Difference between revisions of "Endometrium"
| (15 intermediate revisions by the same user not shown) | |||
| Line 13: | Line 13: | ||
===Endometrial thickness on ultrasound=== | ===Endometrial thickness on ultrasound=== | ||
*A thin endometrium on ultrasound has a very low risk of malignancy.<ref | *A thin endometrium on ultrasound has a very low risk of malignancy.<ref name=pmid15283934>{{Cite journal | last1 = Gambacciani | first1 = M. | last2 = Monteleone | first2 = P. | last3 = Ciaponi | first3 = M. | last4 = Sacco | first4 = A. | last5 = Genazzani | first5 = AR. | title = Clinical usefulness of endometrial screening by ultrasound in asymptomatic postmenopausal women. | journal = Maturitas | volume = 48 | issue = 4 | pages = 421-4 | month = Aug | year = 2004 | doi = 10.1016/j.maturitas.2003.10.006 | PMID = 15283934 }}</ref> | ||
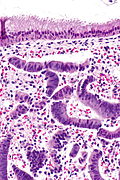
=Normal microscopic findings= | =Normal microscopic findings= | ||
| Line 42: | Line 42: | ||
*Focal [[complex endometrial hyperplasia]]. | *Focal [[complex endometrial hyperplasia]]. | ||
Image | ===Image=== | ||
*[http://www.ncbi.nlm.nih.gov/pmc/articles/PMC1860448/figure/fig4/ Gland compression (bmjjournals.com)].<ref name=pmid16873562/> | *[http://www.ncbi.nlm.nih.gov/pmc/articles/PMC1860448/figure/fig4/ Gland compression (bmjjournals.com)].<ref name=pmid16873562/> | ||
===Micro=== | ===Micro=== | ||
An increased gland density is seen focally, at the edge of one tissue fragment, in association with tearing of the stroma (compression artifact). | An increased gland density is seen focally, at the edge of one tissue fragment, in association with tearing of the stroma (compression artifact). | ||
===See also=== | |||
*[[Endometrial gland coiling]]. | |||
==Endocervical epithelium versus endometrial epithelium== | ==Endocervical epithelium versus endometrial epithelium== | ||
| Line 61: | Line 64: | ||
| hyperchromatic | | hyperchromatic | ||
|- | |- | ||
| | | [[Nucleus-to-cytoplasm ratio]] | ||
| moderate to high (1:2) | | moderate to high (1:2) | ||
| low (often 1:3) | | low (often 1:3) | ||
| Line 249: | Line 252: | ||
COMMENT: | COMMENT: | ||
Re-biopsy is advised. | Re-biopsy is advised. | ||
</pre> | |||
<pre> | |||
ENDOMETRIUM, BIOPSY: | |||
- BENIGN STRIPPED ENDOCERVICAL EPITHELIUM AND BENIGN INFLAMED ENDOCERVICAL MUCOSA. | |||
- NO DEFINITE ENDOMETRIUM WITH STROMA, INADEQUATE SPECIMEN. | |||
</pre> | </pre> | ||
| Line 348: | Line 357: | ||
| normal postmenopausal finding | | normal postmenopausal finding | ||
| [[Image:Nonproliferative endometrial epithelium - alt -- high mag.jpg|thumb|150px|center|Inactive endometrium. (WC)]] | | [[Image:Nonproliferative endometrial epithelium - alt -- high mag.jpg|thumb|150px|center|Inactive endometrium. (WC)]] | ||
|- | |||
| [[Disordered proliferative endometrium]] | |||
| proliferative focally dilated & irregular glands (usu. with tubal metaplasia) | |||
| no nuclear atypia, +/-evidence of shedding (stromal condensation) | |||
| [[simple endometrial hyperplasia]], [[proliferative phase endometrium]] | |||
| can be thought of a [[waffle diagnosis]] | |||
| [[Image:Disordered proliferative endometrium -- low mag.jpg|thumb|150px|center|Disordered proliferative endometrium. (WC)]] | |||
|- <!-- | |- <!-- | ||
| Diagnosis | | Diagnosis | ||
| Line 378: | Line 394: | ||
DDx: | DDx: | ||
*[[Small cell carcinoma]]. | *[[Small cell carcinoma]] - proliferative activity in the moulded (stromal condensation-like) cells. | ||
*[[Anovulatory endometrium]] - less neutrophils. | *[[Anovulatory endometrium]] - less neutrophils. | ||
