Difference between revisions of "Endometritis"
| (5 intermediate revisions by the same user not shown) | |||
| Line 18: | Line 18: | ||
| Assdx = | | Assdx = | ||
| Syndromes = | | Syndromes = | ||
| Clinicalhx = | | Clinicalhx = +/-postpartum, +/-recent instrumentation | ||
| Signs = | | Signs = | ||
| Symptoms = | | Symptoms = | ||
| Line 38: | Line 38: | ||
==Microscopic== | ==Microscopic== | ||
===Acute endometritis=== | ===Acute endometritis=== | ||
Features: | Features:{{fact}} | ||
*Neutrophils clusters (>5 [[PMN]]s) in the: | *Neutrophils clusters (>5 [[PMN]]s) in the: | ||
**Endometrial stroma. | **Endometrial stroma. | ||
| Line 49: | Line 49: | ||
*[[Menstrual endometrium]] - less neutrophils. (???) | *[[Menstrual endometrium]] - less neutrophils. (???) | ||
Image | ====Kiviat definition==== | ||
Kiviat ''et al.'' definition - requires both:<ref name=pmid2137304>{{cite journal |author=Kiviat NB, Wølner-Hanssen P, Eschenbach DA, ''et al.'' |title=Endometrial histopathology in patients with culture-proved upper genital tract infection and laparoscopically diagnosed acute salpingitis |journal=Am. J. Surg. Pathol. |volume=14 |issue=2 |pages=167–75 |year=1990 |month=February |pmid=2137304 |doi= |url=}}</ref> | |||
#>=5 [[PMN]]s in surface epithelium/400x magnification field of view. | |||
#>=1 [[plasma cell]] in the endometrial stroma/120x magnification field of view. | |||
Notes: | |||
*Above definition is considered "widely accepted".<ref name=pmid>{{cite journal |author=Ross JD |title=What is endometritis and does it require treatment? |journal=Sex Transm Infect |volume=80 |issue=4 |pages=252–3 |year=2004 |month=August |pmid=15295119 |pmc=1744883 |doi=10.1136/sti.2004.009548 |url=}}</ref> | |||
*Definition suffers from [[HPFitis]] and [[IPFitis]]. | |||
====Image==== | |||
*[http://www.hsc.stonybrook.edu/gyn-atlas/UT53.10.1.htm Acute endometritis (stonybrook.edu)]. | *[http://www.hsc.stonybrook.edu/gyn-atlas/UT53.10.1.htm Acute endometritis (stonybrook.edu)]. | ||
| Line 66: | Line 75: | ||
Notes: | Notes: | ||
*One [[plasma cell]] is not enough to call it. | *One [[plasma cell]] is not enough to call it.<ref name=pmid21996319>{{cite journal |author=Vicetti Miguel RD, Chivukula M, Krishnamurti U, ''et al.'' |title=Limitations of the criteria used to diagnose histologic endometritis in epidemiologic pelvic inflammatory disease research |journal=Pathol. Res. Pract. |volume=207 |issue=11 |pages=680–5 |year=2011 |month=November |pmid=21996319 |pmc=3215901 |doi=10.1016/j.prp.2011.08.007 |url=}}</ref><ref name=pmid16873562>{{Cite journal | last1 = McCluggage | first1 = WG. | title = My approach to the interpretation of endometrial biopsies and curettings. | journal = J Clin Pathol | volume = 59 | issue = 8 | pages = 801-12 | month = Aug | year = 2006 | doi = 10.1136/jcp.2005.029702 | PMID = 16873562 }}</ref> | ||
DDx: | DDx: | ||
Latest revision as of 17:52, 3 July 2014
| Endometritis | |
|---|---|
| Diagnosis in short | |
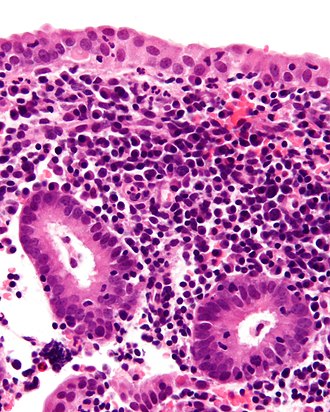 Chronic endometritis. H&E stain. | |
|
| |
| LM |
acute: abundant neutrophils, clusters >5 (in stroma & glands); chronic: plasma cells (key feature), often eosinophils, lymphoid aggregates |
| Subtypes | acute, chronic |
| LM DDx | menstrual endometrium |
| Site | endometrium |
|
| |
| Clinical history | +/-postpartum, +/-recent instrumentation |
| Prevalence | uncommon |
| Prognosis | benign |
Endometritis is inflammation of the endometrium. It usually subdivided into acute and chronic.
General
- Usually post-delivery or post-instrumentation, e.g. previous biopsy.
