Difference between revisions of "Primary biliary cholangitis"
m (touch) |
m |
||
| (10 intermediate revisions by 2 users not shown) | |||
| Line 1: | Line 1: | ||
{{ Infobox diagnosis | {{ Infobox diagnosis | ||
| Name = {{PAGENAME}} | | Name = {{PAGENAME}} | ||
| Image = | | Image = Primary_biliary_cirrhosis_intermed_mag.jpg | ||
| Width = | | Width = | ||
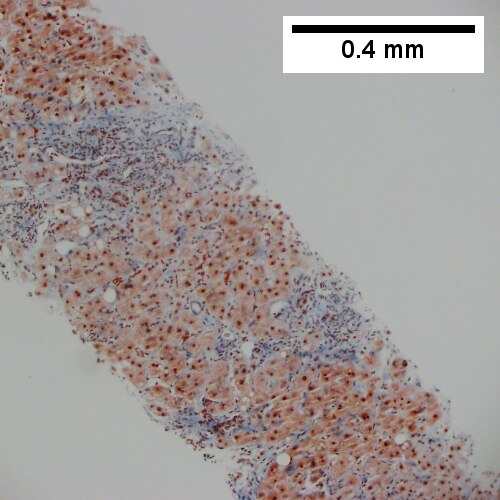
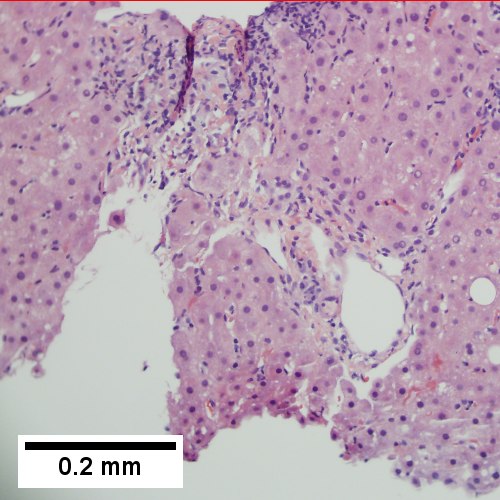
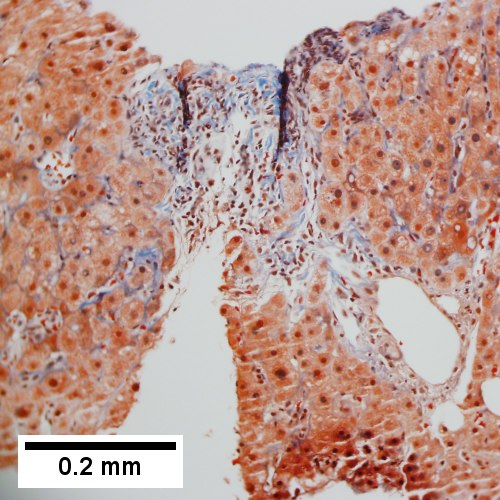
| Caption = Primary biliary | | Caption = Primary biliary cholangitis. [[H&E stain]]. | ||
| Synonyms = primary biliary cirrhosis (obsolete term) | |||
| Micro = "florid duct lesion": intraepithelial lymphocytes - in bile duct, bile duct epithelial cells with eosinophilic cytoplasm; plasma cells; +/-[[granulomas]] (close to bile duct); +/-"garland" cirrhosis -- has irregular border | | Micro = "florid duct lesion": intraepithelial lymphocytes - in bile duct, bile duct epithelial cells with eosinophilic cytoplasm; plasma cells; +/-[[granulomas]] (close to bile duct); +/-"garland" cirrhosis -- has irregular border | ||
| Subtypes = | | Subtypes = | ||
| Line 28: | Line 29: | ||
| ClinDDx = | | ClinDDx = | ||
}} | }} | ||
'''Primary biliary | '''Primary biliary cholangitis''', abbreviated '''PBC''', is a rare [[medical liver disease]]. | ||
It was previously known as ''primary ciliary cirrhosis''.<ref name=pmid26416194>{{cite journal |authors=Beuers U, Gershwin ME, Gish RG, Invernizzi P, Jones DE, Lindor K, Ma X, Mackay IR, Parés A, Tanaka A, Vierling JM, Poupon R |title=Changing Nomenclature for PBC: From 'Cirrhosis' to 'Cholangitis' |journal=Am J Gastroenterol |volume=110 |issue=11 |pages=1536–8 |date=November 2015 |pmid=26416194 |pmc=4679751 |doi=10.1038/ajg.2015.312 |url=}}</ref> | |||
==General== | ==General== | ||
| Line 81: | Line 84: | ||
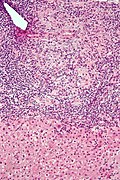
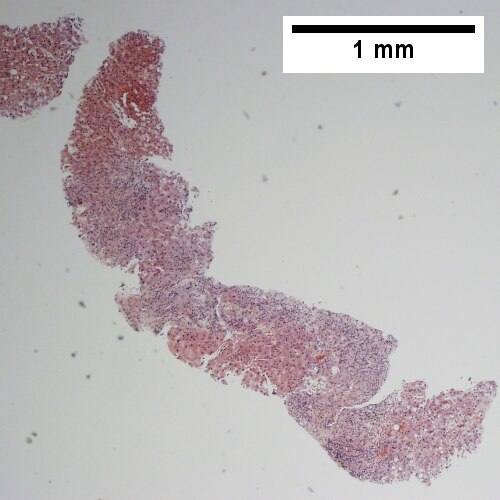
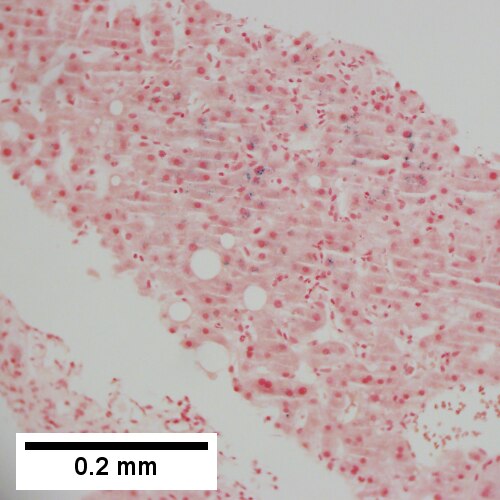
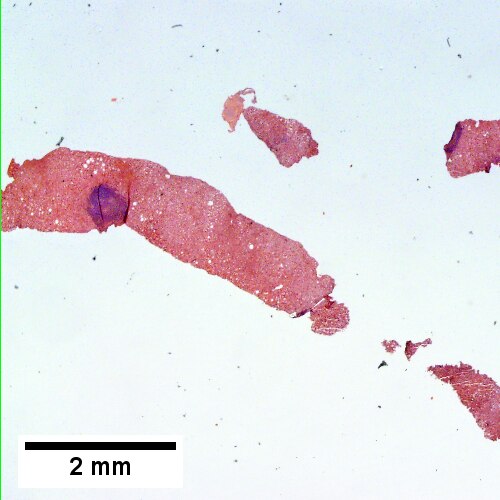
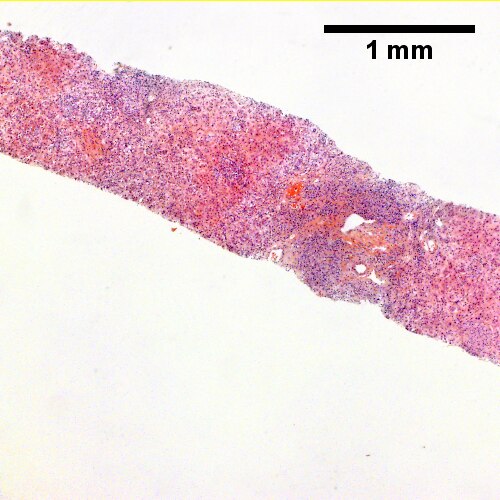
Image:Primary_biliary_cirrhosis_low_mag.jpg | PBC - low mag. (WC) | Image:Primary_biliary_cirrhosis_low_mag.jpg | PBC - low mag. (WC) | ||
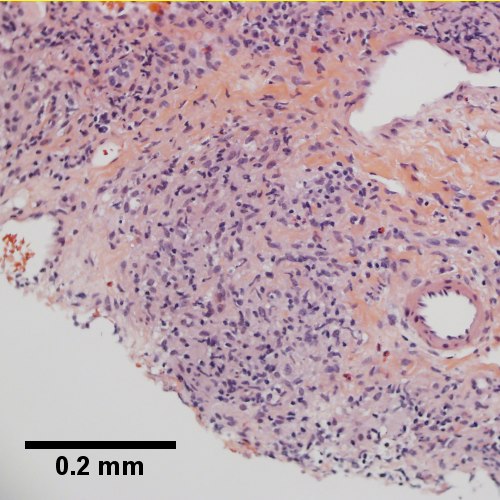
