Difference between revisions of "Prostate gland"
Jump to navigation
Jump to search
(→Cancer: more, ref) |
Alessandro (talk | contribs) m (added a word for clarity) |
||
| (305 intermediate revisions by one other user not shown) | |||
| Line 1: | Line 1: | ||
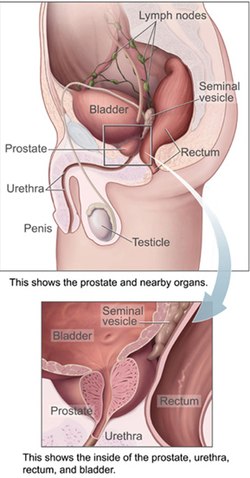
The '''prostate''' adds juice to the sperm. In old men it creates | [[Image:Prostatelead.jpg|thumb|right|200px|The prostate gland and its surrounding structures. (WC/NCI)]] | ||
The '''prostate gland''' adds juice to the sperm. In old men it creates a lot of problems... [[nodular hyperplasia]] (commonly called BPH or [[benign prostatic hyperplasia]]) and cancer (usually adenocarcinoma). | |||
==Normal== | [[Prostate cancer]] is such a big topic it is dealt with in its own article. | ||
The female homologue of the prostate gland is considered to be Skene's gland.<ref name=pmid8522254>{{Cite journal | last1 = Dodson | first1 = MK. | last2 = Cliby | first2 = WA. | last3 = Pettavel | first3 = PP. | last4 = Keeney | first4 = GL. | last5 = Podratz | first5 = KC. | title = Female urethral adenocarcinoma: evidence for more than one tissue of origin? | journal = Gynecol Oncol | volume = 59 | issue = 3 | pages = 352-7 | month = Dec | year = 1995 | doi = 10.1006/gyno.1995.9963 | PMID = 8522254 }}</ref> | |||
=Normal prostate gland= | |||
==Anatomy== | |||
Divided into three zones:<ref name=pmid2456702>{{Cite journal | last1 = McNeal | first1 = JE. | title = Normal histology of the prostate. | journal = Am J Surg Pathol | volume = 12 | issue = 8 | pages = 619-33 | month = Aug | year = 1988 | doi = | PMID = 2456702 }} | |||
</ref> | |||
#Peripheral zone - posterior aspect, palpable with digit. | |||
#*Classic location for [[prostate cancer|cancer]]. | |||
#Central zone - considered resistant to disease. | |||
#Transition zone - usual location for [[nodular hyperplasia of the prostate|nodular hyperplasia]]. | |||
==Histology== | |||
*Glands have two cell layers (similar to glands in breast). | *Glands have two cell layers (similar to glands in breast). | ||
**Second cell layer may be difficult to see (like in breast). | **Second cell layer may be difficult to see (like in breast). | ||
*Epithelium in glands | *Epithelium in glands is "folded" or "tufted". | ||
**Very important - helps | **Very important - helps to differentiate from Gleason pattern 3. | ||
*Luminal epithelium often clear | *Luminal epithelium often clear cytoplasm. | ||
*Single nucleus. | *Single nucleus. | ||
Benign normal: | |||
*Corpora amylacea. | *Corpora amylacea. | ||
**Round/ovoid-eosinophilic bodies -- with laminations (layered appearance). | **Round/ovoid-eosinophilic bodies -- with laminations (layered appearance). | ||
| Line 19: | Line 31: | ||
**These should be differentiated from ''eosinophilic proteinaceous debris'' - which is associated with cancer. | **These should be differentiated from ''eosinophilic proteinaceous debris'' - which is associated with cancer. | ||
* | Negatives: | ||
*No nucleoli present (if you see nuclei think: cancer, HGPIN, reactive changes, basal cell hyperplasia). | |||
*No mitoses - these are uncommon... even in high grade prostate cancer. | |||
Notes: | |||
*Tufted epithelium is a strong indicator of benignancy; however two uncommon prostate cancer variants typically have tufted epithelium: | |||
**[[Pseudohyperplastic adenocarcinoma]]. | |||
**[[Foamy gland carcinoma]]. | |||
====Images==== | |||
<gallery> | |||
Image:Corpora_amylacea_low_mag.jpg | Benign prostate with corpora amylacea - low mag. (WC/Nephron) | |||
Image:Corpora_amylacea_high_mag.jpg | Benign prostate with corpora amylacea - high mag. (WC/Nephron) | |||
</gallery> | |||