| Line 390: | Line 406: | ||
===Sign out=== | ===Sign out=== | ||
<pre> | |||
Endometrium, Biopsy: | |||
- Consistent with menstrual endometrium. | |||
-- Weakly proliferative endometrial glands with apoptosis, fragmented. | |||
-- Abundant balls of condensed non-proliferative endometrial stroma and blood. | |||
</pre> | |||
====Block letters==== | |||
<pre> | <pre> | ||
ENDOMETRIUM, BIOPSY: | ENDOMETRIUM, BIOPSY: | ||
| Line 475: | Line 499: | ||
The presence of adipose tissue raises the possibility of perforation. | The presence of adipose tissue raises the possibility of perforation. | ||
The findings were briefly discussed with Dr. Brown on | The findings were briefly discussed with Dr. Brown on November 6, 2009. | ||
</pre> | </pre> | ||
| Line 489: | Line 513: | ||
==Anovulatory endometrium== | ==Anovulatory endometrium== | ||
{{Main|Anovulatory endometrium}} | |||
==Disordered proliferative endometrium== | ==Disordered proliferative endometrium== | ||
| Line 552: | Line 519: | ||
*[[AKA]] ''endometrium with disordered proliferative phase''. | *[[AKA]] ''endometrium with disordered proliferative phase''. | ||
*[[AKA]] ''disordered proliferative phase''. | *[[AKA]] ''disordered proliferative phase''. | ||
{{Main|Disordered proliferative endometrium}} | |||
==Endometrium with changes due to exogenous hormones== | ==Endometrium with changes due to exogenous hormones== | ||
| Line 650: | Line 534: | ||
==Endometrium with squamous morules== | ==Endometrium with squamous morules== | ||
{{Main|Endometrium with squamous morules}} | {{Main|Endometrium with squamous morules}} | ||
==Endometrium with psammoma bodies== | |||
{{Main|Endometrium with psammoma bodies}} | |||
==Endometrial hyperplasia== | ==Endometrial hyperplasia== | ||
| Line 668: | Line 555: | ||
*[[Uterine tumours]]. | *[[Uterine tumours]]. | ||
*[[Gynecologic pathology]]. | *[[Gynecologic pathology]]. | ||
*[[Psammoma bodies]]. | |||
=References= | =References= | ||
Latest revision as of 14:37, 2 March 2017
The endometrium is typically biopsied because of abnormal bleeding. Endometrial hyperplasia and endometrial carcinoma are dealt with in separate articles. An overview of gynecologic pathology is in the gynecologic pathology article.
Indications for endometrial biopsy
Abnormal bleeding:
- Abnormal uterine bleeding (AUB).
- Dysfunctional uterine bleeding, abbreviated DUB, is diagnosed if other causes of bleeding are excluded.
- DUB may get a D&C if they fail medical management.[1]
- Post-menopausal bleeding.
Other indications:[2]
- Products of conception - dealt with in a separate article.
- Dating of endometrium - infertility work-up.
Endometrial thickness on ultrasound
- A thin endometrium on ultrasound has a very low risk of malignancy.[3]
Normal microscopic findings
Endometrium - consists of:
- Epithelium (endometrial glands).
- Stroma (endometrial stroma).
In endometrial biopsies:
- Endocervical glands are commonly seen, as is endocervical mucous.
- This is 'cause the gynecologist scrapes some off on the way in or out.
Glandular telescoping
- Considered an artifact of tissue processing, i.e. normal.[4]
Image:
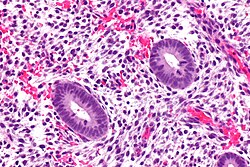
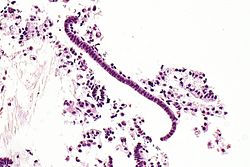
Endometrial gland compression artifact
- AKA compression artifact.
- Gland moulding.
- Tearing of tissue around the compressed glands - key feature.
- Usually at the edge of a tissue fragment.
DDx:
Image
Micro
An increased gland density is seen focally, at the edge of one tissue fragment, in association with tearing of the stroma (compression artifact).
