Difference between revisions of "Astrocytoma, IDH-mutant"
Jump to navigation
Jump to search
Jensflorian (talk | contribs) (1st creation from diffuse and anaplastic astrocytoma) |
Jensflorian (talk | contribs) (→Molecular: image text updated) |
||
| (5 intermediate revisions by the same user not shown) | |||
| Line 1: | Line 1: | ||
'''Astrocytoma, IDH-mutant''' is a diffusely-growing, infiltrating astrocytoma of the adult occurring in the CNS white matter. IDH1 codon 132 or IDH2 codon 172 mutations are frequently associated with ATRX and TP53 mutations. | '''Astrocytoma, IDH-mutant''' is a diffusely-growing, infiltrating astrocytoma of the adult occurring in the CNS white matter. IDH1 codon 132 or IDH2 codon 172 mutations is mandatory for diagnosis and are frequently associated with ATRX and TP53 mutations. | ||
=General= | =General= | ||
| Line 7: | Line 7: | ||
* Astrocytoma, IDH mutant grade 4 (ICD-O: 9445/3) | * Astrocytoma, IDH mutant grade 4 (ICD-O: 9445/3) | ||
* Diffuse astrocytoma,NOS (ICD-O 9400/3) - genetic testing still missing. | * Diffuse astrocytoma,NOS (ICD-O 9400/3) - genetic testing still missing. | ||
The existence of diffuse astrocytoma, IDH wildtype is challenged.<ref>{{Cite journal | last1 = Reuss | first1 = DE. | last2 = Kratz | first2 = A. | last3 = Sahm | first3 = F. | last4 = Capper | first4 = D. | last5 = Schrimpf | first5 = D. | last6 = Koelsche | first6 = C. | last7 = Hovestadt | first7 = V. | last8 = Bewerunge-Hudler | first8 = M. | last9 = Jones | first9 = DT. | title = Adult IDH wild type astrocytomas biologically and clinically resolve into other tumor entities. | journal = Acta Neuropathol | volume = 130 | issue = 3 | pages = 407-17 | month = Sep | year = 2015 | doi = 10.1007/s00401-015-1454-8 | PMID = 26087904 }}</ref> Most adult IDH wildtype cases show genetic alterations identical to glioblastoma.<ref>{{Cite journal | last1 = Hasselblatt | first1 = M. | last2 = Jaber | first2 = M. | last3 = Reuss | first3 = D. | last4 = Grauer | first4 = O. | last5 = Bibo | first5 = A. | last6 = Terwey | first6 = S. | last7 = Schick | first7 = U. | last8 = Ebel | first8 = H. | last9 = Niederstadt | first9 = T. | title = Diffuse Astrocytoma, IDH-Wildtype: A Dissolving Diagnosis. | journal = J Neuropathol Exp Neurol | volume = | issue = | pages = | month = Feb | year = 2018 | doi = 10.1093/jnen/nly012 | PMID = 29444314 }}</ref> | |||
==Astrocytoma, IDH mutant grade 2== | ==Astrocytoma, IDH mutant grade 2== | ||
* Most common CNS grade 2 WHO glioma in adults (peaks between 30-40 years). | * Most common CNS grade 2 WHO glioma in adults (peaks between 30-40 years). | ||
* 10-15% of all [[astrocytoma]]s. | * 10-15% of all [[astrocytoma]]s. | ||
* Usually shows progression to | * Usually shows progression to WHO CNS grade 3 sooner or later. <ref>{{Cite journal | last1 = Louis | first1 = DN. | last2 = Perry | first2 = A. | last3 = Reifenberger | first3 = G. | last4 = von Deimling | first4 = A. | last5 = Figarella-Branger | first5 = D. | last6 = Cavenee | first6 = WK. | last7 = Ohgaki | first7 = H. | last8 = Wiestler | first8 = OD. | last9 = Kleihues | first9 = P. | title = The 2016 World Health Organization Classification of Tumors of the Central Nervous System: a summary. | journal = Acta Neuropathol | volume = 131 | issue = 6 | pages = 803-20 | month = Jun | year = 2016 | doi = 10.1007/s00401-016-1545-1 | PMID = 27157931 }}</ref> | ||