==IHC of normal prostate== | |||
Normal prostate: | Normal prostate: | ||
AMACR-, p63+, HMWCK+ | *[[AMACR]] -ve (mark epithelial cells). | ||
*[[CK5/6]] +ve,<ref name=pmid19605815>{{Cite journal | last1 = Trpkov | first1 = K. | last2 = Bartczak-McKay | first2 = J. | last3 = Yilmaz | first3 = A. | title = Usefulness of cytokeratin 5/6 and AMACR applied as double sequential immunostains for diagnostic assessment of problematic prostate specimens. | journal = Am J Clin Pathol | volume = 132 | issue = 2 | pages = 211-20; quiz 307 | month = Aug | year = 2009 | doi = 10.1309/AJCPGFJP83IXZEUR | PMID = 19605815 }}</ref> p63 +ve, HMWCK +ve (mark basal cells). | |||
*PSA ([[prostate-specific antigen]]) +ve, PSAP ([[prostatic-specific acid phosphatase]]) +ve. | |||
== | ==Sign out== | ||
===Staining slightly abnormal - morphology not definitely abnormal=== | |||
<pre> | |||
COMMENT: | |||
Very focal AMACR staining is seen; this is interpreted as negative, in the | |||
context of no definite cytologic changes. The basal cells appear to be | |||
preserved in all of the tissue sampled. | |||
</pre> | |||
== | ===Compatible with previous biopsy=== | ||
<pre> | |||
COMMENT: | |||
Siderophages are seen in several cores; this is compatible with the history | |||
of a previous biopsy. | |||
</pre> | |||
=== | =Other accessory glands= | ||
* | ==Bulbourethral gland== | ||
*[[AKA]] ''Cowper's gland''. | |||
{{Main|Bulbourethral gland}} | |||
=== | ==Seminal vesicles== | ||
{{Main|Seminal vesicles}} | |||
=Specimens= | |||
* | *[[Prostate core biopsy]] - done transrectal. | ||
*[[Prostate chips]] (from a ''transurethral resection of the prostate'', abbreviated ''TURP'') - usu. done for [[nodular hyperplasia of the prostate gland]]; may be done in the context of obstructing cancer. | |||
*[[Radical prostatectomy]] - includes the [[seminal vesicles]]. | |||
*[[Radical cystoprostatectomy]] - includes the [[urinary bladder]] and [[seminal vesicles]].<ref>URL: [http://www.cancer.gov/dictionary?cdrid=446218 http://www.cancer.gov/dictionary?cdrid=446218]. Accessed on: 23 February 2012.</ref> | |||
= | =Approach= | ||
* | *Know the common diagnoses well. | ||
* | *Core biopsies - scan the slides with the 10x objective. | ||
=== | ==Common diagnoses== | ||
*Benign. | |||
**[[Atrophy of the prostate|Atrophy]] - may resemble adenocarcinoma - typically not reported. | |||
**[[Adenosis of the prostate|Adenosis]] - may resemble adenocarcinoma - typically not reported. | |||
*[[Prostate adenocarcinoma]]. | |||
*[[HGPIN]] (high-grade prostatic intraepithelial neoplasia) - prostate adenocarcinoma precursor lesion. | |||
*[[ASAP]] (atypical small acinar proliferation) - used if you have a few abnormal appearing glands... but can't decide between prostate adenocarcinoma & benign. | |||
*Chronic inflammation. | |||
*Acute inflammation - can result in an elevated PSA and may have prompted the biopsy you're looking at. | |||
*[[Nodular hyperplasia of the prostate]]; [[AKA]] ''benign prostatic hypertrophy'' (BPH). | |||
**Not diagnosed on needle biopsies. | |||
**''BPH'' is technically incorrect -- the process is a hyperplasia. | |||
***Hyperplasia = proliferation of cells, hypertrophy = enlargement of cells. | |||
****How to remember? A. '''P'''rostate... hyper'''P'''lasia. | |||
== | =Clinical history= | ||
* | {{Main|Prostate specific antigen}} | ||
* | *[[PSA]] (serum). | ||
** | ** >10 ng/mL worrisome for prostate cancer. | ||
** Normal is age dependent - increases with age, usu. cut-off ~ 4 ng/mL. | |||
*HIFU = ''High Intensity Focused Ultrasound'' - an ablation procedure for prostate cancer.<ref>URL: [http://www.internationalhifu.com/what-is-hifu-mainmenu-132.html http://www.internationalhifu.com/what-is-hifu-mainmenu-132.html]. Accessed on: 15 June 2010.</ref> | |||