Image:Primary_biliary_cirrhosis_intermed_mag.jpg | PBC - intermed. mag. (WC) | Image:Primary_biliary_cirrhosis_intermed_mag.jpg | PBC - intermed. mag. (WC) | ||
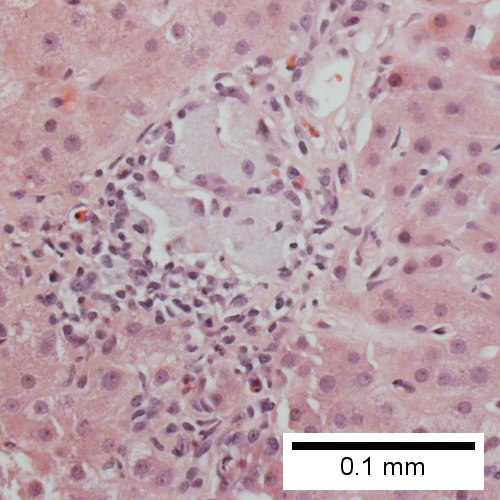
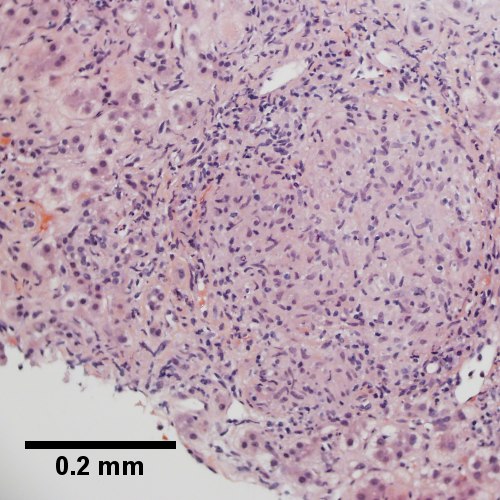
Image:Primary_biliary_cirrhosis_intermed_mag_2.jpg | PBC - intermed. mag. (WC) | |||
</gallery> | </gallery> | ||
www: | www: | ||
*[http://www.gidesigns.net/images/MC-copper-flower-garland-L.jpg Garland - wreath of flowers (gidesigns.net)]. | *[http://www.gidesigns.net/images/MC-copper-flower-garland-L.jpg Garland - wreath of flowers (gidesigns.net)]. | ||
{| | |||
[[File:1 PBC 4 680x512px.tif|Inflamed triads [arrows] amid undisturbed hepatocytes (Row 1 Left 40X).]] | |||
[[File:2 PBC 4 680x512px.tif|Granuloma in portal triad (Row 1 Right 400X).]] | |||
<br> | |||
[[File:3 PBC 4 680x512px.tif|Florid duct lesion (Row 2 Left 400X).]] | |||
[[File:4 PBC 4 680x512px.tif|Triad missing interlobular bile duct (Row 2 Right 400X).]] | |||
|} | |||
Primary biliary cirrhosis. Inflamed triads [arrows] amid undisturbed hepatocytes (Row 1 Left 40X). Granuloma in portal triad (Row 1 Right 400X). Florid duct lesion (Row 2 Left 400X). Triad missing interlobular bile duct (Row 2 Right 400X). | |||
{| | |||
[[File:1 PBC 3 680x512px.tif| Ill defined triads, inflamed lobule (40X).]] | |||
[[File:2 PBC 3 680x512px.tif| Triad without a bile duct. Macrophages & occasional lymphocytes without epithelioid cells needed for granuloma and space where bile duct likely once was [cyan arrowhead] (400X).]] | |||
<br> | |||
[[File:3 PBC 3 680x512px.tif| PAS without diastase shows triad lacking bile duct and piecemeal necrosis (200X).]] | |||
[[File:4 PBC 3 680x512px.tif| PAS with diastase shows bile duct/proliferating bile ductules with epithelial injury and hepatocytes with ballooning degeneration (400X).]] | |||
<br> | |||
[[File:5 PBC 3 680x512px.tif| Trichrome shows space of Disse collagenization and periportal fibrosis without definite bridging (100X)..]] | |||
[[File:6 PBC 3 680x512px.tif| Iron stain shows isolated focus of hepatocytes with cytoplasmic blue granules (200X)]] | |||
|} | |||
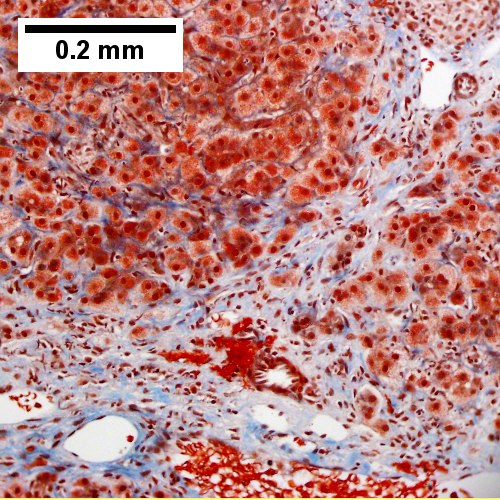
