Difference between revisions of "CSF cytopathology"
Jump to navigation
Jump to search
Jensflorian (talk | contribs) (→Meningeosis carcinomatosa: english term added to latin description) |
|||
| (13 intermediate revisions by 3 users not shown) | |||
| Line 8: | Line 8: | ||
#Lymphoma is a common malignancy of malignancies found in the CSF. | #Lymphoma is a common malignancy of malignancies found in the CSF. | ||
In many institutions, all CSF specimens are ''stat''. | In many institutions, all CSF specimens are ''stat''. ''Lumbar puncture'' redirects here. | ||
==Cerebrospinal fluid== | ==Cerebrospinal fluid== | ||
==Normal== | ==Normal== | ||
*Paucicellular. | *Paucicellular. | ||
*< | **Acellular specimens common and considered adequate.<ref>{{cite book |author=Mody, Dina R. |title= [https://www.amazon.ca/Diagnostic-Pathology-Cytopathology-Dina-Mody/dp/1931884552/ Diagnostic Cytopathology] |publisher=Elsevier Canada |location= |year=2018 |pages= {{{1|II-3 2}}} |edition=1st |isbn=978-1931884556 |oclc= |doi= |accessdate=}}</ref> | ||
*protein is around 15-40 mg/dl. | |||
Gobs of anuclear material: | Gobs of anuclear material: | ||
*Protein vs. white | *Protein vs. white matter. | ||
*Ocassionally arachnoid cap cell- | |||
Bark-like flaky material: | Bark-like flaky material: | ||
| Line 35: | Line 37: | ||
==Hemorrhage== | ==Hemorrhage== | ||
*Xanthochromatous specimen | *Xanthochromatous specimen | ||
**Can be artificial -> due punctuation. | **Can be artificial -> due punctuation injuries or rifampin medication.<ref name="pmid7125611">{{Cite journal | last1 = Liggett | first1 = SB. | last2 = Berger | first2 = JR. | last3 = Hush | first3 = J. | title = Cerebrospinal fluid xanthochromia with rifampin. | journal = Ann Neurol | volume = 12 | issue = 2 | pages = 228-9 | month = Aug | year = 1982 | doi = 10.1002/ana.410120240 | PMID = 7125611 }}</ref> | ||
**Can be seen in newborn -> due to increased bilirubin levels. | |||
**Best seen when looking from top through the tube. <ref name="pmid3981778">{{Cite journal | last1 = Bremer | first1 = HL. | title = Identification of xanthochromia. | journal = JAMA | volume = 253 | issue = 17 | pages = 2496 | month = May | year = 1985 | doi = | PMID = 3981778 }}</ref> | |||
**pink (free hemoglobin directly after bleeding) to yellow (bilirubin after one day). | |||
===Cytology=== | ===Cytology=== | ||
| Line 44: | Line 50: | ||
<gallery> | <gallery> | ||
File:XanthochromeCSF.jpg | Xanthochromatous CSF (WC/Dschafar) | File:XanthochromeCSF.jpg | Xanthochromatous CSF (WC/Dschafar) | ||
File:Siderophage_CSF_cytology.jpg | A siderophage (WC/jensflorian) | |||
</gallery> | </gallery> | ||
| Line 56: | Line 63: | ||
<gallery> | <gallery> | ||
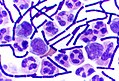
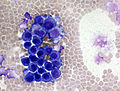
File:CSF_pleocytosis_neutrophils.jpg | CSF (Pappenheim stain) with numerous neutrophils indicating a purulent meningitis (WC/jensflorian) | File:CSF_pleocytosis_neutrophils.jpg | CSF (Pappenheim stain) with numerous neutrophils indicating a purulent meningitis (WC/jensflorian) | ||
File:CSF S capitis 2013-11-08.JPG | Streoptococcal meningitis in a neonate with ventriculoperitoneal shunt (WC/Paulo Henrique Orlandi Mourao) | |||
File:Gram Stain Anthrax.jpg | Gram-positive Anthrax bacteria in a CSF specimen (WC/TenOfAllTrades). | |||
</gallery> | </gallery> | ||
DDx: | |||
*[[TBC]] | |||
*Fungal meningitis | |||
==Viral meningitis== | ==Viral meningitis== | ||
