Difference between revisions of "Parathyroid hyperplasia"
Jump to navigation
Jump to search
| (21 intermediate revisions by the same user not shown) | |||
| Line 1: | Line 1: | ||
'''Parathyroid hyperplasia''' is a common cause of [[hyperparathyroidism]] that is | {{ Infobox diagnosis | ||
| Name = {{PAGENAME}} | |||
| Image = Parathyroid hyperplasia -- intermed mag.jpg | |||
| Width = | |||
| Caption = Parathyroid hyperplasia. [[H&E stain]]. | |||
| Synonyms = | |||
| Micro = hypercellular - usu. chief cell predominant, decreased adipose tissue, +/-"water-clear" cells (cells with abundant granular/foamy cytoplasm, mild nuclear pleomorphism) | |||
| Subtypes = | |||
| LMDDx = [[parathyroid adenoma]], [[parathyroid carcinoma]] | |||
| Stains = | |||
| IHC = | |||
| EM = | |||
| Molecular = | |||
| IF = | |||
| Gross = all parathyroid glands are enlarged | |||
| Grossing = | |||
| Staging = | |||
| Site = [[parathyroid gland]] | |||
| Assdx = [[chronic renal failure]] | |||
| Syndromes = [[MEN 1]], [[MEN 2A]] | |||
| Clinicalhx = | |||
| Signs = | |||
| Symptoms = | |||
| Prevalence = uncommon | |||
| Bloodwork = elevated PTH, +/-elevated calcium | |||
| Rads = | |||
| Endoscopy = | |||
| Prognosis = | |||
| Other = | |||
| ClinDDx = parathyroid adenoma | |||
| Tx = surgical removal of all parathyroid glands & re-implantation of half of one parathyroid in the forearm | |||
}} | |||
'''Parathyroid hyperplasia''' is an abnormal proliferation of the [[parathyroid gland]]s and a relatively common cause of [[hyperparathyroidism]] that is typically associated with [[chronic renal failure]].<ref name=pmid23267748>{{Cite journal | last1 = Jamal | first1 = SA. | last2 = Miller | first2 = PD. | title = Secondary and tertiary hyperparathyroidism. | journal = J Clin Densitom | volume = 16 | issue = 1 | pages = 64-8 | month = | year = | doi = 10.1016/j.jocd.2012.11.012 | PMID = 23267748 }}</ref> | |||
==General== | ==General== | ||
*Common cause of [[hyperparathyroidism]]. | *Common cause of [[hyperparathyroidism]]. | ||
*Usually associated with [[chronic renal failure]]. | *Usually associated with [[chronic renal failure]]. | ||
*May be syndromic - chief cell hyperplasia - associated with [[MEN 1]], [[MEN 2A]].<ref>URL: [http://www.pathconsultddx.com/pathCon/diagnosis?pii=S1559-8675%2806%2970475-2 http://www.pathconsultddx.com/pathCon/diagnosis?pii=S1559-8675%2806%2970475-2]. Accessed on: 29 July 2010.</ref> | *May be syndromic - chief cell hyperplasia - associated with [[MEN 1]], [[MEN 2A]].<ref>URL: [http://www.pathconsultddx.com/pathCon/diagnosis?pii=S1559-8675%2806%2970475-2 http://www.pathconsultddx.com/pathCon/diagnosis?pii=S1559-8675%2806%2970475-2]. Accessed on: 29 July 2010.</ref> ‡ | ||
Treatment: | |||
*Surgical removal of all parathyroid glands & re-implantation of half of one parathyroid in the forearm. | |||
Note: <br> | |||
‡ MEN 1 and MEN 2A are often described as causing parathyroid hyperplasia; more correctly, it is thought these are actually multiple parathyroid adenomas.<ref name=pmid15490065>{{cite journal |authors=Doherty GM, Lairmore TC, DeBenedetti MK |title=Multiple endocrine neoplasia type 1 parathyroid adenoma development over time |journal=World J Surg |volume=28 |issue=11 |pages=1139–42 |date=November 2004 |pmid=15490065 |doi=10.1007/s00268-004-7560-8 |url=}}</ref> | |||
==Gross== | ==Gross== | ||
* | *Parathyroid gland enlargement - classically all parathyroid glands are involved; however, some may be spared making it difficult to differentiate this from parathyroid adenoma.<ref name=Ref_PBoD8_1128>{{Ref PBoD8|1128}}</ref> | ||
==Microscopic== | ==Microscopic== | ||
Features:<ref name= | Features: | ||
* | *Hyperplastic/hypercellular appearance: | ||