See also
Endocervical epithelium versus endometrial epithelium
Table
| Feature | Endometrial | Endocervical | Tubal metaplasia |
|---|---|---|---|
| Cytoplasmic staining | usu. hyperchromatic +/-vacuoles | clear or light eosinophilic | hyperchromatic |
| Nucleus-to-cytoplasm ratio | moderate to high (1:2) | low (often 1:3) | high (1:1) |
| Surface features | villi | ||
| Associated stroma | cellular, hyperchromatic | inflamed, less cellular | variable |
List
Endocervical:
- Less hyperchromatic.
- Nuclei round & small.
- Cell borders usually well-defined.
Endometrial:
- More hyperchromatic.
- Nuclei columnar.
Images
Metaplasias of the endometrium
The big table of metaplasias - adapted from Nicolae et al.:[5]
| Metaplasia | Subtypes | Microscopic | Notes | Risk of malignancy | Image |
|---|---|---|---|---|---|
| Morules | - | nearly always | 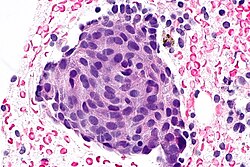
| ||
| Ciliary | - | ciliated cells | usu. lumped together with tubal, unopposed estrogen, endometriosis | frequent - endometrial hyperplasia (complex and simple), adenocarcinoma | |
| Tubal | complex, simple | ciliated cells, secretory cell, intercallary cells | usu. lumped together with ciliary, unopposed estrogen, seen in endometriosis | frequent (complex only) - endometrial hyperplasia (complex and simple), adenocarcinoma | |
| Mucinous | complex, simple | frequent (complex only) | |||
| Squamous | - | rare | |||
| Papillary syncytial change (surface) | - | rare | |||
| Eosinophilic, oxyphilic, oncocytic | not known | ||||
| Clear cell (secretory) | - | not reported | |||
| Stromal metaplasia | osseous, cartilaginous, adipose, smooth muscle, myoid, sex-cord like | not reported |
Tamoxifen effects
Inadequate endometrial biopsy
- Endometrial biopsies often have scant tissue.
- This is normal in post-menopausal women.
- Ideally, the biopsy should have some endometrial stroma.
- Without stroma it is not possible to assess the gland-to-stroma ratio.
Sign out
No stroma
ENDOMETRIUM, BIOPSY: - VERY SCANT STRIPPED NON-PROLIFERATIVE COLUMNAR EPITHELIUM, PROBABLY FROM THE LOWER UTERINE SEGMENT. - NO DEFINITE ENDOMETRIAL STROMA, SEE COMMENT. - STRIPPED ENDOCERVICAL EPITHELIUM AND ENODOCERVICAL MUCOSA WITHIN NORMAL LIMITS. - MUCOUS. COMMENT: A re-biopsy should be considered within the clinical context.
ENDOMETRIUM, BIOPSY: - VERY SCANT STRIPPED EPITHELIUM PROBABLY FROM THE LOWER UTERINE SEGMENT. - NO DEFINITE ENDOMETRIAL STROMA. - SCANT STRIPPED ENDOCERVICAL EPITHELIUM WITHIN NORMAL LIMITS. - SMALL FRAGMENTS OF DETACHED BENIGN SQUAMOUS EPITHELIUM. COMMENT: A re-biopsy should be considered within the clinical context.
ENDOMETRIUM, BIOPSY: - FRAGMENTS OF DETACHED SQUAMOUS EPITHELIUM AND DETACHED NON-PROLIFERATIVE ENDOMETRIAL GLANDS. - ASSESSMENT LIMITED AS VERY SCANT ENDOMETRIAL STROMA IS PRESENT.
ENDOMETRIUM, BIOPSY: - ENDOMETRIUM: STRIPS OF EPITHELIUM, NON-PROLIFERATIVE. - ENDOCERVIX: SCANT BENIGN EPITHELIUM. - EXOCERVIX: SCANT BENIGN EPITHELIUM. - OTHER: TUBAL METAPLASIA.
ENDOMETRIUM, BIOPSY: - STRIPS OF NON-PROLIFERATIVE ENDOMETRIUM. - SCANT BENIGN ENDOCERVICAL EPITHELIUM. - SCANT BENIGN SQUAMOUS EPITHELIUM. - TUBAL METAPLASIA.