WHO | ==Astrocytoma, IDH mutant grade 3== | ||
* Most common CNS grade 3 WHO glioma in adults (peaks between 40-50 years). | |||
* Approx 5% of all [[glioma]]s.<ref>{{Cite journal | last1 = Ohgaki | first1 = H. | last2 = Kleihues | first2 = P. | title = Population-based studies on incidence, survival rates, and genetic alterations in astrocytic and oligodendroglial gliomas. | journal = J Neuropathol Exp Neurol | volume = 64 | issue = 6 | pages = 479-89 | month = Jun | year = 2005 | doi = | PMID = 15977639 }}</ref> | |||
* | * Usually shows progression to WHO CNS grade 4 sooner or later. | ||
* | *Overall prognosis is rather poor (average survival 2-3 years). | ||
*Grade 3 tumors share a similiar prognosis to grade 2 IDH-mutant tumors.<ref>{{Cite journal | last1 = Reuss | first1 = DE. | last2 = Mamatjan | first2 = Y. | last3 = Schrimpf | first3 = D. | last4 = Capper | first4 = D. | last5 = Hovestadt | first5 = V. | last6 = Kratz | first6 = A. | last7 = Sahm | first7 = F. | last8 = Koelsche | first8 = C. | last9 = Korshunov | first9 = A. | title = IDH mutant diffuse and anaplastic astrocytomas have similar age at presentation and little difference in survival: a grading problem for WHO. | journal = Acta Neuropathol | volume = 129 | issue = 6 | pages = 867-73 | month = Jun | year = 2015 | doi = 10.1007/s00401-015-1438-8 | PMID = 25962792 }}</ref> | |||
==Astrocytoma, IDH mutant grade 4== | |||
* Formely called glioblastoma, IDH-mutant or "secondary glioblastoma". | |||
* CDKN2A deletion in grade 2 or grade 3 tumors results in upgrading to CNS WHO grade 4. | |||
=Radiology/Clinic= | |||
*Mass effect. | *Mass effect. | ||
*Seizures. | *Seizures. | ||
*Neurologic decifit. | *Neurologic decifit. | ||
*Usually not contrast-enhanching, T2 bright. | *CNS grade 2: Usually not contrast-enhanching, T2 bright. | ||
*CNS grade 3 and 4: The majority are contrast-enhanching, T2 bright. | |||
=Macroscopy= | |||
*No clear demarcation from white matter | *No clear demarcation from white matter. | ||
*Softer consistency and opacity. | |||
*May contain larger cysts | *May contain larger cysts | ||
*No | *Invaded structures may appear enlarged. | ||
*CNS grade 2 and 3: No necrosis. | |||
=Histology= | |||
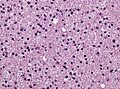
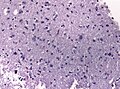
CNS grade 2 features: <ref name=AFIP2007>{{Ref AFIP2007|34}}</ref> | |||
*Cell density higher than normal brain. | *Cell density higher than normal brain. | ||
*Mild to moderate nuclear pleomorphism. | *Mild to moderate nuclear pleomorphism. | ||
| Line 43: | Line 51: | ||
*Mitoses absent or very rare. | *Mitoses absent or very rare. | ||
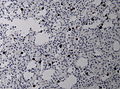
*Microcystic spaces of the background (none to extensive). | *Microcystic spaces of the background (none to extensive). | ||
*Lymphocytic cuffing (mostly in gemistocytic type) | *Lymphocytic cuffing (mostly in gemistocytic type) | ||
*Abent to few rosenthal fibers. | *Abent to few rosenthal fibers. | ||
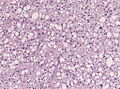
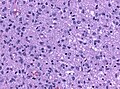
< | CNS grade 3 features: <ref name=AFIP2007>{{Ref AFIP2007|34}}</ref> | ||
*Increased cellularity (compared to CNS grade 2). | |||
*Mitoses present (a single mitosis in a small specimen indicates a high-grade tumor). | |||
**Specimens with low cellularity but plenty of mitoses are also considered grade 3. | |||
*Distinct nuclear atypia and pleomorphism. | |||
