Difference between revisions of "Gastroesophageal reflux disease"
Jump to navigation
Jump to search
m (touch) |
(→Gross) |
||
| (3 intermediate revisions by the same user not shown) | |||
| Line 53: | Line 53: | ||
Note: | Note: | ||
*Many be graded using ''Savary-Miller classification''. | *Many be graded using ''Savary-Miller classification'' or ''Los Angeles classification''.<ref name=pmid20659145>{{Cite journal | last1 = Genta | first1 = RM. | last2 = Spechler | first2 = SJ. | last3 = Kielhorn | first3 = AF. | title = The Los Angeles and Savary-Miller systems for grading esophagitis: utilization and correlation with histology. | journal = Dis Esophagus | volume = 24 | issue = 1 | pages = 10-7 | month = Jan | year = 2011 | doi = 10.1111/j.1442-2050.2010.01092.x | PMID = 20659145 }}</ref> | ||
Images: | Images: | ||
*[http://www.gastrohep.com/images/image.asp?id=171 Savary-Miller classification - endoscopic images (gastrohep.com)]. | *[http://www.gastrohep.com/images/image.asp?id=171 Savary-Miller classification - endoscopic images (gastrohep.com)]. | ||
===Los Angeles classification for GERD=== | |||
Features:<ref>URL: [http://www.sciencedirect.com/science/article/pii/S2212097113700463 http://www.sciencedirect.com/science/article/pii/S2212097113700463]. Accessed on: 14 April 2015</ref> | |||
{| class="wikitable sortable" | |||
! Classification | |||
! Description | |||
|- | |||
| A | |||
| mucosal break <=5 mm, not beyond the tops of two (adjacent) mucosal folds | |||
|- | |||
| B | |||
| mucosal break >5 mm, not beyond the tops of two (adjacent) mucosal folds | |||
|- | |||
| C | |||
| mucosa break beyond the tops of two mucosal folds but <75% of the esophageal circumference | |||
|- | |||
| D | |||
| mucosal break >=75% of the esophageal circumference | |||
|- | |||
|} | |||
Note: | |||
*Correlation with histology is poor; mucosal breaks are seen rarely.<ref name=pmid20659145>{{Cite journal | last1 = Genta | first1 = RM. | last2 = Spechler | first2 = SJ. | last3 = Kielhorn | first3 = AF. | title = The Los Angeles and Savary-Miller systems for grading esophagitis: utilization and correlation with histology. | journal = Dis Esophagus | volume = 24 | issue = 1 | pages = 10-7 | month = Jan | year = 2011 | doi = 10.1111/j.1442-2050.2010.01092.x | PMID = 20659145 }}</ref> | |||
==Microscopic== | ==Microscopic== | ||
| Line 89: | Line 111: | ||
www: | www: | ||
*[http://www.archivesofpathology.org/action/showFullPopup?id=i1543-2165-134-6-815-f03&doi=10.1043%2F1543-2165-134.6.815 EE versus GERD (archivesofpathology.org)].<ref name=pmid20524860>{{Cite journal | last1 = Genevay | first1 = M. | last2 = Rubbia-Brandt | first2 = L. | last3 = Rougemont | first3 = AL. | title = Do eosinophil numbers differentiate eosinophilic esophagitis from gastroesophageal reflux disease? | journal = Arch Pathol Lab Med | volume = 134 | issue = 6 | pages = 815-25 | month = Jun | year = 2010 | doi = 10.1043/1543-2165-134.6.815 | PMID = 20524860 }}</ref> | *[http://www.archivesofpathology.org/action/showFullPopup?id=i1543-2165-134-6-815-f03&doi=10.1043%2F1543-2165-134.6.815 EE versus GERD (archivesofpathology.org)].