Primary biliary cirrhosis. AMA positive. Viral serology/ANA negative. No definite granulomas. Ill defined triads, inflamed lobule (Row 1 Left 40X). Triad without a bile duct. Macrophages & occasional lymphocytes without epithelioid cells needed for granuloma and space where bile duct likely once was [cyan arrowhead] (Row 1 Right 400X). PAS without diastase shows triad lacking bile duct and piecemeal necrosis (Row 2 Left 200X). PAS with diastase shows bile duct/proliferating bile ductules with epithelial injury and hepatocytes with ballooning degeneration (Row 2 Right 400X). Trichrome shows space of Disse collagenization and periportal fibrosis without definite bridging (Row 3 Left 100X). Iron stain shows isolated focus of hepatocytes with cytoplasmic blue granules (Row 3 Right 200X). | |||
{| | |||
[[File:1 PBC 2 680x512px.tif|Two inflamed triads accompany acini with mild steatosis (20X).]] | |||
[[File:2 PBC 2 680x512px.tif|A triad bears a poorly formed granuloma [yellow arrowhead]. A bile duct is also seen [red arrowhead] (200X).]] | |||
<br> | |||
[[File:3 PBC 2 680x512px.tif|A triad lacks a bile duct (200X).]] | |||
[[File:4 PBC 2 680x512px.tif|Trichrome of the same triad shows portal fibrosis (200X).]] | |||
|} | |||
Primary biliary cirrhosis. Two inflamed triads accompany acini with mild steatosis (Row 1 Left 20X). A triad bears a poorly formed granuloma [yellow arrowhead]. A bile duct is also seen [red arrowhead] (Row 1 Right 200X). A triad lacks a bile duct (Row 2 Left 200X). Trichrome of the same triad shows portal fibrosis (Row 2 Right 200X). | |||
{| | |||
[[File:1 PBC - 1 - 40X 680x512px.tif|Acini & lobules distorted by inflammation]] | |||
[[File:2 PBC - 1 - 200X 680x512px.tif|Loose granuloma in triad without duct]] | |||
<br> | |||
[[File:3 PBC - 1 - 200X 680x512px.tif|Well-formed granuloma]] | |||
[[File:4 PBC - 1 -200X 680x512px.tif|Piecemeal necrosis, PAS without diastase]] | |||
<br> | |||
[[File:5 PBC - 1 -400X 680x512px.tif|Damaged bile duct, PAS with diastase]] | |||
[[File:6 PBC - 1 -200X 680x512px.tif|Bridging fibrosis, trichrome]] | |||
|} | |||