* | **Decreased adipose tissue.<ref name=pmid8090603>{{Cite journal | last1 = Yong | first1 = JL. | last2 = Vrga | first2 = L. | last3 = Warren | first3 = BA. | title = A study of parathyroid hyperplasia in chronic renal failure. | journal = Pathology | volume = 26 | issue = 2 | pages = 99-109 | month = Apr | year = 1994 | doi = | PMID = 8090603 }}</ref> | ||
**Increased parenchymal cells. | |||
***Chief cells - usually predominant.<ref name=pmid8090603/> | |||
***"Water-clear" cells: | |||
****Abundant foamy or granular cytoplasm.<ref name=pmid7487410/> | |||
****Mild [[nuclear pleomorphism]]. | |||
****May not be present or apparent. | |||
***Other parenchymal cells include: oxyphil cells and transitional oxyphil cells. | |||
Note: | Note: | ||
*Generally, it is impossible to discern between [[parathyroid adenoma]]s and | *Generally, it is impossible to discern between [[parathyroid adenoma]]s and parathyroid hyperplasias by histology alone.<ref name=Ref_BITFS191>{{Ref BITFS|191}}</ref> | ||
**One requires information of the size of the other glands to make the diagnosis. | **One requires information of the size of the other glands to make the diagnosis. | ||
*Water-clear cells may be seen in an adenoma.<ref name=pmid7487410>{{Cite journal | last1 = Grenko | first1 = RT. | last2 = Anderson | first2 = KM. | last3 = Kauffman | first3 = G. | last4 = Abt | first4 = AB. | title = Water-clear cell adenoma of the parathyroid. A case report with immunohistochemistry and electron microscopy. | journal = Arch Pathol Lab Med | volume = 119 | issue = 11 | pages = 1072-4 | month = Nov | year = 1995 | doi = | PMID = 7487410 }}</ref> | |||
DDx: | DDx: | ||
*[[Parathyroid adenoma]] - classically have a rim of normal parathyroid gland around it. | *[[Parathyroid adenoma]] - classically have a rim of normal parathyroid gland around it. | ||
*[[Parathyroid carcinoma]] - has invasive tissue destruction or far away metastases. | |||
===Images=== | |||
<gallery> | |||
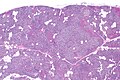
Image: Parathyroid hyperplasia -- very low mag.jpg | PA - very low mag. (WC) | |||
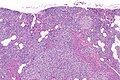
Image: Parathyroid hyperplasia -- low mag.jpg | PA - low mag. (WC) | |||
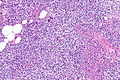
Image: Parathyroid hyperplasia -- intermed mag.jpg | PA - intermed. mag. (WC) | |||
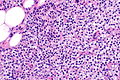
Image: Parathyroid hyperplasia -- high mag.jpg | PA - high mag. (WC) | |||
</gallery> | |||
====www==== | |||
*[https://www.flickr.com/photos/jian-hua_qiao_md/13138532173 Water clear cells in hyperplasia (flicker.com)]. | |||
==Sign out== | ==Sign out== | ||
===Clinical history is suggestive=== | |||
<pre> | <pre> | ||
A. Right Superior Parathyroid, Excision: | A. Right Superior Parathyroid, Excision: | ||
Latest revision as of 21:53, 6 April 2022
| Parathyroid hyperplasia | |
|---|---|
| Diagnosis in short | |
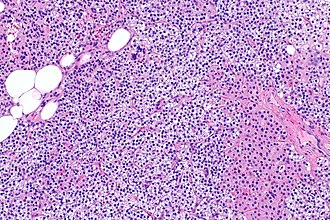 Parathyroid hyperplasia. H&E stain. | |
|
| |
| LM | hypercellular - usu. chief cell predominant, decreased adipose tissue, +/-"water-clear" cells (cells with abundant granular/foamy cytoplasm, mild nuclear pleomorphism) |
| LM DDx | parathyroid adenoma, parathyroid carcinoma |
| Gross | all parathyroid glands are enlarged |
| Site | parathyroid gland |
|
| |
| Associated Dx | chronic renal failure |
| Syndromes | MEN 1, MEN 2A |
|
| |
| Prevalence | uncommon |
| Blood work | elevated PTH, +/-elevated calcium |
| Clin. DDx | parathyroid adenoma |
| Treatment | surgical removal of all parathyroid glands & re-implantation of half of one parathyroid in the forearm |
Parathyroid hyperplasia is an abnormal proliferation of the parathyroid glands and a relatively common cause of hyperparathyroidism that is typically associated with chronic renal failure.[1]
General
- Common cause of hyperparathyroidism.
