Difference between revisions of "Parathyroid carcinoma"
Jump to navigation
Jump to search
(+infobox) |
m |
||
| (15 intermediate revisions by the same user not shown) | |||
| Line 1: | Line 1: | ||
{{ Infobox diagnosis | {{ Infobox diagnosis | ||
| Name = {{PAGENAME}} | | Name = {{PAGENAME}} | ||
| Image = | | Image = Parathyroid carcinoma - 1 -- high mag.jpg | ||
| Width = | | Width = | ||
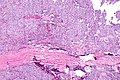
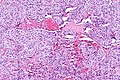
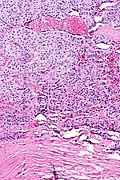
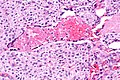
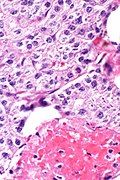
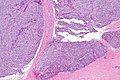
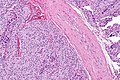
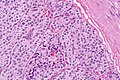
| Caption = | | Caption = Parathyroid carcinoma. [[H&E stain]]. | ||
| Synonyms = | | Synonyms = | ||
| Micro = | | Micro = vascular invasion, local invasion, metastases; nuclear atypia ''not'' diagnostic | ||
| Subtypes = | | Subtypes = | ||
| LMDDx = | | LMDDx = [[parathyroid adenoma]], [[parathyroid hyperplasia]], thyroid lesions | ||
| Stains = | | Stains = | ||
| IHC = | | IHC = [[PAX8]] +ve, Ki-67 >6% +ve, [[GATA3]] +ve, parafibromin -ve | ||
| EM = | | EM = | ||
| Molecular = | | Molecular = +/-HRPT2 gene mutations | ||
| IF = | | IF = | ||
| Gross = | | Gross = | ||
| Line 18: | Line 18: | ||
| Site = [[parathyroid gland]] | | Site = [[parathyroid gland]] | ||
| Assdx = | | Assdx = | ||
| Syndromes = | | Syndromes = familial primary hyperparathyroidism | ||
| Clinicalhx = | | Clinicalhx = | ||
| Signs = | | Signs = | ||
| Line 35: | Line 35: | ||
==General== | ==General== | ||
*Extremely rare. | *Extremely rare. | ||
*May be seen in the context of ''familial primary hyperparathyroidism'' (PHPT).<ref name=pmid28949121>{{Cite journal | last1 = Cetani | first1 = F. | last2 = Pardi | first2 = E. | last3 = Marcocci | first3 = C. | title = Parathyroid carcinoma: a clinical and genetic perspective. | journal = Minerva Endocrinol | volume = 43 | issue = 2 | pages = 144-155 | month = Jun | year = 2018 | doi = 10.23736/S0391-1977.17.02737-7 | PMID = 28949121 }}</ref> | |||
==Microscopic== | ==Microscopic== | ||
| Line 44: | Line 45: | ||
*+/-[[Metastasis]] - '''diagnostic feature'''. | *+/-[[Metastasis]] - '''diagnostic feature'''. | ||
DDx: | |||
* | *[[Parathyroid adenoma]]. | ||
*[[Parathyroid hyperplasia]]. | |||
*[[Poorly differentiated thyroid carcinoma]] and other thyroid cancers. | |||
===Images=== | ===Images=== | ||
| Line 69: | Line 72: | ||
*Ki-67 >6% of cells positive - supports diagnosis.<ref name=pmid7860042>{{Cite journal | last1 = Abbona | first1 = GC. | last2 = Papotti | first2 = M. | last3 = Gasparri | first3 = G. | last4 = Bussolati | first4 = G. | title = Proliferative activity in parathyroid tumors as detected by Ki-67 immunostaining. | journal = Hum Pathol | volume = 26 | issue = 2 | pages = 135-8 | month = Feb | year = 1995 | doi = | PMID = 7860042 }}</ref> | *Ki-67 >6% of cells positive - supports diagnosis.<ref name=pmid7860042>{{Cite journal | last1 = Abbona | first1 = GC. | last2 = Papotti | first2 = M. | last3 = Gasparri | first3 = G. | last4 = Bussolati | first4 = G. | title = Proliferative activity in parathyroid tumors as detected by Ki-67 immunostaining. | journal = Hum Pathol | volume = 26 | issue = 2 | pages = 135-8 | month = Feb | year = 1995 | doi = | PMID = 7860042 }}</ref> | ||
**Parathyroid adenomas and hyperplasias ~ 3%. | **Parathyroid adenomas and hyperplasias ~ 3%. | ||
*[[PAX8]] +ve.<ref name=pmid22498579>{{Cite journal | last1 = Ordóñez | first1 = NG. | title = Value of PAX 8 immunostaining in tumor diagnosis: a review and update. | journal = Adv Anat Pathol | volume = 19 | issue = 3 | pages = 140-51 | month = May | year = 2012 | doi = 10.1097/PAP.0b013e318253465d | PMID = 22498579 }}</ref> | |||
*GATA3 +ve.<ref>{{cite journal |authors=Ordóñez NG |title=Value of GATA3 immunostaining in the diagnosis of parathyroid tumors |journal=Appl Immunohistochem Mol Morphol |volume=22 |issue=10 |pages=756–61 |date=2014 |pmid=25046229 |doi=10.1097/PAI.0000000000000007 |url=}}</ref> | |||