<ref name=pmid20524860>{{Cite journal | last1 = Genevay | first1 = M. | last2 = Rubbia-Brandt | first2 = L. | last3 = Rougemont | first3 = AL. | title = Do eosinophil numbers differentiate eosinophilic esophagitis from gastroesophageal reflux disease? | journal = Arch Pathol Lab Med | volume = 134 | issue = 6 | pages = 815-25 | month = Jun | year = 2010 | doi = 10.1043/1543-2165-134.6.815 | PMID = 20524860 }}</ref> | ||
==Stains== | |||
*[[Oil red O stain]] +ve in macrophages from [[bronchoalveolar lavage]] specimens.<ref name=pmid20466562>{{Cite journal | last1 = Hopkins | first1 = PM. | last2 = Kermeen | first2 = F. | last3 = Duhig | first3 = E. | last4 = Fletcher | first4 = L. | last5 = Gradwell | first5 = J. | last6 = Whitfield | first6 = L. | last7 = Godinez | first7 = C. | last8 = Musk | first8 = M. | last9 = Chambers | first9 = D. | title = Oil red O stain of alveolar macrophages is an effective screening test for gastroesophageal reflux disease in lung transplant recipients. | journal = J Heart Lung Transplant | volume = 29 | issue = 8 | pages = 859-64 | month = Aug | year = 2010 | doi = 10.1016/j.healun.2010.03.015 | PMID = 20466562 }}</ref> | |||
==Sign out== | ==Sign out== | ||
| Line 139: | Line 164: | ||
*[[Barrett's esophagus]]. | *[[Barrett's esophagus]]. | ||
*[[PPI effect]]. | *[[PPI effect]]. | ||
*[[Glycogenic acanthosis of the esophagus]]. | |||
==References== | ==References== | ||
Latest revision as of 19:27, 14 April 2016
| Gastroesophageal reflux disease | |
|---|---|
| Diagnosis in short | |
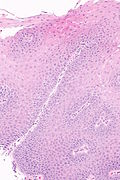
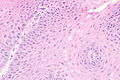
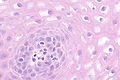
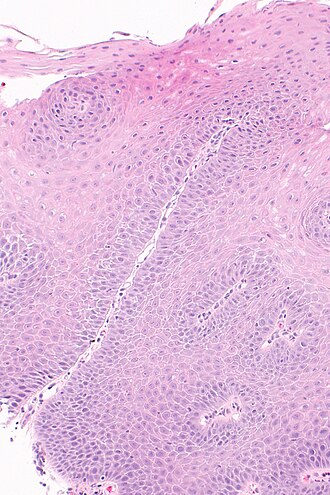 Micrograph showing histology compatible with gastroesophageal reflux disease. H&E stain. | |
|
| |
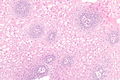
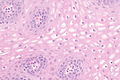
| LM | basal cell hyperplasia (> 3 cells thick or >15% of epithelial thickness), papillae elongated (papillae reach into the top 1/3 of the epithelial layer), inflammation, esp. eosinophils, lymphocytes with convoluted nuclei ("squiggle cells"), +/-intraepithelial edema, +/-apoptotic cells, +/-glycogenation |
| LM DDx | intestinal metaplasia (Barrett's esophagus), eosinophilic esophagitis, acute esophagitis |
| Site | esophagus |
|
| |
| Associated Dx | obesity, Barrett's esophagus |
| Prevalence | common |
| Endoscopy | erythema, erosions, +/-ulceration. |
| Prognosis | benign |
| Clin. DDx | eosinophilic esophagitis, acute esophagitis |
| Treatment | proton pump inhibitors |
Gastroesophageal reflux disease, abbreviated GERD, is a common pathology of the esophagus. It is occasionally abbreviated GORD (gastro-oesophageal reflux disease).
Reflux esophagitis redirects here. It technically isn't a synonym.[1][2]
General
Clinical:
- Usually chest pain
- +/-Abdominal pain.
- +/-Vomiting.
- +/-Blood loss.
Treatment:
- Treated with proton pump inhibitors (PPIs).
DDx (clinical):
Gross
- Erythema.