**May include multinucleated cells. | |||
*Cytoplasm highly variable (even within the same tumour). | |||
*Microcystic spaces of the background (none to extensive). | |||
*No necrosis, no vascular proliferations. | |||
**Except radiation necrosis after pretreatment. | |||
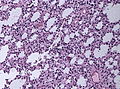
CNS grade 4 features: | |||
*Increased cellularity (compared to CNS grade 2). | |||
*Mitoses frequently present. | |||
*Distinct nuclear atypia and pleomorphism. | |||
*Multinucleated cells. | |||
*Microvascular proliferation. | |||
*Necrosis (less common than in [[glioblastoma]]). | |||
=IHC= | |||
*[[GFAP]]+ve. | *[[GFAP]]+ve. | ||
*[[MAP2]]+ve (especially in cell processes). | *[[MAP2]]+ve (especially in cell processes). | ||
*OLIG2 +ve. | |||
*Vimentin+ve (often perinuclear). | *Vimentin+ve (often perinuclear). | ||
*S-100+ve. | *S-100+ve. | ||
*p53: Nuclear staining in 30% of the tumours (usually few cells). | *p53: Nuclear staining in 30% of the tumours (usually few cells). | ||
*MIB-1: 0-5% (mean: 2%). | *MIB-1: CNS grade 2: 0-5% (mean: 2%); CNS grade 3 usu. 5-10%. | ||
*[[IDH-1]] (R132H)+ve in 60-70%. | *[[IDH-1]] (R132H)+ve in 60-70%. | ||
**'Note:'' | **'Note:'' The mutation-specific antibody does not detect other less common IDH1/2 hotspot mutations. | ||
*[[ATRX]] nuclear loss in | *[[ATRX]] nuclear loss. | ||
=Molecular= | |||
*IDH1 R132- or IDH2 R172-hotspot mutations are mandatory. | |||
*Absence of LOH 1p/19q (otherwise classify tumor as [[oligodendroglioma]], IDH-mutant and 1p/19q codeleted). | |||
*Tp53 mutations in approx. 60% (80-90% in gemistocytic, 50% in fibrillary types). | |||
*MGMT promotor methylated in approx. 50%. | |||
*CDKN2A/B homozygous deletion results in CNS grade 4<ref>{{Cite journal | last1 = Shirahata | first1 = M. | last2 = Ono | first2 = T. | last3 = Stichel | first3 = D. | last4 = Schrimpf | first4 = D. | last5 = Reuss | first5 = DE. | last6 = Sahm | first6 = F. | last7 = Koelsche | first7 = C. | last8 = Wefers | first8 = A. | last9 = Reinhardt | first9 = A. | title = Novel, improved grading system(s) for IDH-mutant astrocytic gliomas. | journal = Acta Neuropathol | volume = 136 | issue = 1 | pages = 153-166 | month = Jul | year = 2018 | doi = 10.1007/s00401-018-1849-4 | PMID = 29687258 }}</ref><ref>{{Cite journal | last1 = Aoki | first1 = K. | last2 = Nakamura | first2 = H. | last3 = Suzuki | first3 = H. | last4 = Matsuo | first4 = K. | last5 = Kataoka | first5 = K. | last6 = Shimamura | first6 = T. | last7 = Motomura | first7 = K. | last8 = Ohka | first8 = F. | last9 = Shiina | first9 = S. | title = Prognostic relevance of genetic alterations in diffuse lower-grade gliomas. | journal = Neuro Oncol | volume = 20 | issue = 1 | pages = 66-77 | month = 01 | year = 2018 | doi = 10.1093/neuonc/nox132 | PMID = 29016839 }}</ref> | |||
*Usu. no EGFR amplification, no combined whole chromosome 7 gain and whole chromosome 10 loss (+ 7/− 10). | |||