*Parafibromin -ve.<ref name=pmid15475453>{{cite journal |authors=Tan MH, Morrison C, Wang P, Yang X, Haven CJ, Zhang C, Zhao P, Tretiakova MS, Korpi-Hyovalti E, Burgess JR, Soo KC, Cheah WK, Cao B, Resau J, Morreau H, Teh BT |title=Loss of parafibromin immunoreactivity is a distinguishing feature of parathyroid carcinoma |journal=Clin Cancer Res |volume=10 |issue=19 |pages=6629–37 |date=October 2004 |pmid=15475453 |doi=10.1158/1078-0432.CCR-04-0493 |url=}}</ref> | |||
==Molecular== | |||
*HRPT2 gene mutations (10 of 15 sporadic cases of parathyroid carcinoma).<ref name=pmid14585940>{{cite journal |authors=Shattuck TM, Välimäki S, Obara T, Gaz RD, Clark OH, Shoback D, Wierman ME, Tojo K, Robbins CM, Carpten JD, Farnebo LO, Larsson C, Arnold A |title=Somatic and germ-line mutations of the HRPT2 gene in sporadic parathyroid carcinoma |journal=N Engl J Med |volume=349 |issue=18 |pages=1722–9 |date=October 2003 |pmid=14585940 |doi=10.1056/NEJMoa031237 |url=}}</ref> | |||
Note: | |||
*The HRPT2 gene encodes the parafibromin protein.<ref name=pmid14585940/> | |||
==See also== | ==See also== | ||
Latest revision as of 22:28, 9 October 2021
| Parathyroid carcinoma | |
|---|---|
| Diagnosis in short | |
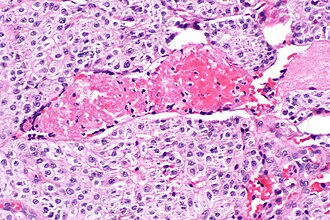 Parathyroid carcinoma. H&E stain. | |
|
| |
| LM | vascular invasion, local invasion, metastases; nuclear atypia not diagnostic |
| LM DDx | parathyroid adenoma, parathyroid hyperplasia, thyroid lesions |
| IHC | PAX8 +ve, Ki-67 >6% +ve, GATA3 +ve, parafibromin -ve |
| Molecular | +/-HRPT2 gene mutations |
| Site | parathyroid gland |
|
| |
| Syndromes | familial primary hyperparathyroidism |
|
| |
| Prevalence | very rare |
| Prognosis | poor |
| Clin. DDx | parathyroid adenoma, parathyroid hyperplasia, thyroid cancer |
| Treatment | surgical excision |
Parathyroid carcinoma is a rare epithelial malignancy of the parathyroid gland.
General
- Extremely rare.
- May be seen in the context of familial primary hyperparathyroidism (PHPT).[1]
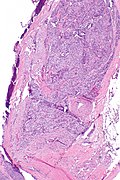
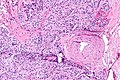
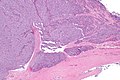
Microscopic
Features:[2]
- Histologically normal parathyroid cells.
- Cytologic features not reliable for diagnosis.
- Fibrous capsule.
- Invasion of surrounding tissue - key feature.
- +/-Metastasis - diagnostic feature.
DDx:
- Parathyroid adenoma.
- Parathyroid hyperplasia.
- Poorly differentiated thyroid carcinoma and other thyroid cancers.
Images
IHC
- Ki-67 >6% of cells positive - supports diagnosis.[3]
- Parathyroid adenomas and hyperplasias ~ 3%.
- PAX8 +ve.[4]
- GATA3 +ve.[5]
- Parafibromin -ve.[6]
Molecular
- HRPT2 gene mutations (10 of 15 sporadic cases of parathyroid carcinoma).[7]
Note:
- The HRPT2 gene encodes the parafibromin protein.[7]
See also
References
- ↑ Cetani, F.; Pardi, E.; Marcocci, C. (Jun 2018). "Parathyroid carcinoma: a clinical and genetic perspective.". Minerva Endocrinol 43 (2): 144-155. doi:10.23736/S0391-1977.17.02737-7. PMID 28949121.
- ↑ Kumar, Vinay; Abbas, Abul K.; Fausto, Nelson; Aster, Jon (2009). Robbins and Cotran pathologic basis of disease (8th ed.). Elsevier Saunders. pp. 1128. ISBN 978-1416031215.
- ↑ Abbona, GC.; Papotti, M.; Gasparri, G.; Bussolati, G. (Feb 1995). "Proliferative activity in parathyroid tumors as detected by Ki-67 immunostaining.". Hum Pathol 26 (2): 135-8. PMID 7860042.
- ↑ Ordóñez, NG. (May 2012). "Value of PAX 8 immunostaining in tumor diagnosis: a review and update.". Adv Anat Pathol 19 (3): 140-51. doi:10.1097/PAP.0b013e318253465d. PMID 22498579.
- ↑ Ordóñez NG (2014). "Value of GATA3 immunostaining in the diagnosis of parathyroid tumors". Appl Immunohistochem Mol Morphol 22 (10): 756–61. doi:10.1097/PAI.0000000000000007. PMID 25046229.
- ↑ Tan MH, Morrison C, Wang P, Yang X, Haven CJ, Zhang C, Zhao P, Tretiakova MS, Korpi-Hyovalti E, Burgess JR, Soo KC, Cheah WK, Cao B, Resau J, Morreau H, Teh BT (October 2004). "Loss of parafibromin immunoreactivity is a distinguishing feature of parathyroid carcinoma". Clin Cancer Res 10 (19): 6629–37. doi:10.1158/1078-0432.CCR-04-0493. PMID 15475453.
- ↑ 7.0 7.1 Shattuck TM, Välimäki S, Obara T, Gaz RD, Clark OH, Shoback D, Wierman ME, Tojo K, Robbins CM, Carpten JD, Farnebo LO, Larsson C, Arnold A (October 2003). "Somatic and germ-line mutations of the HRPT2 gene in sporadic parathyroid carcinoma". N Engl J Med 349 (18): 1722–9. doi:10.1056/NEJMoa031237. PMID 14585940.