ENDOMETRIUM, BIOPSY: - STRIPS OF BENIGN ENDOMETRIAL EPITHELIUM/TUBAL METAPLASIA, NON-PROLIFERATIVE. - SCANT BENIGN ENDOCERVICAL EPITHELIUM. - RARE SQUAMOUS METAPLASTIC CELLS.
Proliferative without definite stroma
ENDOMETRIUM, BIOPSY: - FRAGMENTS OF DETACHED SQUAMOUS EPITHELIUM, ENDOCERVICAL EPITHELIUM AND FOCALLY PROLIFERATIVE ENDOMETRIAL GLANDS. - ASSESSMENT LIMITED AS NO DEFINITE ENDOMETRIAL STROMA IS PRESENT.
Possible endometrium - insufficient
ENDOMETRIUM, ASPIRATION: - ONE MINUTE STRIP OF POSSIBLE NONPROLIFERATIVE ENDOMETRIAL EPITHELIUM, INSUFFICIENT FOR ADEQUATE DIAGNOSTIC ASSESSMENT. - VERY SCANT BENIGN STRIPPED ENDOCERVICAL EPITHELIUM. - VERY SCANT METAPLASTIC SQUAMOUS EPITHELIUM. COMMENT: Re-biopsy is advised.
ENDOMETRIUM, BIOPSY: - BENIGN STRIPPED ENDOCERVICAL EPITHELIUM AND BENIGN INFLAMED ENDOCERVICAL MUCOSA. - NO DEFINITE ENDOMETRIUM WITH STROMA, INADEQUATE SPECIMEN.
No endometrium
ENDOMETRIUM, BIOPSY: - SPECIMEN INADEQUATE; NO ENDOMETRIUM IDENTIFIED. - ONE VERY TINY FRAGMENT OF ENDOCERVICAL MUCOSA WITHOUT APPARENT PATHOLOGY.
ENDOMETRIUM, BIOPSY: - ENDOCERVICAL MUCOSA AND STRIPPED ENDOCERVICAL EPITHELIUM WITHIN NORMAL LIMITS. - MICROGLANDULAR HYPERPLASIA AND FOCAL SQUAMOUS METAPLASIA. - NO DEFINITE ENDOMETRIUM IDENTIFIED, SUGGEST RE-BIOPSY.
No tissue
ENDOMETRIUM, BIOPSY: - NO TISSUE IDENTIFIED ON MICROSCOPY.
Overview
A simple approach
Low power
- Decide whether you are looking at endometrium.
- Is the gland-to-stroma ratio normal?
- 1:3 is normal.
- If the gland-to-stroma ratio is increased... think complex endometrial hyperplasia.
- If the glands are fused to one another or cribriform... think endometrial carcinoma.
- Glands round?
- Round is normal.
- Irregular - may be seen in secretory phase endometrium, menses, disordered proliferative endometrium (focal), simple endometrial hyperplasia (diffuse).
- Glands pseudostratified?
- Pseudostratified glands are normal in the proliferative phase endometrium, hyperplasias, malignancy.
- Balls of cells?
- Blue - likely menstrual (stromal condensation).
- Pink - consider leiomyoma, squamous morules (associated with endometrial hyperplasia, endometrioid endometrial carcinoma, may be benign).
High power
- Mitoses present in the glands?
- Present in the proliferative phase, hyperplasias, malignancies.
- Mitoses present in the stroma?
- Present in the proliferative phase, hyperplasias, malignancies.
- Mucous present in the glands?
- Present in the secretory phase.
- Inflammatory cells present?
- Some are normal during menses.