*Absence of TERT promoter mutation (if present in IDH-mutant tumour, consider oligodendroglioma).<ref>{{Cite journal | last1 = Lee | first1 = Y. | last2 = Koh | first2 = J. | last3 = Kim | first3 = SI. | last4 = Won | first4 = JK. | last5 = Park | first5 = CK. | last6 = Choi | first6 = SH. | last7 = Park | first7 = SH. | title = The frequency and prognostic effect of TERT promoter mutation in diffuse gliomas. | journal = Acta Neuropathol Commun | volume = 5 | issue = 1 | pages = 62 | month = Aug | year = 2017 | doi = 10.1186/s40478-017-0465-1 | PMID = 28851427 }}</ref><ref>{{Cite journal | last1 = Koelsche | first1 = C. | last2 = Sahm | first2 = F. | last3 = Capper | first3 = D. | last4 = Reuss | first4 = D. | last5 = Sturm | first5 = D. | last6 = Jones | first6 = DT. | last7 = Kool | first7 = M. | last8 = Northcott | first8 = PA. | last9 = Wiestler | first9 = B. | title = Distribution of TERT promoter mutations in pediatric and adult tumors of the nervous system. | journal = Acta Neuropathol | volume = 126 | issue = 6 | pages = 907-15 | month = Dec | year = 2013 | doi = 10.1007/s00401-013-1195-5 | PMID = 24154961 }}</ref> | |||
<gallery> | <gallery> | ||
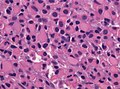
File:GFAP astrocytoma.jpg| GFAP in astrocytoma (WC/jensflorian) | File:Diffuse_astrocytoma_HE_stain.jpg | Astrocytoma, grade 2 [[H&E]] (WC/jensflorian) | ||
File:Image NP T2a 0002.JPG | Astrocytoma, grade 2 [[H&E]] (WC/jensflorian) | |||
File:Astrocytoma whoII HE.jpg | Astrocytoma, fibrillary type (WC/jensflorian) | |||
File:Neuropathology case II 02.jpg | Astrocytoma, protoplasmatic type (WC/jensflorian) | |||
File:Gemistocytic astrocytoma.jpg | Astrocytoma, gemistocytic cells (WC/jensflorian) | |||
File:Mitoses_astro_III.jpg | Marked mitotic activity in astrocytoma grade 3 (WC/jensflorian). | |||
File:405551M-ANAPLASTIC_ASTROCYTOMA.jpg | Marked nuclear pleomorphism (AFIP). | |||
File:GFAP astrocytoma.jpg| GFAP staining in astrocytoma (WC/jensflorian) | |||
File:Neuropathology case II 04.jpg | ATRX loss in astrocytoma (WC/jensflorian) | File:Neuropathology case II 04.jpg | ATRX loss in astrocytoma (WC/jensflorian) | ||
File:IDH1 GBM 20x.jpg | IDH1 R132H immunreactivity in a Grade 4 astrocytoma (WC/Marvin101) | |||
</gallery> | </gallery> | ||
==DDx== | ==DDx== | ||
| Line 102: | Line 117: | ||
For CNS grade 3 tumours: | For CNS grade 3 tumours: | ||
*Anaplastic [[Oligodendroglioma]], when LOH 1p/19q is present. | *Anaplastic [[Oligodendroglioma]], when LOH 1p/19q is present. | ||
For CNS grade 4 tumours: | |||
*[[Glioblastoma]] - vascular proliferations and / or necrosis. | *[[Glioblastoma]] - vascular proliferations and / or necrosis. | ||
==Outdated terminologies== | ==Outdated terminologies== | ||
| Line 173: | Line 124: | ||
*Gemistocytic astrocytoma | *Gemistocytic astrocytoma | ||
*Diffuse astrocytoma, IDH-wildtype | *Diffuse astrocytoma, IDH-wildtype | ||
*Glioblastoma; IDH-mutant | |||
*Fibrillary astrocytoma (ICD-O: 9420/3) | |||
*Protoplasmatic astrocytoma (ICD-O:9410/3) | |||
=See also= | =See also= | ||
Latest revision as of 09:10, 14 April 2022
Astrocytoma, IDH-mutant is a diffusely-growing, infiltrating astrocytoma of the adult occurring in the CNS white matter. IDH1 codon 132 or IDH2 codon 172 mutations is mandatory for diagnosis and are frequently associated with ATRX and TP53 mutations.
General
The current WHO classification recognizes three tumour grades:
- Astrocytoma, IDH mutant grade 2 (ICD-O: 9400/3)
- Astrocytoma, IDH mutant grade 3 (ICD-O: 9401/3)
- Astrocytoma, IDH mutant grade 4 (ICD-O: 9445/3)
- Diffuse astrocytoma,NOS (ICD-O 9400/3) - genetic testing still missing.
The existence of diffuse astrocytoma, IDH wildtype is challenged.[1] Most adult IDH wildtype cases show genetic alterations identical to glioblastoma.[2]
Astrocytoma, IDH mutant grade 2
- Most common CNS grade 2 WHO glioma in adults (peaks between 30-40 years).
- 10-15% of all astrocytomas.
