Difference between revisions of "Pseudomelanosis coli"
Jump to navigation
Jump to search
(→General: wikify) |
|||
| (One intermediate revision by the same user not shown) | |||
| Line 4: | Line 4: | ||
| Width = | | Width = | ||
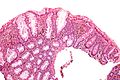
| Caption = Pseudomelanosis coli. [[H&E stain]]. | | Caption = Pseudomelanosis coli. [[H&E stain]]. | ||
| Synonyms = melanosis coli | |||
| Micro = brown granular pigment in the lamina propria, abundant | | Micro = brown granular pigment in the lamina propria, abundant | ||
| Subtypes = | | Subtypes = | ||
| Line 39: | Line 40: | ||
==General== | ==General== | ||
*''Not melanin'' as the name ''melanosis coli'' suggests; it is actually lipofuscin (in macrophages).<ref name=pmid18666316>{{cite journal |author=Freeman HJ |title="Melanosis" in the small and large intestine |journal=World J. Gastroenterol. |volume=14 |issue=27 |pages=4296-9 |year=2008 |month=July |pmid=18666316 |doi= |url=http://www.wjgnet.com/1007-9327/14/4296.asp}}</ref> | *''Not melanin'' as the name ''melanosis coli'' suggests; it is actually [[lipofuscin]] (in macrophages).<ref name=pmid18666316>{{cite journal |author=Freeman HJ |title="Melanosis" in the small and large intestine |journal=World J. Gastroenterol. |volume=14 |issue=27 |pages=4296-9 |year=2008 |month=July |pmid=18666316 |doi= |url=http://www.wjgnet.com/1007-9327/14/4296.asp}}</ref> | ||
*Endoscopist may see brown pigmentation of mucosa and suspect the diagnosis. | *Endoscopist may see brown pigmentation of mucosa and suspect the diagnosis. | ||
*Presence may lead to endoscopic misinterpretation of colitis severity.<ref name=pmid21375218>{{Cite journal | last1 = Zapatier | first1 = JA. | last2 = Schneider | first2 = A. | last3 = Parra | first3 = JL. | title = Overestimation of ulcerative colitis due to melanosis coli. | journal = Acta Gastroenterol Latinoam | volume = 40 | issue = 4 | pages = 351-3 | month = Dec | year = 2010 | doi = | PMID = 21375218 }}</ref> | *Presence may lead to endoscopic misinterpretation of colitis severity.<ref name=pmid21375218>{{Cite journal | last1 = Zapatier | first1 = JA. | last2 = Schneider | first2 = A. | last3 = Parra | first3 = JL. | title = Overestimation of ulcerative colitis due to melanosis coli. | journal = Acta Gastroenterol Latinoam | volume = 40 | issue = 4 | pages = 351-3 | month = Dec | year = 2010 | doi = | PMID = 21375218 }}</ref> | ||
Latest revision as of 18:08, 24 May 2020
| Pseudomelanosis coli | |
|---|---|
| Diagnosis in short | |
 Pseudomelanosis coli. H&E stain. | |
|
| |
| Synonyms | melanosis coli |
|
| |
| LM | brown granular pigment in the lamina propria, abundant |
| LM DDx | hemorrhage, melanocytic lesion (rarely) |
| Stains | PAS +ve, Prussian blue -ve, Fontana-Masson +ve |
| Site | colon, cecum, occasionally small intestine |
|
| |
| Clinical history | use of laxatives and herbals |
| Endoscopy | brown discolouration of the mucosa, esp. proximal colon and cecum |
| Prognosis | benign |
| Clin. DDx | colitis |
| Pseudomelanosis coli | |
|---|---|
| External resources | |
| Wikipedia | melanosis coli |
Pseudomelanosis coli, also known as melanosis coli,[1] is a relatively common benign change seen in the colon.
General
- Not melanin as the name melanosis coli suggests; it is actually lipofuscin (in macrophages).[2]
- Endoscopist may see brown pigmentation of mucosa and suspect the diagnosis.