Tabular summary
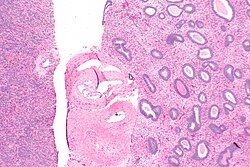
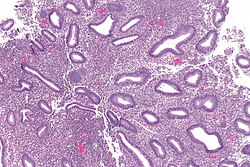
| Diagnosis | Key feature (low power) | Additional features | DDx | Other | Image |
|---|---|---|---|---|---|
| Proliferative phase endometrium | round spaced pseudostratified glands | mitoses in glands and stroma | disordered proliferative phase, simple endometrial hyperplasia, complex endometrial hyperplasia, early secretory phase endometrium | normal | |
| Secretory phase endometrium | irregular glands with secretions or simple glands with vacuoles | decidual changes (nucleus central, eosinophilic cytoplasm, well-defined cell borders) | endometrial hyperplasia with secretory changes, late proliferative phase endometrium | normal | |
| Menstrual endometrium | stromal condensation | nonproliferative glands, stromal/epithelial neutrophils, glandular cell apoptosis | disordered proliferative phase | normal | Image |
| Benign endometrial polyp | fibrous stroma, muscular blood vessels | polypoid shape (epithelium on 3 sides), +/-gland dilation | disordered proliferative endometrium (DPE), simple endometrial hyperplasia (SEH) | DPE and SEH do not occur in polyps | |
| Endometrium with changes due to exogenous hormones | decidualized stroma (nucleus central, eosinophilic cytoplasm, well-defined cell borders) | inactive glands (round/ovoid glands, simple cuboidal epithelium, no mitoses) | secretory phase endometrium, endometrial hyperplasia with secretory changes | variant of normal | |
| Atrophic endometrium | nonproliferative glands | no nuclear atypia, often without appreciable stroma | serous endometrial carcinoma | normal postmenopausal finding | |
| Disordered proliferative endometrium | proliferative focally dilated & irregular glands (usu. with tubal metaplasia) | no nuclear atypia, +/-evidence of shedding (stromal condensation) | simple endometrial hyperplasia, proliferative phase endometrium | can be thought of a waffle diagnosis |
Normal endometrium
Proliferative phase endometrium
Secretory phase endometrium
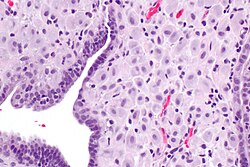
Menstrual endometrium
General
- Technically part of the proliferative phase or follicular phase.
Microscopic
Features:
- Proliferative endometrium (mitoses).[6]
- Apoptotic cells common.[7]
- Tightly packed cellular balls of stromal cells with nuclear moulding.
- Known as "blue balls".
- Tightly packed cellular stromal cells known as "stromal condensation".
- Inflammation, especially abundant neutrophils.
DDx:
- Small cell carcinoma - proliferative activity in the moulded (stromal condensation-like) cells.
- Anovulatory endometrium - less neutrophils.
Images
www:
Sign out
Endometrium, Biopsy: - Consistent with menstrual endometrium. -- Weakly proliferative endometrial glands with apoptosis, fragmented. -- Abundant balls of condensed non-proliferative endometrial stroma and blood.
Block letters
ENDOMETRIUM, BIOPSY: - CONSISTENT WITH MENSTRUAL ENDOMETRIUM: -- STRIPPED WEAKLY PROLIFERATIVE ENDOMETRIAL GLANDS. -- BALLS OF CONDENSED ENDOMETRIAL STROMA. -- ABUNDANT NEUTROPHILS AND BLOOD.
ENDOMETRIUM, BIOPSY: - CONSISTENT WITH MENSTRUAL PHASE ENDOMETRIUM: -- WEAKLY PROLIFERATIVE ENDOMETRIAL GLANDS WITH NEUTROPHILS AND APOPTOSIS. -- BALLS OF CONDENSED ENDOMETRIAL STROMA. -- BLOOD.
ENDOMETRIUM, BIOPSY: - VERY WEAKLY PROLIFERATIVE ENDOMETRIAL GLANDS WITH NEUTROPHILS AND APOPTOSIS. - BALLS OF CONDENSED ENDOMETRIAL STROMA AND BLOOD. - NEGATIVE FOR HYPERPLASIA AND NEGATIVE FOR MALIGNANCY.
Consistent with menstrual endometrium
ENDOMETRIUM, ASPIRATION: - CONSISTENT WITH MENSTRUAL ENDOMETRIUM (FRAGMENTED ENDOMETRIUM WITH PSEUDOSTRATIFIED GLANDS WITH APOPTOTIC CELLS, ABUNDANT NEUTROPHILS, CONDENSED ENDOMETRIAL STROMA AND BLOOD). - NEGATIVE FOR HYPERPLASIA AND NEGATIVE FOR MALIGNANCY.
ENDOMETRIUM, ASPIRATION: - CONSISTENT WITH MENSTRUAL ENDOMETRIUM (FRAGMENTED ENDOMETRIUM WITH SIMPLE GLANDS WITH APOPTOTIC CELLS, ABUNDANT NEUTROPHILS, CONDENSED ENDOMETRIAL STROMA (FOCAL) AND BLOOD). - NEGATIVE FOR HYPERPLASIA AND NEGATIVE FOR MALIGNANCY.