- Usually associated with chronic renal failure.
- May be syndromic - chief cell hyperplasia - associated with MEN 1, MEN 2A.[2] ‡
Treatment:
- Surgical removal of all parathyroid glands & re-implantation of half of one parathyroid in the forearm.
Note:
‡ MEN 1 and MEN 2A are often described as causing parathyroid hyperplasia; more correctly, it is thought these are actually multiple parathyroid adenomas.[3]
Gross
- Parathyroid gland enlargement - classically all parathyroid glands are involved; however, some may be spared making it difficult to differentiate this from parathyroid adenoma.[4]
Microscopic
Features:
- Hyperplastic/hypercellular appearance:
- Decreased adipose tissue.[5]
- Increased parenchymal cells.
- Chief cells - usually predominant.[5]
- "Water-clear" cells:
- Abundant foamy or granular cytoplasm.[6]
- Mild nuclear pleomorphism.
- May not be present or apparent.
- Other parenchymal cells include: oxyphil cells and transitional oxyphil cells.
Note:
- Generally, it is impossible to discern between parathyroid adenomas and parathyroid hyperplasias by histology alone.[7]
- One requires information of the size of the other glands to make the diagnosis.
- Water-clear cells may be seen in an adenoma.[6]
DDx:
- Parathyroid adenoma - classically have a rim of normal parathyroid gland around it.
- Parathyroid carcinoma - has invasive tissue destruction or far away metastases.
Images
www
Sign out
Clinical history is suggestive
A. Right Superior Parathyroid, Excision: - Parathyroid tissue compatible with hyperplasia. B. Right Inferior Parathyroid, Excision: - Parathyroid tissue compatible with hyperplasia. C. Portion of Left Inferior Parathyroid, Excision: - Parathyroid tissue compatible with hyperplasia. D. Left Superior Parathyroid, Excision: - Parathyroid tissue compatible with hyperplasia.
See also
References
- ↑ Jamal, SA.; Miller, PD.. "Secondary and tertiary hyperparathyroidism.". J Clin Densitom 16 (1): 64-8. doi:10.1016/j.jocd.2012.11.012. PMID 23267748.
- ↑ URL: http://www.pathconsultddx.com/pathCon/diagnosis?pii=S1559-8675%2806%2970475-2. Accessed on: 29 July 2010.
- ↑ Doherty GM, Lairmore TC, DeBenedetti MK (November 2004). "Multiple endocrine neoplasia type 1 parathyroid adenoma development over time". World J Surg 28 (11): 1139–42. doi:10.1007/s00268-004-7560-8. PMID 15490065.
- ↑ Kumar, Vinay; Abbas, Abul K.; Fausto, Nelson; Aster, Jon (2009). Robbins and Cotran pathologic basis of disease (8th ed.). Elsevier Saunders. pp. 1128. ISBN 978-1416031215.
- ↑ 5.0 5.1 Yong, JL.; Vrga, L.; Warren, BA. (Apr 1994). "A study of parathyroid hyperplasia in chronic renal failure.". Pathology 26 (2): 99-109. PMID 8090603.
- ↑ 6.0 6.1 Grenko, RT.; Anderson, KM.; Kauffman, G.; Abt, AB. (Nov 1995). "Water-clear cell adenoma of the parathyroid. A case report with immunohistochemistry and electron microscopy.". Arch Pathol Lab Med 119 (11): 1072-4. PMID 7487410.
- ↑ Taxy, J.; Husain, A; Montag, A. (2009). Biopsy Interpretation: The Frozen Section (1st ed.). Lippincott Williams & Wilkins. pp. 191. ISBN 978-0781767798.