Primary biliary cirrhosis with bridging fibrosis. Acini & lobules distorted by inflammation (Row 1 Left 40X) Loose granuloma in triad without duct (Row 1 Right 200X) Well-formed granuloma (Row 2 Left 200X) Piecemeal necrosis, PAS without diastase (Row 2 Right 200X) Damaged bile duct, PAS with diastase (Row 3 Left 400X) Bridging fibrosis, trichrome (Row 3 Right,200X) | |||
{| | |||
[[File:1 PBC 5 680x512px.tif|Stage 4 PBC.]] | |||
[[File:2 PBC 5 680x512px.tif| Stage 4 PBC.]] | |||
<br> | |||
[[File:3 PBC 5 680x512px.tif| Stage 4 PBC.]] | |||
[[File:4 PBC 5 680x512px.tif| Stage 4 PBC.]] | |||
<br> | |||
[[File:5 PBC 5 680x512px.tif| Stage 4 PBC.]] | |||
[[File:6 PBC 5 680x512px.tif| Stage 4 PBC.]] | |||
|} | |||
Primary biliary cirrhosis with Metavir stage 4 fibrosis (extensive fibrosis/cirrhosis). The patient was AMA positive and ANA negative. A. Inflamed tracts and bridges are intensely inflamed, with odd appearing edges of hepatocytes (arrows), suggestive of a jig saw pattern [40x]. B. Trichrome shows thin fibrous bands bounding regenerative isles (arrows) [Trichrome, 100X]. C. Reticulin shows two cell thick cords and cords lacking orientation, documenting regeneration; black lines about single cells document piecemeal necrosis [100X]. D. Lymphocytes, plasma cells, and macrophages, show piecemeal necrosis, surrounding hepatocytes (cyan arrows), as well as spreading into the lobule (green arrows), with aggregates reflecting spotty necrosis (black arrow). [400X]. E. PAS with diastase highlights a proliferated bile ductule (arrows) with epithelial damage [400X]. F. PAS with diastase shows an arteriole (green arrow) at great distance from an isolated bile ductule at the periphery of the triad (cyan arrow), consistent with loss of bile duct; neutrophils (black arrows) do not prove ascending cholangitis [400X]. | |||
===Staging PBC=== | ===Staging PBC=== | ||
Latest revision as of 22:29, 9 October 2021
| Primary biliary cholangitis | |
|---|---|
| Diagnosis in short | |
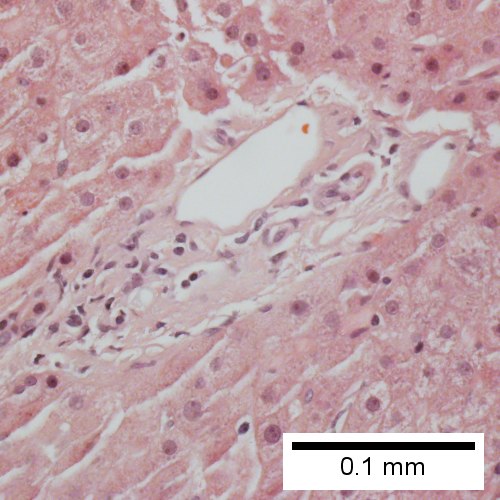
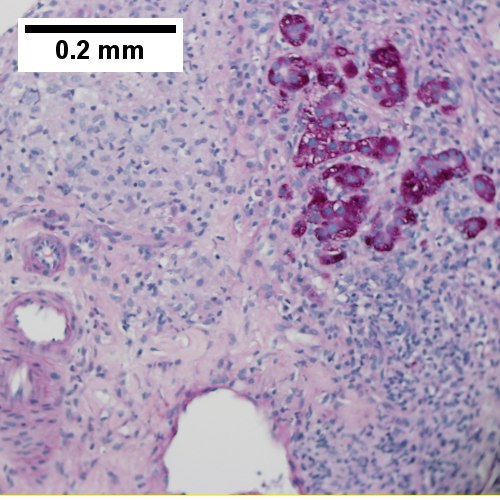
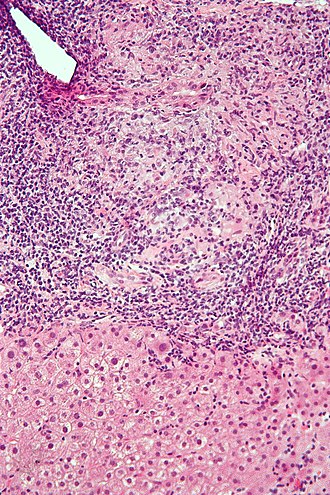 Primary biliary cholangitis. H&E stain. | |
|
| |
| Synonyms | primary biliary cirrhosis (obsolete term) |
|
| |
| LM | "florid duct lesion": intraepithelial lymphocytes - in bile duct, bile duct epithelial cells with eosinophilic cytoplasm; plasma cells; +/-granulomas (close to bile duct); +/-"garland" cirrhosis -- has irregular border |