- May be spontaneous, e.g. tuberculous endometritis.
Microscopic
Acute endometritis
Features:[citation needed]
- Neutrophils clusters (>5 PMNs) in the:
- Endometrial stroma.
- Within uterine glands.
Notes:
- Neutrophils are normal in the context of menses.
DDx:
- Menstrual endometrium - less neutrophils. (???)
Kiviat definition
Kiviat et al. definition - requires both:[1]
- >=5 PMNs in surface epithelium/400x magnification field of view.
- >=1 plasma cell in the endometrial stroma/120x magnification field of view.
Notes:
Image
Chronic endometritis
Features:[3]
- Plasma cells with in the endometrial stroma - key feature.
- Usually superficial/close to the luminal aspect.
- Lymphocytic infiltrate - usually marked.
- May form lymphoid aggregates - low power finding.
- +/-Eosinophils - presence should prompt a search for plasma cells.[4]
Other findings:[3]
- +/-Necrosis.
- Edema - common.
- Hemorrhage.
Notes:
- One plasma cell is not enough to call it.[5][6]
DDx:
- Menstrual endometrium - endometrial stromal condensation.
Images
www:
- Chronic endometritis (webpathology.com).
- Chronic endometritis (webpathology.com).
- Tuberculous endometritis (webpathology.com).
Sign out
ENDOMETRIUM, BIOPSY: - CHRONIC ENDOMETRITIS.
Not definite endometritis
ENDOMETRIUM, ASPIRATION: - PROLIFERATIVE PHASE ENDOMETRIUM WITH A MILD LYMPHOCYTIC INFILTRATE AND VERY RARE PLASMA CELLS, SEE COMMENT. - NEGATIVE FOR HYPERPLASIA. COMMENT: The lymphocytic infiltrate and plasma cells raise the possibility of a mild chronic endometritis; clinical correlation is suggested.
Nonspecific lymphocytic infiltrate
If not more than one plasma cell is apparent after searching.
ENDOMETRIUM, ASPIRATION: - PROLIFERATIVE PHASE ENDOMETRIUM WITH A MILD LYMPHOCYTIC INFILTRATE. - SMALL FRAGMENT OF ENDOCERVICAL MUCOSA WITHIN NORMAL LIMITS. - NEGATIVE FOR HYPERPLASIA.
Micro
The section show proliferative endometrium with a normal gland-to-stroma ratio. Mitotic activity is seen in the glands and stroma. No cytologic atypia is apparent. A mild nonspecific lymphocytic infiltrate is present.
No lymphoid aggregates are apparent. No eosinophils are apparent. No significant number of plasma cells is apparent.
Alternate
The sections show a fragmented nonproliferative endometrium with stromal decidualization and focal glandular dilation. The gland-to-stroma ratio is within normal limits. No cytologic atypia is apparent.
Lymphoid aggregates are present. Focally, rare eosinophils are identified. No significant number of plasma cells is apparent.
See also
References
- ↑ Kiviat NB, Wølner-Hanssen P, Eschenbach DA, et al. (February 1990). "Endometrial histopathology in patients with culture-proved upper genital tract infection and laparoscopically diagnosed acute salpingitis". Am. J. Surg. Pathol. 14 (2): 167–75. PMID 2137304.
- ↑ Ross JD (August 2004). "What is endometritis and does it require treatment?". Sex Transm Infect 80 (4): 252–3. doi:10.1136/sti.2004.009548. PMC 1744883. PMID 15295119. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1744883/.
- ↑ 3.0 3.1 Tawfik, O.; Venuti, S.; Brown, S.; Collins, J. (1996). "Immunohistochemical characterization of leukocytic subpopulations in chronic endometritis.". Infect Dis Obstet Gynecol 4 (5): 287-93. doi:10.1155/S1064744996000555. PMC 2364507. PMID 18476109. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2364507/.
- ↑ Adegboyega, PA.; Pei, Y.; McLarty, J. (Jan 2010). "Relationship between eosinophils and chronic endometritis.". Hum Pathol 41 (1): 33-7. doi:10.1016/j.humpath.2009.07.008. PMID 19801162.
- ↑ Vicetti Miguel RD, Chivukula M, Krishnamurti U, et al. (November 2011). "Limitations of the criteria used to diagnose histologic endometritis in epidemiologic pelvic inflammatory disease research". Pathol. Res. Pract. 207 (11): 680–5. doi:10.1016/j.prp.2011.08.007. PMC 3215901. PMID 21996319. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3215901/.
- ↑ McCluggage, WG. (Aug 2006). "My approach to the interpretation of endometrial biopsies and curettings.". J Clin Pathol 59 (8): 801-12. doi:10.1136/jcp.2005.029702. PMID 16873562.