- Presence may lead to endoscopic misinterpretation of colitis severity.[3]
Epidemiology
- Classically associated with anthracene containing laxative (e.g. Senokot) use and herbal remedies.[2]
- May be seen in individuals not using laxatives.[4]
- Seen in (long-standing) inflammatory bowel disease, especially ulcerative colitis.[4]
Gross
- Brown pigmentation of the mucosa, especially cecum and proximal colon.[2]
- Less pigmentation distal.
Note:
- May also been seen in the small intestine.[2]
Endoscopic image
Microscopic
Features:
- Brown granular pigment - in the lamina propria.
- Typically more prominent in the cecum and proximal colon.[2]
Notes:
- DDx of brown pigment:
- Lipofuscin - comes with age (can be demonstrated with a PAS stain[5] or Kluver-Barrera stain[6]).
- Melanosis coli.
- Old haemorrhage, i.e. hemosiderin-laden macrophages (may be demonstrated with Prussian blue stain[7]).
- Melanin (from melanocytes) - rare in colon (may be demonstrated with a Fontana-Masson stain[8]).
- Fontana-Masson not useful for differentiating from pseudomelanosis, as pseudomelanosis is Fontana-Masson positive.[9]
- Foreign material (e.g. tattoo pigment) - not seen in GI tract.
- Lipofuscin - comes with age (can be demonstrated with a PAS stain[5] or Kluver-Barrera stain[6]).
Images
Another case:
Stains
Note:
- Fontana-Masson stain is not useful for differentiating pseudomelanosis from true melanin pigment, as pseudomelanosis is Fontana-Masson positive.[9]
Sign out
ASCENDING COLON, BIOPSY: - PSEUDOMELANOSIS COLI. - NEGATIVE FOR ACTIVE COLITIS. - NEGATIVE FOR DYSPLASIA.
See also
References
- ↑ URL: http://www.medicinenet.com/melanosis_coli/article.htm. Accessed on: 4 March 2011.
- ↑ 2.0 2.1 2.2 2.3 2.4 Freeman HJ (July 2008). ""Melanosis" in the small and large intestine". World J. Gastroenterol. 14 (27): 4296-9. PMID 18666316. http://www.wjgnet.com/1007-9327/14/4296.asp.
- ↑ Zapatier, JA.; Schneider, A.; Parra, JL. (Dec 2010). "Overestimation of ulcerative colitis due to melanosis coli.". Acta Gastroenterol Latinoam 40 (4): 351-3. PMID 21375218.
- ↑ 4.0 4.1 Pardi, DS.; Tremaine, WJ.; Rothenberg, HJ.; Batts, KP. (Apr 1998). "Melanosis coli in inflammatory bowel disease.". J Clin Gastroenterol 26 (3): 167-70. PMID 9600362.
- ↑ Kovi J, Leifer C (July 1970). "Lipofuscin pigment accumulation in spontaneous mammary carcinoma of A/Jax mouse". J Natl Med Assoc 62 (4): 287–90. PMC 2611776. PMID 5463681. http://www.ncbi.nlm.nih.gov/pmc/articles/PMC2611776/pdf/jnma00512-0077.pdf.
- ↑ URL: http://education.vetmed.vt.edu/curriculum/VM8054/labs/Lab2/Examples/exkluvbarr.htm. Accessed on: 5 May 2010.
- ↑ URL: http://education.vetmed.vt.edu/curriculum/VM8054/labs/Lab2/Examples/exprussb.htm. Accessed on: 5 May 2010.
- ↑ URL: http://education.vetmed.vt.edu/curriculum/VM8054/labs/Lab2/Examples/exfontana.htm. Accessed on: 5 May 2010.
- ↑ 9.0 9.1 Park, C.; Cho, NH.; Jeong, HJ. (Mar 1990). "Melanosis coli--histochemical and immunohistochemical comparison of the pigments of melanosis coli and Dubin-Johnson syndrome.". Yonsei Med J 31 (1): 27-32. PMID 2346038.
- ↑ Benavides SH, Morgante PE, Monserrat AJ, Zárate J, Porta EA (August 1997). "The pigment of melanosis coli: a lectin histochemical study". Gastrointest. Endosc. 46 (2): 131–8. PMID 9283862.