==== | =Benign changes and remnants= | ||
* | ==Adenosis of the prostate gland== | ||
*[[AKA]] ''atypical adenomatous hyperplasia of the prostate gland'' (or ''atypical adenomatous hyperplasia''). | |||
{{Main|Adenosis of the prostate gland}} | |||
== | ==Basal cell hyperplasia of the prostate== | ||
{{Main|Basal cell hyperplasia of the prostate}} | |||
== | ==Atrophy of the prostate== | ||
* | *[[AKA]] ''atrophy''. | ||
* | *[[AKA]] ''prostatic atrophy''. | ||
* | *[[AKA]] ''atrophy of the prostate gland''. | ||
{{Main|Atrophy of the prostate gland}} | |||
==== | ==Mesonephric remnant of the prostate gland== | ||
{{Main|Mesonephric remnant of the prostate gland}} | |||
=Benign conditions= | |||
* | ==Prostatic nodular hyperplasia== | ||
**It | *[[AKA]] ''nodular hyperplasia of the prostate''. | ||
*AKA ''benign prostatic hyperplasia'' (abbreviated BPH). | |||
*AKA ''benign prostatic hypertrophy''. | |||
**This is a misnomer. It is ''not'' a hypertrophy. | |||
{{Main|Nodular hyperplasia of the prostate}} | |||
=== | ==Acute inflammation of the prostate gland== | ||
{{ Infobox external links | |||
* | | Name = {{PAGENAME}} | ||
* | | EHVSC = 10176 | ||
| pathprotocols = | |||
| wikipedia = | |||
| pathoutlines = | |||
}} | |||
*[[AKA]] ''prostate gland with acute inflammation''. | |||
===General=== | |||
*A may lead to an increase in the PSA and prompt biopsy. | |||
Note: | |||
*"[[Prostatitis]]" is considered a clinical diagnosis. | |||
**Cases are signed out as "acute inflammation". | |||
***Some pathologists do not comment on the presence (or absence) of inflammation. | |||
===Microscopic=== | |||
Features: | |||
=== | *[[Neutrophil]]s within the glands, between the epithelial cells ''or'' within the stroma - '''key feature'''. | ||
*+/-Chronic inflammation (lymphocytes) within the surrounding stroma. | |||
* | |||
* | |||
DDx: | |||
*[[Prostatic infarction]]. | |||
* | |||
=== | ====Image==== | ||
<gallery> | |||
Image:Acute_inflammation_of_prostate.jpg| Prostate with acute inflammation. (WC/Nephron) | |||
</gallery> | |||
===Sign out=== | |||
<pre> | |||
G. PROSTATE, LEFT LATERAL SUPERIOR, BIOPSY: | |||
- BENIGN PROSTATE TISSUE; | |||
- FOCAL ACUTE INFLAMMATION. | |||
</pre> | |||
<pre> | |||
G. PROSTATE, LEFT LATERAL SUPERIOR, BIOPSY: | |||
- BENIGN PROSTATE TISSUE; | |||
- FOCAL ACUTE AND CHRONIC INFLAMMATION. | |||
</pre> | |||
== | ==Chronic inflammation not otherwise specified== | ||
===General=== | |||
* | *Common. | ||
* | *Non-specific finding. | ||
* | *Etiology usually not apparent on histomorphology. | ||
===Microscopic=== | |||
Features: | |||
*Lymphocytes within the glands, between the epithelial cells ''or'' within the stroma - '''key feature'''. | |||
Notes: | |||
*Rare scattered lymphocytes are common, especially in the central portion of the gland. | |||
* | *"Focal" one field with a 2.2 mm diameter involved. | ||
* | |||
====Image==== | |||
<gallery> | |||
Image:Inflammation_of_prostate.jpg | Prostate with chronic inflammation. (WC/Nephron) | |||
</gallery> | |||
===Sign out=== | |||
<pre> | |||
G. PROSTATE, LEFT LATERAL SUPERIOR, BIOPSY: | |||
- BENIGN PROSTATE TISSUE; | |||
- FOCAL CHRONIC INFLAMMATION. | |||
</pre> | |||
<pre> | |||
F. PROSTATE, RIGHT MEDIAL MIDZONE, BIOPSY: | |||
- BENIGN PROSTATE TISSUE; | |||
- CHRONIC INFLAMMATION. | |||
</pre> | |||
Note: | |||
* | *Opinion is divided on whether this finding should be reported. | ||
**Advocates for reporting inflammation say "[i]t is just reporting what you see and may explain the bump in PSA." | |||
**Naysayers opine that "[i]t may provide false assurance that no cancer is present." | |||
==Granulomatous prostatitis== | |||