Late menses
ENDOMETRIUM, ASPIRATION: - ENDOMETRIAL GLANDS WITH APOPTOTIC CELLS, INFILTRATING NEUTROPHILS, AND GLANDULAR PROLIFERATIVE ACTIVITY. - BALLS OF CONDENSED ENDOMETRIAL STROMA. - SCANT STRIPPED ENDOCERVICAL EPITHELIUM WITHIN NORMAL LIMITS. - NEGATIVE FOR HYPERPLASIA. COMMENT: The findings are most in keeping with late menstrual endometrium.
Specific entities/abnormalities
Adipose tissue on endometrial biopsy
- AKA fat on endometrial biopsy.
General
- Benign.
- Raises the possibility of perforation - should prompt a phone call to the clinician.
Microscopic
Features:
- Adipose tissue, benign - key finding.
- Definite endometrium.
DDx:
- Extraneous tissue.
- Tissue floater.
- Pick-up.
Images
Sign out
ENDOMETRIUM, BIOPSY: - BENIGN ADIPOSE TISSUE, SEE COMMENT. - PROLIFERATIVE PHASE ENDOMETRIUM. COMMENT: The presence of adipose tissue raises the possibility of perforation. The findings were briefly discussed with Dr. Brown on November 6, 2009.
Arias-Stella reaction
- Benign atypical endometrial changes associated with chorionic tissue -- may be seen in a completely normal pregnancy and misdiagnosed as a malignancy.[8]
Endometritis
Benign endometrial polyp
Anovulatory endometrium
Disordered proliferative endometrium
- Abbreviated DPE.
- AKA endometrium with disordered proliferative phase.
- AKA disordered proliferative phase.
Endometrium with changes due to exogenous hormones
Atrophic endometrium
Ablated endometrium
Endometrium with squamous morules
Endometrium with psammoma bodies
Endometrial hyperplasia
Can be thought of as a precursor lesion for endometrial carcinoma.
It comes in two main flavours:
- Simple.
- Complex.
Each flavour may or may not have nuclear atypia.
Endometrial carcinoma
Endometrial cancer is the most common gynecologic malignancy (in the USA).[9]
See also
References
- ↑ URL: http://emedicine.medscape.com/article/257007-treatment. Accessed on: 15 July 2010.
- ↑ Mazur, Michael T.; Kurman, Robert J. (2005). Diagnosis of Endometrial Biopsies and Curettings: A Practical Approach (2nd ed.). Springer. pp. 1. ISBN 978-0387986159.
- ↑ Gambacciani, M.; Monteleone, P.; Ciaponi, M.; Sacco, A.; Genazzani, AR. (Aug 2004). "Clinical usefulness of endometrial screening by ultrasound in asymptomatic postmenopausal women.". Maturitas 48 (4): 421-4. doi:10.1016/j.maturitas.2003.10.006. PMID 15283934.
- ↑ 4.0 4.1 4.2 McCluggage, WG. (Aug 2006). "My approach to the interpretation of endometrial biopsies and curettings.". J Clin Pathol 59 (8): 801-12. doi:10.1136/jcp.2005.029702. PMID 16873562.
- ↑ Nicolae, A.; Preda, O.; Nogales, FF. (Feb 2011). "Endometrial metaplasias and reactive changes: a spectrum of altered differentiation.". J Clin Pathol 64 (2): 97-106. doi:10.1136/jcp.2010.085555. PMID 21126963.
- ↑ Tadrous, Paul.J. Diagnostic Criteria Handbook in Histopathology: A Surgical Pathology Vade Mecum (1st ed.). Wiley. pp. 237. ISBN 978-0470519035.
- ↑ Spencer, SJ.; Cataldo, NA.; Jaffe, RB. (May 1996). "Apoptosis in the human female reproductive tract.". Obstet Gynecol Surv 51 (5): 314-23. PMID 8744416.
- ↑ Arias-Stella, J. (Jan 2002). "The Arias-Stella reaction: facts and fancies four decades after.". Adv Anat Pathol 9 (1): 12-23. PMID 11756756.
- ↑ Lu KH (April 2009). "Management of early-stage endometrial cancer". Semin. Oncol. 36 (2): 137–44. doi:10.1053/j.seminoncol.2008.12.005. PMID 19332248.