- Erosions.
- +/-Ulceration.
Note:
- Many be graded using Savary-Miller classification or Los Angeles classification.[3]
Images:
Los Angeles classification for GERD
Features:[4]
| Classification | Description |
|---|---|
| A | mucosal break <=5 mm, not beyond the tops of two (adjacent) mucosal folds |
| B | mucosal break >5 mm, not beyond the tops of two (adjacent) mucosal folds |
| C | mucosa break beyond the tops of two mucosal folds but <75% of the esophageal circumference |
| D | mucosal break >=75% of the esophageal circumference |
Note:
- Correlation with histology is poor; mucosal breaks are seen rarely.[3]
Microscopic
Features:
- Basal cell hyperplasia;[5] > 3 cells thick or >15% of epithelial thickness.
- Papillae elongated; papillae reach into the top 1/3 of the epithelial layer.[6]
- Inflammation, esp. eosinophils, lymphocytes with convoluted nuclei ("squiggle cells").
- +/-Intraepithelial edema.
- +/-Apoptotic cells.[7]
- +/-Glycogen - cytoplasm cleared (white).[8]
Notes:
- Intraepithelial cells with irregular nuclear contours, "squiggle cells" (T lymphocytes[9]), may mimic neutrophils.
- Changes may be focal.
- PPI effect may be seen in a concurrent gastric biopsy.
- Perinuclear clearing may be seen.[10]
DDx:
- Eosinophilic esophagitis - characterized by similar histomorphologic features. The key difference is: more eosinophils.
- Barrett's esophagus - intestinal metaplasia may be minimal.
Images
www:
Stains
- Oil red O stain +ve in macrophages from bronchoalveolar lavage specimens.[12]
Sign out
Poorly oriented
ESOPHAGUS, BIOPSY: - SQUAMOUS MUCOSA WITH BASAL CELL HYPERPLASIA, INTRAEPITHELIAL EDEMA AND RARE INTRAEPITHELIAL EOSINOPHILS -- COMPATIBLE WITH GASTROESOPHAGEAL REFLUX.
Columnar epithelium present
ESOPHAGUS, BIOPSY: - SQUAMOUS MUCOSA WITH BASAL CELL HYPERPLASIA, INTRAEPITHELIAL EDEMA AND RARE INTRAEPITHELIAL EOSINOPHILS -- COMPATIBLE WITH GASTROESOPHAGEAL REFLUX. - COLUMNAR EPITHELIUM WITH MODERATE CHRONIC INACTIVE INFLAMMATION. - NEGATIVE FOR INTESTINAL METAPLASIA. - NEGATIVE FOR DYSPLASIA AND NEGATIVE FOR MALIGNANCY.
Ulceration present
ESOPHAGUS, DISTAL, BIOPSY: - SQUAMOUS MUCOSA WITH BASAL CELL HYPERPLASIA, INTRAEPITHELIAL EDEMA, RARE INTRAEPITHELIAL EOSINOPHILS AND EVIDENCE OF ULCERATION -- COMPATIBLE WITH GASTROESOPHAGEAL REFLUX. - COLUMNAR EPITHELIUM WITH MODERATE CHRONIC INACTIVE INFLAMMATION. - NEGATIVE FOR INTESTINAL METAPLASIA. - NEGATIVE FOR DYSPLASIA AND NEGATIVE FOR MALIGNANCY. COMMENT: PAS-D staining is negative for microorganisms.
BE and GERD present
ESOPHAGUS (DISTAL), BIOPSY: - COLUMNAR EPITHELIUM WITH INTESTINAL METAPLASIA AND MODERATE CHRONIC INFLAMMATION, SEE COMMENT. - SQUAMOUS MUCOSA WITH BASAL CELL HYPERPLASIA, INTRAEPITHELIAL EDEMA AND RARE INTRAEPITHELIAL EOSINOPHILS -- COMPATIBLE WITH GASTROESOPHAGEAL REFLUX. - NEGATIVE FOR DYSPLASIA AND NEGATIVE FOR MALIGNANCY. COMMENT: The findings are consistent with Barrett's esophagus in the appropriate endoscopic setting.