| Line 62: | Line 75: | ||
===General=== | ===General=== | ||
*Positive viral culture. | *Positive viral culture. | ||
**HSV | |||
**CMV | |||
**Enterovirus | |||
**HIV | |||
===Cytology=== | ===Cytology=== | ||
*Pleocytosis (usu. 10-1000 cells/µl). | |||
*Polymorphous population of lymphocytes.<ref name=Ref_APBR681/> | *Polymorphous population of lymphocytes.<ref name=Ref_APBR681/> | ||
* Activated lymphocytes. | |||
* Plasma cells (sometimes bi- and multinuclear). | |||
* Occ. mitoses. | |||
* Activated (vacuolated) monocytes. | |||
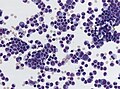
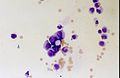
<gallery> | |||
File:Hiv_meningeoencephalitis_csf_pleocytosis.jpg | Lymphocytic plecoytosis in HIV meningeoencephalitis | |||
File:HSV1_encephalitis_CSF_specimen.jpg | Activated lymphocytes in HSV1 encephalitis | |||
</gallery> | |||
==Mollaret's meningitis== | ==Mollaret's meningitis== | ||
| Line 118: | Line 145: | ||
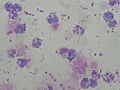
File:Meningeosis carcinomatosa.jpg | Lung adenocarcinoma cells in CSF (WC/Marvin101). | File:Meningeosis carcinomatosa.jpg | Lung adenocarcinoma cells in CSF (WC/Marvin101). | ||
File:Leptomeningeal metastasis.jpg | Atypical mitosis in epithelial cells in CSF (WC/jensflorian). | File:Leptomeningeal metastasis.jpg | Atypical mitosis in epithelial cells in CSF (WC/jensflorian). | ||
File:Meningiosis carcinomatosa.jpg | Leptomeningeal carinomatois (WC/jensflorian). | |||
</gallery> | </gallery> | ||
Latest revision as of 17:38, 26 June 2024
CSF cytopathology is a subset of CNS cytopathology, which is a subset of cytopathology.
This article deal only with cerebrospinal fluid (CSF) cytopathology. An introduction to cytopathology is in the cytopathology article.
In many institutions, CSF specimens get triaged/rapidly assessed as:
- They are small specimens ~ usually 1-10 ml.
- The procedure to obtain them is non-trivial, i.e. not pleasant for the patient and not risk free.
- Lymphoma is a common malignancy of malignancies found in the CSF.
In many institutions, all CSF specimens are stat. Lumbar puncture redirects here.
Cerebrospinal fluid
Normal
- Paucicellular.
- Acellular specimens common and considered adequate.[1]
- protein is around 15-40 mg/dl.
Gobs of anuclear material:
- Protein vs. white matter.
- Ocassionally arachnoid cap cell-
Bark-like flaky material:
- Contaminant.
Fluffy/smudged large cells (~2-3x RBC dia.) with an indistinct nucleus:
- Degenerated white cells.
- Should prompt a comment about "degeneration", if the population is dominant.
Routine processing
- Cytospin - if no abnormality at triage.
- The cellularity of the cytospin will appear to be increased (artifact).
Images
Hemorrhage
- Xanthochromatous specimen
Cytology
- Mostly RBC.
- Neutrophils can be increased.
- +/-Erythro- and Siderophages (usu. after 3-4d).
Acute bacterial meningitis
Main article: Meningitis
Cytology
- Neutrophils - none should be present normally.[4][5]
- If the tap is traumatic (i.e. fibrin is present) the finding may be uninterpretable.
- Neutrophils may be present in early exsudative phase of viral meningitis.
- Cell count usually above 1000/µl.
DDx:
- TBC
- Fungal meningitis
Viral meningitis
Main article: Meningitis
General
- Positive viral culture.
- HSV
- CMV
- Enterovirus
- HIV
Cytology
- Pleocytosis (usu. 10-1000 cells/µl).
- Polymorphous population of lymphocytes.[4]
- Activated lymphocytes.
