Difference between revisions of "Tumour budding"
Jump to navigation
Jump to search
| (5 intermediate revisions by the same user not shown) | |||
| Line 16: | Line 16: | ||
Note: | Note: | ||
*Assessed in a field area of 0.785 mm<sup>2</sup>.<ref name=pmid28548122/> | *Assessed in a field area of 0.785 mm<sup>2</sup>.<ref name=pmid28548122/> | ||
**Microscopes with a 22 mm eye pieces typically have a 0.2376 mm*mm field area with the 40x objective; thus, three fields is 0.7128 mm*mm. | |||
**Tumour budding was '''previously''' assessed in a field of 0.385 mm<sup>2</sup>.<ref name=pmid11952856>{{Cite journal | last1 = Ueno | first1 = H. | last2 = Murphy | first2 = J. | last3 = Jass | first3 = JR. | last4 = Mochizuki | first4 = H. | last5 = Talbot | first5 = IC. | title = Tumour 'budding' as an index to estimate the potential of aggressiveness in rectal cancer. | journal = Histopathology | volume = 40 | issue = 2 | pages = 127-32 | month = Feb | year = 2002 | doi = | PMID = 11952856 }}</ref> | **Tumour budding was '''previously''' assessed in a field of 0.385 mm<sup>2</sup>.<ref name=pmid11952856>{{Cite journal | last1 = Ueno | first1 = H. | last2 = Murphy | first2 = J. | last3 = Jass | first3 = JR. | last4 = Mochizuki | first4 = H. | last5 = Talbot | first5 = IC. | title = Tumour 'budding' as an index to estimate the potential of aggressiveness in rectal cancer. | journal = Histopathology | volume = 40 | issue = 2 | pages = 127-32 | month = Feb | year = 2002 | doi = | PMID = 11952856 }}</ref> | ||
*"Tumour buds suspended in pools of mucin should not be counted" as per the consensus.<ref name=pmid28548122/> | |||
DDx: | DDx: | ||
| Line 27: | Line 29: | ||
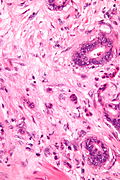
Image: Tumour budding in colorectal carcinoma - very high mag.jpg | Tumour budding in CRC - very high mag. (WC) | Image: Tumour budding in colorectal carcinoma - very high mag.jpg | Tumour budding in CRC - very high mag. (WC) | ||
</gallery> | </gallery> | ||
== Sign out == | |||
<pre> | |||
There are <5 tumour buds/0.785 mm*mm; this tumour has low grade tumour budding. | |||
</pre> | |||
<pre> | |||
There are 5-9 tumour buds/0.785 mm*mm; this tumour has intermediate grade tumour budding. | |||
</pre> | |||
<pre> | |||
There are >=10 tumour buds/0.785 mm*mm; this tumour has high grade tumour budding. | |||
</pre> | |||
===Alternate=== | |||
<pre> | |||
The tumour is NEGATIVE for significant tumour budding (<5 buds/0.785 mm*mm). | |||
</pre> | |||
==See also== | ==See also== | ||
| Line 32: | Line 49: | ||
*[[In-transit metastasis]]. | *[[In-transit metastasis]]. | ||
*[[Tumour deposits]]. | *[[Tumour deposits]]. | ||
*[[Worst pattern of invasion]]. | |||
*[[Spread through air spaces]]. | |||
==References== | ==References== | ||
Latest revision as of 15:50, 25 August 2023
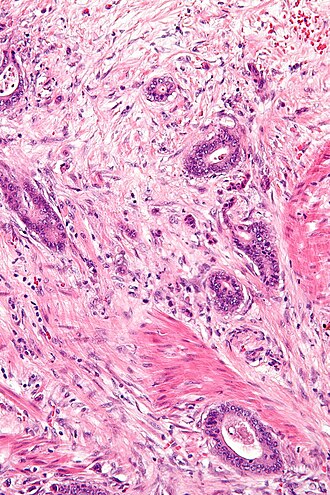
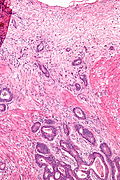
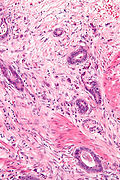
Tumour budding refers to lone tumour cells or small clusters of tumour cells at the advancing front of a tumour.[1]
General
- Poor prognosticator in colorectal carcinoma,[2] and invasive ductal carcinoma of the breast.[3]
Microscopic
Definition in rectal carcinoma - based on international consensus:[4]
- Tumour bud = 1-4 cell(s) -- at the tumour front.
Grading:
- Low grade: 0-4 tumour buds.
- Intermediate grade: 5-9 tumour buds.
- High grade: >=10 tumour buds.
Note:
- Assessed in a field area of 0.785 mm2.[4]
- Microscopes with a 22 mm eye pieces typically have a 0.2376 mm*mm field area with the 40x objective; thus, three fields is 0.7128 mm*mm.
- Tumour budding was previously assessed in a field of 0.385 mm2.[1]
- "Tumour buds suspended in pools of mucin should not be counted" as per the consensus.[4]
DDx:
- Poorly differentiated adenocarcinoma.
Images
Tumour budding in CRC - intermed. mag. (WC)
Sign out
There are <5 tumour buds/0.785 mm*mm; this tumour has low grade tumour budding.
There are 5-9 tumour buds/0.785 mm*mm; this tumour has intermediate grade tumour budding.
There are >=10 tumour buds/0.785 mm*mm; this tumour has high grade tumour budding.
Alternate
The tumour is NEGATIVE for significant tumour budding (<5 buds/0.785 mm*mm).
See also
- High risk features in colorectal adenomatous polyps.
- In-transit metastasis.
- Tumour deposits.
- Worst pattern of invasion.
- Spread through air spaces.
References
- ↑ 1.0 1.1 Ueno, H.; Murphy, J.; Jass, JR.; Mochizuki, H.; Talbot, IC. (Feb 2002). "Tumour 'budding' as an index to estimate the potential of aggressiveness in rectal cancer.". Histopathology 40 (2): 127-32. PMID 11952856.
- ↑ Mitrovic, B.; Schaeffer, DF.; Riddell, RH.; Kirsch, R. (Oct 2012). "Tumor budding in colorectal carcinoma: time to take notice.". Mod Pathol 25 (10): 1315-25. doi:10.1038/modpathol.2012.94. PMID 22790014.
- ↑ Gujam, FJ.; McMillan, DC.; Mohammed, ZM.; Edwards, J.; Going, JJ. (Sep 2015). "The relationship between tumour budding, the tumour microenvironment and survival in patients with invasive ductal breast cancer.". Br J Cancer 113 (7): 1066-74. doi:10.1038/bjc.2015.287. PMID 26263482.
- ↑ 4.0 4.1 4.2 Lugli, A.; Kirsch, R.; Ajioka, Y.; Bosman, F.; Cathomas, G.; Dawson, H.; El Zimaity, H.; Fléjou, JF. et al. (Sep 2017). "Recommendations for reporting tumor budding in colorectal cancer based on the International Tumor Budding Consensus Conference (ITBCC) 2016.". Mod Pathol 30 (9): 1299-1311. doi:10.1038/modpathol.2017.46. PMID 28548122.