed on: 22 August 2012.
- ↑ Busam, Klaus J. (2009). Dermatopathology: A Volume in the Foundations in Diagnostic Pathology Series (1st ed.). Saunders. pp. 382. ISBN 978-0443066542.
- ↑ 67.0 67.1 67.2 67.3 67.4 Paties, C.; Taccagni, GL.; Papotti, M.; Valente, G.; Zangrandi, A.; Aloi, F. (Jan 1993). "Apocrine carcinoma of the skin. A clinicopathologic, immunocytochemical, and ultrastructural study.". Cancer 71 (2): 375-81. PMID 7678545.
- ↑ Rulon, DB.; Helwig, EB. (May 1977). "Papillary eccrine adenoma.". Arch Dermatol 113 (5): 596-8. PMID 857729.
- ↑ URL: http://archderm.jamanetwork.com/article.aspx?articleid=541159. Accessed on: 10 December 2012.
- ↑ Duke, WH.; Sherrod, TT.; Lupton, GP. (Jun 2000). "Aggressive digital papillary adenocarcinoma (aggressive digital papillary adenoma and adenocarcinoma revisited).". Am J Surg Pathol 24 (6): 775-84. PMID 10843279.
- ↑ 71.0 71.1 Laxmisha, C.; Thappa, DM.; Jayanthi, S.. "Papillary eccrine adenoma.". Indian J Dermatol Venereol Leprol 70 (6): 370-2. PMID 17642667.
- ↑ 72.0 72.1 Guccion, JG.; Patterson, RH.; Nayar, R.; Saini, NB.. "Papillary eccrine adenoma: an ultrastructural and immunohistochemical study.". Ultrastruct Pathol 22 (3): 263-9. PMID 9793207.
- ↑ 73.0 73.1 73.2 Mizuoka, H.; Senzaki, H.; Shikata, N.; Uemura, Y.; Tsubura, A. (Jan 1998). "Papillary eccrine adenoma: immunohistochemical study and literature review.". J Cutan Pathol 25 (1): 59-64. PMID 9508346.
- ↑ Fox, SB.; Cotton, DW. (Apr 1992). "Tubular apocrine adenoma and papillary eccrine adenoma. Entities or unity?". Am J Dermatopathol 14 (2): 149-54. PMID 1566975.
- ↑ Ishiko, A.; Shimizu, H.; Inamoto, N.; Nakmura, K. (Oct 1993). "Is tubular apocrine adenoma a distinct clinical entity?". Am J Dermatopathol 15 (5): 482-7. PMID 8238787.