{{Main|Granulomatous prostatitis}} | |||
==Prostatic infarct== | |||
* | *[[AKA]] ''prostatic [[infarction]]''. | ||
* | ===General=== | ||
* | *Rare < 0.1% of core biopsies.<ref name=pmid11023099>{{Cite journal | last1 = Milord | first1 = RA. | last2 = Kahane | first2 = H. | last3 = Epstein | first3 = JI. | title = Infarct of the prostate gland: experience on needle biopsy specimens. | journal = Am J Surg Pathol | volume = 24 | issue = 10 | pages = 1378-84 | month = Oct | year = 2000 | doi = | PMID = 11023099 }}</ref> | ||
*Can mimic cancer - [[urothelial carcinoma]].<ref name=pmid11023099/> | |||
*Prostate usually large. | |||
== | ===Microscopic=== | ||
Features: | |||
* | *Classic findings of [[necrosis]]: | ||
**Karyolysis (loss of nuclei), karyorrhexis (frag. of nuclei), pyknosis (small shrunken nuclei). | |||
** | *+/-Squamous metaplasia of prostate gland epithelium. | ||
* | |||
Notes: | |||
* | *Corpora amylacea - help... call it benign. | ||
* | *Glands maintain normal spacing. | ||
DDx: | |||
*[[Urothelial carcinoma]] with squamous differentiation. | |||
* | |||
Image: | |||
* | *[http://www.sciencephoto.com/media/258565/enlarge Prostatic thrombosis (sciencephoto.com)]. | ||
=== | =Preneoplastic changes and atypical changes= | ||
==High-grade prostatic intraepithelial neoplasia== | |||
* | *Abbreviated as ''HGPIN''. | ||
* | *May be referred to as ''prostatic intraepithelial neoplasia'', abbreviated ''PIN''. | ||
{{Main|High-grade prostatic intraepithelial neoplasia}} | |||
==Atypical small acinar proliferation== | ==Atypical small acinar proliferation== | ||
*Abbreviated ''ASAP''. | *Abbreviated ''ASAP''. | ||
* | *[[AKA]] ''suspicious for carcinoma''.<ref>THvdK. 19 June 2010.</ref> | ||
**''ASAP'' is preferred as it does not contain the word ''carcinoma'' and, thus, cannot be misread as ''carcinoma'', i.e. positive for malignancy. | |||
{{Main|Atypical small acinar proliferation}} | |||
* | |||
* | |||
=Prostate cancer= | |||
{{Main|Prostate cancer}} | |||
This is a big topic that is dealt with in its own article. | |||
=See also= | |||
*[[Urothelium]]. | *[[Urothelium]]. | ||
*[[Genitourinary pathology]]. | *[[Genitourinary pathology]]. | ||
=References= | |||
{{reflist|2}} | {{reflist|2}} | ||
[[Category: Genitourinary pathology]] | [[Category: Genitourinary pathology]] | ||
Latest revision as of 19:21, 10 February 2019
The prostate gland adds juice to the sperm. In old men it creates a lot of problems... nodular hyperplasia (commonly called BPH or benign prostatic hyperplasia) and cancer (usually adenocarcinoma).
Prostate cancer is such a big topic it is dealt with in its own article.
The female homologue of the prostate gland is considered to be Skene's gland.[1]
Normal prostate gland
Anatomy
Divided into three zones:[2]
- Peripheral zone - posterior aspect, palpable with digit.
- Classic location for cancer.
- Central zone - considered resistant to disease.
- Transition zone - usual location for nodular hyperplasia.
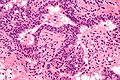
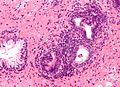
Histology
- Glands have two cell layers (similar to glands in breast).
- Second cell layer may be difficult to see (like in breast).
- Epithelium in glands is "folded" or "tufted".
- Very important - helps to differentiate from Gleason pattern 3.
- Luminal epithelium often clear cytoplasm.
- Single nucleus.
Benign normal:
- Corpora amylacea.
- Round/ovoid-eosinophilic bodies -- with laminations (layered appearance).
- In gland lumina.
- Usually in benign glands - but cannot be used to exclude cancer.[3]
- Very common.