| LM DDx | sarcoidosis, primary sclerosing cholangitis, viral hepatitis, autoimmune hepatitis, drug-induced liver disease, Hodgkin's lymphoma |
| Site | liver - see medical liver diseases |
|
| |
| Associated Dx | other autoimmune conditions, e.g. celiac disease, Sjögren syndrome |
| Clinical history | woman, middle age |
| Symptoms | pruritis |
| Blood work | AMA +ve |
Primary biliary cholangitis, abbreviated PBC, is a rare medical liver disease.
It was previously known as primary ciliary cirrhosis.[1]
General
Epidemiology:
- Female>male (~9:1).[2]
- Usually middle age.
- Associated with other autoimmune conditions (Sjögren syndrome, progressive systemic sclerosis, celiac disease).
Etiology:
- Autoimmune.
Serology:
- AMA +ve.[3]
Classic presentation:
- Pruritis.
Pathophysiology:
- Septal bile duct attacked.
Treatment:
- Ursodeoxycholic acid.
- May be indication for transplant.
Microscopic
Features:
- "Florid duct lesion":[4]
- Intraepithelial lymphocytes - in bile duct - key feature.
- Bile duct epithelial cells with eosinophilic cytoplasm.[5]
- Plasma cells.
- Granulomas - close to bile duct.
- Seen in classic presentation -- often not present or poorly formed.
- Focal damage (may be missed on biopsy -- due to sampling).
- "Garland" cirrhosis -- has irregular border (unlike in EtOH).
- Garland originally "wreath of flowers" (in French).[6]
Notes:
- PAS stain useful for examining basement membrane... which is lost in PBC.
- Lobular inflammation should be minimal.
- May cause cholestatic picture.[7]
DDx:[8]
- Sarcoidosis (if granulomas present).
- Primary sclerosing cholangitis.
- Viral hepatitis.
- Autoimmune hepatitis.
- Drug-induced liver disease.
- Hodgkin's lymphoma.[9]
Images
www:
![Inflamed triads [arrows] amid undisturbed hepatocytes (Row 1 Left 40X).](/w/images/thumb/9/95/1_PBC_4_680x512px.tif/lossy-page1-500px-1_PBC_4_680x512px.tif.jpg)
Primary biliary cirrhosis. Inflamed triads [arrows] amid undisturbed hepatocytes (Row 1 Left 40X). Granuloma in portal triad (Row 1 Right 400X). Florid duct lesion (Row 2 Left 400X). Triad missing interlobular bile duct (Row 2 Right 400X).