- Plasma cells (sometimes bi- and multinuclear).
- Occ. mitoses.
- Activated (vacuolated) monocytes.
Mollaret's meningitis
General
- Rare aseptic meningitis.
- Suspected to be caused by HSV1 and HSV2.[6]
Clinical:
- Recurrent meningismus, headache, +/-fever.[6]
Cytology
Features:
- Mollaret cells - described as monocytoid cells[4] (look like monocytes[7] - but do not phagocytose), and large endothelial cells.[6]
- Features - large cells with: abundant cytoplasm, footprint-shaped" nucleus.
- Mollaret cells not pathognomonic.[6]
- Mixed population of inflammatory cells[4] (PMNs, monocytes, plasma cells, lymphocytes); usually lymphocyte predominant.[6]
Image:
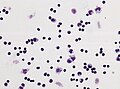
Meningeosis neoplastica
CNS lymphoma
Histology:[4]
- Too many cells - key feature.
- Not diagnostic... but should raise suspicion.
- Single cells (as typical of lymphoma/leukemia).
- Large lymphocytes - >2x RBC diameter.
- +/-Nuclear atypia.
- Radial segmentation - a completely cleaved nucleus/quasi-binucleation.
Notes:
- Massive karyorrhexis (nuclear fragmentation) is suggestive of lymphoma[4] - not common.
Meningeal carcinomatosis (Meningeosis carcinomatosa)
Histology:
- abnormal cell size / giant multinuclear cells.
- unusual nuclear/cytoplasm ratio.
- hyperchromatic nuclei.
- prominent nucleoli.
- atypical mitoses.
- cell clustering.
Notes:
- cell count can be normal.
- accompanied by granulocytes and monocytes.
Non-lymphoid, non-epithelial neoplasm
- Non-lymphoid, non-epithelial neoplasms are rarely found in the CSF.
- Ependymomas and medulloblastomas have a higher rate of dissemination than other primary brain tumors.
Meningeosis gliomatosa (Astrocytoma/Glioblastoma):
- May vaguely resemble a neuroendocrine tumour:
- Small cell clusters.
- Nuclear moulding.
- Cells somewhat larger than small cell carcinoma.
- Scant cytoplasm.
CNS fungal infections
- Cryptococcus is the most common.[8]
Cryptococcosis
Main article: Cryptococcosis
- AKA cryptococcus infection
General
- Usu. immunocompromised host.
Microscopic
Microscopic appearance:
- Yeast:[8]
- Round/ovoid 5-15 micrometres.
- Thick mucopolysacchardie capsule + refractile centre.
- "Target-like" shape/"bull's eye" appearance.
- "Tear drop-shapped" budding pattern (useful to differentiate from Blastomyces, Histoplasma).
Images:
- Cryptococcus in lung FNA - Field stain (WC).
- Crytococcosis - mucicarmine stain (WC).
- Crytococcosis - methenamine silver stain (WC).
See also
References
- ↑ Mody, Dina R. (2018). Diagnostic Cytopathology (1st ed.). Elsevier Canada. pp. II-3 2. ISBN 978-1931884556.
- ↑ Liggett, SB.; Berger, JR.; Hush, J. (Aug 1982). "Cerebrospinal fluid xanthochromia with rifampin.". Ann Neurol 12 (2): 228-9. doi:10.1002/ana.410120240. PMID 7125611.
- ↑ Bremer, HL. (May 1985). "Identification of xanthochromia.". JAMA 253 (17): 2496. PMID 3981778.
- ↑ 4.0 4.1 4.2 4.3 4.4 4.5 Lefkowitch, Jay H. (2006). Anatomic Pathology Board Review (1st ed.). Saunders. pp. 681 (Q25). ISBN 978-1416025887.
- ↑ MUN. 4 November 2010.
- ↑ 6.0 6.1 6.2 6.3 6.4 http://emedicine.medscape.com/article/1169489-overview
- ↑ http://www.mondofacto.com/facts/dictionary?monocytoid+cell
- ↑ 8.0 8.1 Lefkowitch, Jay H. (2006). Anatomic Pathology Board Review (1st ed.). Saunders. pp. 682. ISBN 978-1416025887.