- Usually shows progression to WHO CNS grade 3 sooner or later. [3]
Astrocytoma, IDH mutant grade 3
- Most common CNS grade 3 WHO glioma in adults (peaks between 40-50 years).
- Approx 5% of all gliomas.[4]
- Usually shows progression to WHO CNS grade 4 sooner or later.
- Overall prognosis is rather poor (average survival 2-3 years).
- Grade 3 tumors share a similiar prognosis to grade 2 IDH-mutant tumors.[5]
Astrocytoma, IDH mutant grade 4
- Formely called glioblastoma, IDH-mutant or "secondary glioblastoma".
- CDKN2A deletion in grade 2 or grade 3 tumors results in upgrading to CNS WHO grade 4.
Radiology/Clinic
- Mass effect.
- Seizures.
- Neurologic decifit.
- CNS grade 2: Usually not contrast-enhanching, T2 bright.
- CNS grade 3 and 4: The majority are contrast-enhanching, T2 bright.
Macroscopy
- No clear demarcation from white matter.
- Softer consistency and opacity.
- May contain larger cysts
- Invaded structures may appear enlarged.
- CNS grade 2 and 3: No necrosis.
Histology
CNS grade 2 features: [6]
- Cell density higher than normal brain.
- Mild to moderate nuclear pleomorphism.
- Monotony of atypical nuclei and irregular distribution indicates neoplasm.
- "naked nuclei" without recognizeable processes.
- No prominent nucleolus.
- Cytoplasm highly variable (even within the same tumour).
- In normal CNS the cytoplasm blends within the neuropil.
- Mitoses absent or very rare.
- Microcystic spaces of the background (none to extensive).
- Lymphocytic cuffing (mostly in gemistocytic type)
- Abent to few rosenthal fibers.
CNS grade 3 features: [6]
- Increased cellularity (compared to CNS grade 2).
- Mitoses present (a single mitosis in a small specimen indicates a high-grade tumor).
- Specimens with low cellularity but plenty of mitoses are also considered grade 3.
- Distinct nuclear atypia and pleomorphism.
- May include multinucleated cells.
- Cytoplasm highly variable (even within the same tumour).
- Microcystic spaces of the background (none to extensive).
- No necrosis, no vascular proliferations.
- Except radiation necrosis after pretreatment.
CNS grade 4 features:
- Increased cellularity (compared to CNS grade 2).
- Mitoses frequently present.
- Distinct nuclear atypia and pleomorphism.
- Multinucleated cells.
- Microvascular proliferation.
- Necrosis (less common than in glioblastoma).
IHC
- GFAP+ve.
- MAP2+ve (especially in cell processes).
- OLIG2 +ve.
- Vimentin+ve (often perinuclear).
- S-100+ve.
- p53: Nuclear staining in 30% of the tumours (usually few cells).
- MIB-1: CNS grade 2: 0-5% (mean: 2%); CNS grade 3 usu. 5-10%.
- IDH-1 (R132H)+ve in 60-70%.
- 'Note: The mutation-specific antibody does not detect other less common IDH1/2 hotspot mutations.
- ATRX nuclear loss.
Molecular
- IDH1 R132- or IDH2 R172-hotspot mutations are mandatory.
- Absence of LOH 1p/19q (otherwise classify tumor as oligodendroglioma, IDH-mutant and 1p/19q codeleted).
- Tp53 mutations in approx. 60% (80-90% in gemistocytic, 50% in fibrillary types).
- MGMT promotor methylated in approx. 50%.
- CDKN2A/B homozygous deletion results in CNS grade 4[7][8]
- Usu. no EGFR amplification, no combined whole chromosome 7 gain and whole chromosome 10 loss (+ 7/− 10).
- Absence of TERT promoter mutation (if present in IDH-mutant tumour, consider oligodendroglioma).[9][10]
DDx
For CNS grade 2 tumours:
- Reactive astrocytosis.
- Demyelinisation.
- Grade 3 astrocytoma, IDH mutant - increased mitotic activity.
- Oligodendroglioma, IDH-mutant and 1p/19q codeleted - esp. protoplasmatic forms. LOH 1p/19q testing required.
- SEGA - esp. gemistocytic forms.
- Diffuse glioma, MYB- or MYBL1-altered.
For CNS grade 3 tumours:
- Anaplastic Oligodendroglioma, when LOH 1p/19q is present.