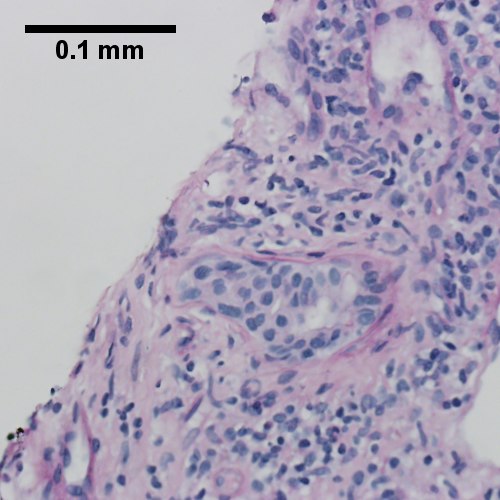
![Triad without a bile duct. Macrophages & occasional lymphocytes without epithelioid cells needed for granuloma and space where bile duct likely once was [cyan arrowhead] (400X).](/w/images/thumb/1/17/2_PBC_3_680x512px.tif/lossy-page1-500px-2_PBC_3_680x512px.tif.jpg)
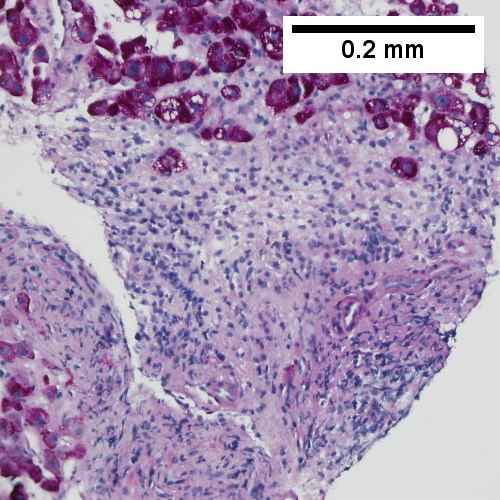
Primary biliary cirrhosis. AMA positive. Viral serology/ANA negative. No definite granulomas. Ill defined triads, inflamed lobule (Row 1 Left 40X). Triad without a bile duct. Macrophages & occasional lymphocytes without epithelioid cells needed for granuloma and space where bile duct likely once was [cyan arrowhead] (Row 1 Right 400X). PAS without diastase shows triad lacking bile duct and piecemeal necrosis (Row 2 Left 200X). PAS with diastase shows bile duct/proliferating bile ductules with epithelial injury and hepatocytes with ballooning degeneration (Row 2 Right 400X). Trichrome shows space of Disse collagenization and periportal fibrosis without definite bridging (Row 3 Left 100X). Iron stain shows isolated focus of hepatocytes with cytoplasmic blue granules (Row 3 Right 200X).
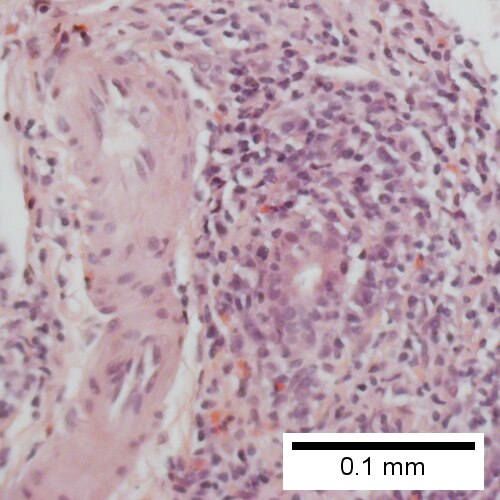
![A triad bears a poorly formed granuloma [yellow arrowhead]. A bile duct is also seen [red arrowhead] (200X).](/w/images/thumb/6/65/2_PBC_2_680x512px.tif/lossy-page1-500px-2_PBC_2_680x512px.tif.jpg)
Primary biliary cirrhosis. Two inflamed triads accompany acini with mild steatosis (Row 1 Left 20X). A triad bears a poorly formed granuloma [yellow arrowhead]. A bile duct is also seen [red arrowhead] (Row 1 Right 200X). A triad lacks a bile duct (Row 2 Left 200X). Trichrome of the same triad shows portal fibrosis (Row 2 Right 200X).