- These should be differentiated from eosinophilic proteinaceous debris - which is associated with cancer.
Negatives:
- No nucleoli present (if you see nuclei think: cancer, HGPIN, reactive changes, basal cell hyperplasia).
- No mitoses - these are uncommon... even in high grade prostate cancer.
Notes:
- Tufted epithelium is a strong indicator of benignancy; however two uncommon prostate cancer variants typically have tufted epithelium:
Images
IHC of normal prostate
Normal prostate:
- AMACR -ve (mark epithelial cells).
- CK5/6 +ve,[4] p63 +ve, HMWCK +ve (mark basal cells).
- PSA (prostate-specific antigen) +ve, PSAP (prostatic-specific acid phosphatase) +ve.
Sign out
Staining slightly abnormal - morphology not definitely abnormal
COMMENT: Very focal AMACR staining is seen; this is interpreted as negative, in the context of no definite cytologic changes. The basal cells appear to be preserved in all of the tissue sampled.
Compatible with previous biopsy
COMMENT: Siderophages are seen in several cores; this is compatible with the history of a previous biopsy.
Other accessory glands
Bulbourethral gland
- AKA Cowper's gland.
Main article: Bulbourethral gland
Seminal vesicles
Main article: Seminal vesicles
Specimens
- Prostate core biopsy - done transrectal.
- Prostate chips (from a transurethral resection of the prostate, abbreviated TURP) - usu. done for nodular hyperplasia of the prostate gland; may be done in the context of obstructing cancer.
- Radical prostatectomy - includes the seminal vesicles.
- Radical cystoprostatectomy - includes the urinary bladder and seminal vesicles.[5]
Approach
- Know the common diagnoses well.
- Core biopsies - scan the slides with the 10x objective.
Common diagnoses
- Benign.
- Prostate adenocarcinoma.
- HGPIN (high-grade prostatic intraepithelial neoplasia) - prostate adenocarcinoma precursor lesion.
- ASAP (atypical small acinar proliferation) - used if you have a few abnormal appearing glands... but can't decide between prostate adenocarcinoma & benign.
- Chronic inflammation.
- Acute inflammation - can result in an elevated PSA and may have prompted the biopsy you're looking at.
- Nodular hyperplasia of the prostate; AKA benign prostatic hypertrophy (BPH).
- Not diagnosed on needle biopsies.
- BPH is technically incorrect -- the process is a hyperplasia.
- Hyperplasia = proliferation of cells, hypertrophy = enlargement of cells.
- How to remember? A. Prostate... hyperPlasia.
- Hyperplasia = proliferation of cells, hypertrophy = enlargement of cells.
Clinical history
Main article: Prostate specific antigen
- PSA (serum).
- >10 ng/mL worrisome for prostate cancer.
- Normal is age dependent - increases with age, usu. cut-off ~ 4 ng/mL.
- HIFU = High Intensity Focused Ultrasound - an ablation procedure for prostate cancer.[6]
Benign changes and remnants
Adenosis of the prostate gland
- AKA atypical adenomatous hyperplasia of the prostate gland (or atypical adenomatous hyperplasia).
Main article: Adenosis of the prostate gland
Basal cell hyperplasia of the prostate
Main article: Basal cell hyperplasia of the prostate
Atrophy of the prostate
Main article: Atrophy of the prostate gland
Mesonephric remnant of the prostate gland
Main article: Mesonephric remnant of the prostate gland
Benign conditions
Prostatic nodular hyperplasia
- AKA nodular hyperplasia of the prostate.
- AKA benign prostatic hyperplasia (abbreviated BPH).
- AKA benign prostatic hypertrophy.
- This is a misnomer. It is not a hypertrophy.
Main article: Nodular hyperplasia of the prostate
Acute inflammation of the prostate gland
| Prostate gland | |
|---|---|
| External resources | |
| EHVSC | 10176 |
- AKA prostate gland with acute inflammation.
General
- A may lead to an increase in the PSA and prompt biopsy.
Note:
- "Prostatitis" is considered a clinical diagnosis.
- Cases are signed out as "acute inflammation".
- Some pathologists do not comment on the presence (or absence) of inflammation.
- Cases are signed out as "acute inflammation".
Microscopic
Features:
- Neutrophils within the glands, between the epithelial cells or within the stroma - key feature.
- +/-Chronic inflammation (lymphocytes) within the surrounding stroma.