For CNS grade 4 tumours:
- Glioblastoma - vascular proliferations and / or necrosis.
Outdated terminologies
- Diffuse astrocytoma
- Gemistocytic astrocytoma
- Diffuse astrocytoma, IDH-wildtype
- Glioblastoma; IDH-mutant
- Fibrillary astrocytoma (ICD-O: 9420/3)
- Protoplasmatic astrocytoma (ICD-O:9410/3)
See also
- ↑ Reuss, DE.; Kratz, A.; Sahm, F.; Capper, D.; Schrimpf, D.; Koelsche, C.; Hovestadt, V.; Bewerunge-Hudler, M. et al. (Sep 2015). "Adult IDH wild type astrocytomas biologically and clinically resolve into other tumor entities.". Acta Neuropathol 130 (3): 407-17. doi:10.1007/s00401-015-1454-8. PMID 26087904.
- ↑ Hasselblatt, M.; Jaber, M.; Reuss, D.; Grauer, O.; Bibo, A.; Terwey, S.; Schick, U.; Ebel, H. et al. (Feb 2018). "Diffuse Astrocytoma, IDH-Wildtype: A Dissolving Diagnosis.". J Neuropathol Exp Neurol. doi:10.1093/jnen/nly012. PMID 29444314.
- ↑ Louis, DN.; Perry, A.; Reifenberger, G.; von Deimling, A.; Figarella-Branger, D.; Cavenee, WK.; Ohgaki, H.; Wiestler, OD. et al. (Jun 2016). "The 2016 World Health Organization Classification of Tumors of the Central Nervous System: a summary.". Acta Neuropathol 131 (6): 803-20. doi:10.1007/s00401-016-1545-1. PMID 27157931.
- ↑ Ohgaki, H.; Kleihues, P. (Jun 2005). "Population-based studies on incidence, survival rates, and genetic alterations in astrocytic and oligodendroglial gliomas.". J Neuropathol Exp Neurol 64 (6): 479-89. PMID 15977639.
- ↑ Reuss, DE.; Mamatjan, Y.; Schrimpf, D.; Capper, D.; Hovestadt, V.; Kratz, A.; Sahm, F.; Koelsche, C. et al. (Jun 2015). "IDH mutant diffuse and anaplastic astrocytomas have similar age at presentation and little difference in survival: a grading problem for WHO.". Acta Neuropathol 129 (6): 867-73. doi:10.1007/s00401-015-1438-8. PMID 25962792.
- ↑ 6.0 6.1 Burger, P.C.; Scheithauer, B.W. (2007). Tumors of the Central Nervous System (Afip Atlas of Tumor Pathology) (4th ed.). Washington: American Registry of Pathology. pp. 34. ISBN 1933477016.
- ↑ Shirahata, M.; Ono, T.; Stichel, D.; Schrimpf, D.; Reuss, DE.; Sahm, F.; Koelsche, C.; Wefers, A. et al. (Jul 2018). "Novel, improved grading system(s) for IDH-mutant astrocytic gliomas.". Acta Neuropathol 136 (1): 153-166. doi:10.1007/s00401-018-1849-4. PMID 29687258.
- ↑ Aoki, K.; Nakamura, H.; Suzuki, H.; Matsuo, K.; Kataoka, K.; Shimamura, T.; Motomura, K.; Ohka, F. et al. (01 2018). "Prognostic relevance of genetic alterations in diffuse lower-grade gliomas.". Neuro Oncol 20 (1): 66-77. doi:10.1093/neuonc/nox132. PMID 29016839.
- ↑ Lee, Y.; Koh, J.; Kim, SI.; Won, JK.; Park, CK.; Choi, SH.; Park, SH. (Aug 2017). "The frequency and prognostic effect of TERT promoter mutation in diffuse gliomas.". Acta Neuropathol Commun 5 (1): 62. doi:10.1186/s40478-017-0465-1. PMID 28851427.
- ↑ Koelsche, C.; Sahm, F.; Capper, D.; Reuss, D.; Sturm, D.; Jones, DT.; Kool, M.; Northcott, PA. et al. (Dec 2013). "Distribution of TERT promoter mutations in pediatric and adult tumors of the nervous system.". Acta Neuropathol 126 (6): 907-15. doi:10.1007/s00401-013-1195-5. PMID 24154961.