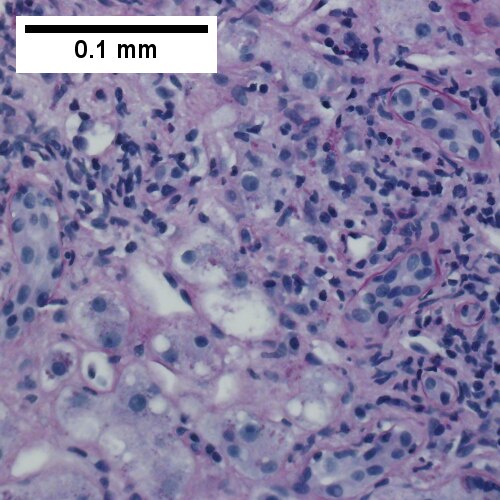
Primary biliary cirrhosis with bridging fibrosis. Acini & lobules distorted by inflammation (Row 1 Left 40X) Loose granuloma in triad without duct (Row 1 Right 200X) Well-formed granuloma (Row 2 Left 200X) Piecemeal necrosis, PAS without diastase (Row 2 Right 200X) Damaged bile duct, PAS with diastase (Row 3 Left 400X) Bridging fibrosis, trichrome (Row 3 Right,200X)

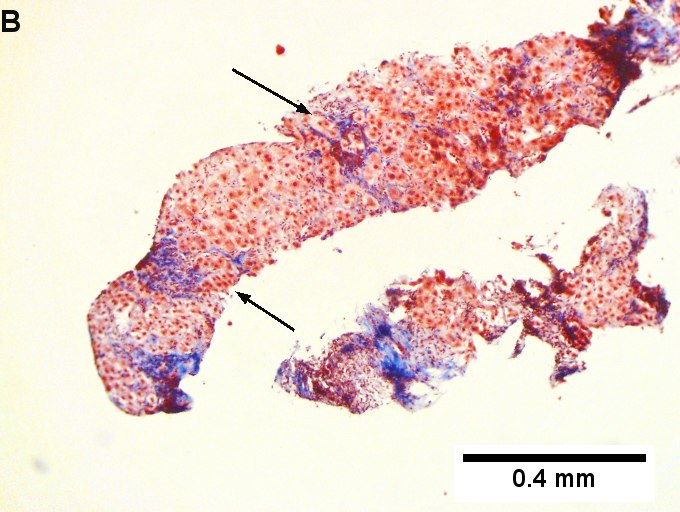
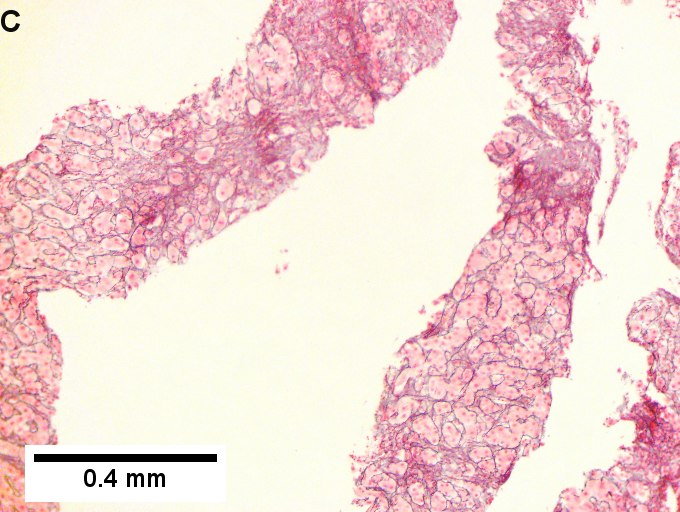
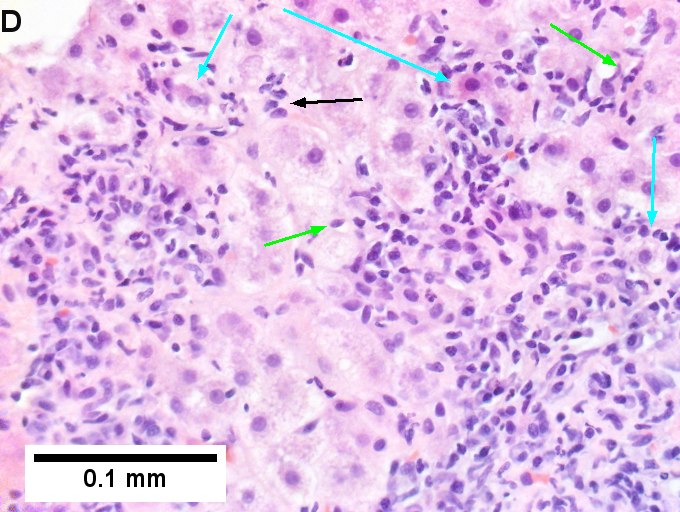
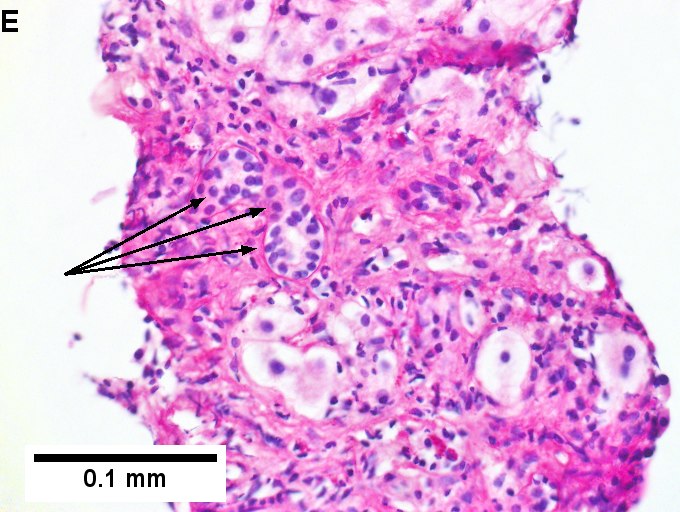
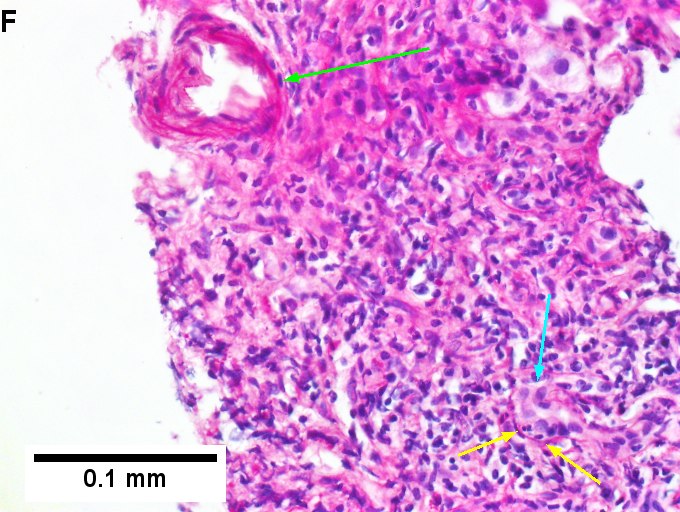
Primary biliary cirrhosis with Metavir stage 4 fibrosis (extensive fibrosis/cirrhosis). The patient was AMA positive and ANA negative. A. Inflamed tracts and bridges are intensely inflamed, with odd appearing edges of hepatocytes (arrows), suggestive of a jig saw pattern [40x]. B. Trichrome shows thin fibrous bands bounding regenerative isles (arrows) [Trichrome, 100X]. C. Reticulin shows two cell thick cords and cords lacking orientation, documenting regeneration; black lines about single cells document piecemeal necrosis [100X]. D. Lymphocytes, plasma cells, and macrophages, show piecemeal necrosis, surrounding hepatocytes (cyan arrows), as well as spreading into the lobule (green arrows), with aggregates reflecting spotty necrosis (black arrow). [400X]. E. PAS with diastase highlights a proliferated bile ductule (arrows) with epithelial damage [400X]. F. PAS with diastase shows an arteriole (green arrow) at great distance from an isolated bile ductule at the periphery of the triad (cyan arrow), consistent with loss of bile duct; neutrophils (black arrows) do not prove ascending cholangitis [400X].
Staging PBC
PBC is staged according to Ludwig:[10]
- Stage 1: Portal - inflammation or bile duct abnormalities.
- Stage 2: Periportal - periportal fibrosis (enlargement of portal tracts) +/- inflammation.
- Stage 3: Septal - septal fibrosis +/-inflammation in septa.