See also
References
- ↑ Orbelo, DM.; Enders, FT.; Romero, Y.; Francis, DL.; Achem, SR.; Dabade, TS.; Crowell, MD.; Geno, DM. et al. (Jan 2014). "Once-Daily Omeprazole/Sodium Bicarbonate Heals Severe Refractory Reflux Esophagitis with Morning or Nighttime Dosing.". Dig Dis Sci. doi:10.1007/s10620-013-3017-y. PMID 24448652.
- ↑ Karbasi, A.; Ardestani, ME.; Ghanei, M.; Harandi, AA. (Jun 2013). "The association between reflux esophagitis and airway hyper-reactivity in patients with gastro-esophageal reflux.". J Res Med Sci 18 (6): 473-6. PMID 24250694.
- ↑ 3.0 3.1 Genta, RM.; Spechler, SJ.; Kielhorn, AF. (Jan 2011). "The Los Angeles and Savary-Miller systems for grading esophagitis: utilization and correlation with histology.". Dis Esophagus 24 (1): 10-7. doi:10.1111/j.1442-2050.2010.01092.x. PMID 20659145.
- ↑ URL: http://www.sciencedirect.com/science/article/pii/S2212097113700463. Accessed on: 14 April 2015
- ↑ Steiner, SJ.; Kernek, KM.; Fitzgerald, JF. (May 2006). "Severity of basal cell hyperplasia differs in reflux versus eosinophilic esophagitis.". J Pediatr Gastroenterol Nutr 42 (5): 506-9. doi:10.1097/01.mpg.0000221906.06899.1b. PMID 16707971.
- ↑ Cotran, Ramzi S.; Kumar, Vinay; Fausto, Nelson; Nelso Fausto; Robbins, Stanley L.; Abbas, Abul K. (2005). Robbins and Cotran pathologic basis of disease (7th ed.). St. Louis, Mo: Elsevier Saunders. pp. 804. ISBN 0-7216-0187-1.
- ↑ Wetscher GJ, Schwelberger H, Unger A, et al. (December 1998). "Reflux-induced apoptosis of the esophageal mucosa is inhibited in Barrett's epithelium". Am. J. Surg. 176 (6): 569–73. PMID 9926792.
- ↑ Vadva MD, Triadafilopoulos G (July 1993). "Glycogenic acanthosis of the esophagus and gastroesophageal reflux". J. Clin. Gastroenterol. 17 (1): 79–83. PMID 8409304.
- ↑ Cucchiara, S.; D'Armiento, F.; Alfieri, E.; Insabato, L.; Minella, R.; De Magistris, TM.; Scoppa, A. (Nov 1995). "Intraepithelial cells with irregular nuclear contours as a marker of esophagitis in children with gastroesophageal reflux disease.". Dig Dis Sci 40 (11): 2305-11. PMID 7587806.
- ↑ URL: http://155.37.5.42/eAtlas/GI/1262.htm. Accessed on: 31 January 2014.
- ↑ Genevay, M.; Rubbia-Brandt, L.; Rougemont, AL. (Jun 2010). "Do eosinophil numbers differentiate eosinophilic esophagitis from gastroesophageal reflux disease?". Arch Pathol Lab Med 134 (6): 815-25. doi:10.1043/1543-2165-134.6.815. PMID 20524860.
- ↑ Hopkins, PM.; Kermeen, F.; Duhig, E.; Fletcher, L.; Gradwell, J.; Whitfield, L.; Godinez, C.; Musk, M. et al. (Aug 2010). "Oil red O stain of alveolar macrophages is an effective screening test for gastroesophageal reflux disease in lung transplant recipients.". J Heart Lung Transplant 29 (8): 859-64. doi:10.1016/j.healun.2010.03.015. PMID 20466562.