DDx:
Image
Sign out
G. PROSTATE, LEFT LATERAL SUPERIOR, BIOPSY: - BENIGN PROSTATE TISSUE; - FOCAL ACUTE INFLAMMATION.
G. PROSTATE, LEFT LATERAL SUPERIOR, BIOPSY: - BENIGN PROSTATE TISSUE; - FOCAL ACUTE AND CHRONIC INFLAMMATION.
Chronic inflammation not otherwise specified
General
- Common.
- Non-specific finding.
- Etiology usually not apparent on histomorphology.
Microscopic
Features:
- Lymphocytes within the glands, between the epithelial cells or within the stroma - key feature.
Notes:
- Rare scattered lymphocytes are common, especially in the central portion of the gland.
- "Focal" one field with a 2.2 mm diameter involved.
Image
Sign out
G. PROSTATE, LEFT LATERAL SUPERIOR, BIOPSY: - BENIGN PROSTATE TISSUE; - FOCAL CHRONIC INFLAMMATION.
F. PROSTATE, RIGHT MEDIAL MIDZONE, BIOPSY: - BENIGN PROSTATE TISSUE; - CHRONIC INFLAMMATION.
Note:
- Opinion is divided on whether this finding should be reported.
- Advocates for reporting inflammation say "[i]t is just reporting what you see and may explain the bump in PSA."
- Naysayers opine that "[i]t may provide false assurance that no cancer is present."
Granulomatous prostatitis
Main article: Granulomatous prostatitis
Prostatic infarct
- AKA prostatic infarction.
General
- Rare < 0.1% of core biopsies.[7]
- Can mimic cancer - urothelial carcinoma.[7]
- Prostate usually large.
Microscopic
Features:
- Classic findings of necrosis:
- Karyolysis (loss of nuclei), karyorrhexis (frag. of nuclei), pyknosis (small shrunken nuclei).
- +/-Squamous metaplasia of prostate gland epithelium.
Notes:
- Corpora amylacea - help... call it benign.
- Glands maintain normal spacing.
DDx:
- Urothelial carcinoma with squamous differentiation.
Image:
Preneoplastic changes and atypical changes
High-grade prostatic intraepithelial neoplasia
- Abbreviated as HGPIN.
- May be referred to as prostatic intraepithelial neoplasia, abbreviated PIN.
Main article: High-grade prostatic intraepithelial neoplasia
Atypical small acinar proliferation
- Abbreviated ASAP.
- AKA suspicious for carcinoma.[8]
- ASAP is preferred as it does not contain the word carcinoma and, thus, cannot be misread as carcinoma, i.e. positive for malignancy.
Main article: Atypical small acinar proliferation
Prostate cancer
Main article: Prostate cancer
This is a big topic that is dealt with in its own article.
See also
References
- ↑ Dodson, MK.; Cliby, WA.; Pettavel, PP.; Keeney, GL.; Podratz, KC. (Dec 1995). "Female urethral adenocarcinoma: evidence for more than one tissue of origin?". Gynecol Oncol 59 (3): 352-7. doi:10.1006/gyno.1995.9963. PMID 8522254.
- ↑ McNeal, JE. (Aug 1988). "Normal histology of the prostate.". Am J Surg Pathol 12 (8): 619-33. PMID 2456702.
- ↑ Christian JD, Lamm TC, Morrow JF, Bostwick DG (January 2005). "Corpora amylacea in adenocarcinoma of the prostate: incidence and histology within needle core biopsies". Mod. Pathol. 18 (1): 36–9. doi:10.1038/modpathol.3800250.
- ↑ Trpkov, K.; Bartczak-McKay, J.; Yilmaz, A. (Aug 2009). "Usefulness of cytokeratin 5/6 and AMACR applied as double sequential immunostains for diagnostic assessment of problematic prostate specimens.". Am J Clin Pathol 132 (2): 211-20; quiz 307. doi:10.1309/AJCPGFJP83IXZEUR. PMID 19605815.
- ↑ URL: http://www.cancer.gov/dictionary?cdrid=446218. Accessed on: 23 February 2012.
- ↑ URL: http://www.internationalhifu.com/what-is-hifu-mainmenu-132.html. Accessed on: 15 June 2010.
- ↑ 7.0 7.1 Milord, RA.; Kahane, H.; Epstein, JI. (Oct 2000). "Infarct of the prostate gland: experience on needle biopsy specimens.". Am J Surg Pathol 24 (10): 1378-84. PMID 11023099.
- ↑ THvdK. 19 June 2010.