- Stage 4: Cirrhosis - nodules of hepatocytes +/- inflammation.
Notes:
- There can be significant variation in staging on biopsy - due to variability of fibrosis in a PBC liver.[11]
- "Worst area" in biopsy specimen is used to determine stage.
See also
References
- ↑ Beuers U, Gershwin ME, Gish RG, Invernizzi P, Jones DE, Lindor K, Ma X, Mackay IR, Parés A, Tanaka A, Vierling JM, Poupon R (November 2015). "Changing Nomenclature for PBC: From 'Cirrhosis' to 'Cholangitis'". Am J Gastroenterol 110 (11): 1536–8. doi:10.1038/ajg.2015.312. PMC 4679751. PMID 26416194. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4679751/.
- ↑ Tadrous, Paul.J. Diagnostic Criteria Handbook in Histopathology: A Surgical Pathology Vade Mecum (1st ed.). Wiley. pp. 162. ISBN 978-0470519035.
- ↑ Nguyen, DL.; Juran, BD.; Lazaridis, KN. (Oct 2010). "Primary biliary cirrhosis.". Best Pract Res Clin Gastroenterol 24 (5): 647-54. doi:10.1016/j.bpg.2010.07.006. PMID 20955967.
- ↑ Nakanuma, Y.; Harada, K. (Sep 1993). "Florid duct lesion in primary biliary cirrhosis shows highly proliferative activities.". J Hepatol 19 (2): 216-21. PMID 7905494.
- ↑ OA. 11 September 2009.
- ↑ http://dictionary.reference.com/browse/garland
- ↑ Grimm, D.; Thimme, R. (Apr 2011). "[Cholestatic liver diseases].". Ther Umsch 68 (4): 195-9. doi:10.1024/0040-5930/a000150. PMID 21452140.
- ↑ Tadrous, Paul.J. Diagnostic Criteria Handbook in Histopathology: A Surgical Pathology Vade Mecum (1st ed.). Wiley. pp. 163. ISBN 978-0470519035.
- ↑ Vanishing bile duct syndrome and Hodgkin disease: a case series and review of the literature. Pass AK, McLin VA, Rushton JR, Kearney DL, Hastings CA, Margolin JF. J Pediatr Hematol Oncol. 2008 Dec;30(12):976-80. PMID 19131796.
- ↑ PBC. eMedicine.com. URL: http://emedicine.medscape.com/article/171117-diagnosis. Accessed on: 22 September 2009.
- ↑ J Clin Pathol. 1996 July; 49(7): 556-559. Available at: http://www.pubmedcentral.nih.gov/articlerender.fcgi?artid=500569. Accessed on: September 22, 2009.