Difference between revisions of "Endometriosis"
Jump to navigation
Jump to search
| (9 intermediate revisions by the same user not shown) | |||
| Line 8: | Line 8: | ||
| LMDDx = [[adenocarcinoma]], [[endosalpingiosis]] | | LMDDx = [[adenocarcinoma]], [[endosalpingiosis]] | ||
| Stains = | | Stains = | ||
| IHC = CD10 +ve (stroma) | | IHC = CK7 +ve, ER +ve, [[CD10]] +ve (stroma), CK20 -ve, CDX2 -ve | ||
| EM = | | EM = | ||
| Molecular = | | Molecular = | ||
| Line 21: | Line 21: | ||
| Symptoms = +/-pelvic pain, +/-deep dyspareunia | | Symptoms = +/-pelvic pain, +/-deep dyspareunia | ||
| Prevalence = common | | Prevalence = common | ||
| Bloodwork = CA-125 mildly elevated | | Bloodwork = [[CA-125]] mildly elevated | ||
| Rads = | | Rads = | ||
| Endoscopy = | | Endoscopy = | ||
| Line 74: | Line 74: | ||
*Endometriosis can appear almost any where. | *Endometriosis can appear almost any where. | ||
**A well-reported uncommon location is the abdominal wall post-caesarian section.<ref name=pmid22381104>{{Cite journal | last1 = Ozel | first1 = L. | last2 = Sagiroglu | first2 = J. | last3 = Unal | first3 = A. | last4 = Unal | first4 = E. | last5 = Gunes | first5 = P. | last6 = Baskent | first6 = E. | last7 = Aka | first7 = N. | last8 = Titiz | first8 = MI. | last9 = Tufekci | first9 = EC. | title = Abdominal wall endometriosis in the cesarean section surgical scar: a potential diagnostic pitfall. | journal = J Obstet Gynaecol Res | volume = 38 | issue = 3 | pages = 526-30 | month = Mar | year = 2012 | doi = 10.1111/j.1447-0756.2011.01739.x | PMID = 22381104 }}</ref> | **A well-reported uncommon location is the abdominal wall post-caesarian section.<ref name=pmid22381104>{{Cite journal | last1 = Ozel | first1 = L. | last2 = Sagiroglu | first2 = J. | last3 = Unal | first3 = A. | last4 = Unal | first4 = E. | last5 = Gunes | first5 = P. | last6 = Baskent | first6 = E. | last7 = Aka | first7 = N. | last8 = Titiz | first8 = MI. | last9 = Tufekci | first9 = EC. | title = Abdominal wall endometriosis in the cesarean section surgical scar: a potential diagnostic pitfall. | journal = J Obstet Gynaecol Res | volume = 38 | issue = 3 | pages = 526-30 | month = Mar | year = 2012 | doi = 10.1111/j.1447-0756.2011.01739.x | PMID = 22381104 }}</ref> | ||
*Intraluminal endometriosis in the Fallopian tube - is relatively common,<ref>{{cite journal |authors=Hill CJ, Fakhreldin M, Maclean A, Dobson L, Nancarrow L, Bradfield A, Choi F, Daley D, Tempest N, Hapangama DK |title=Endometriosis and the Fallopian Tubes: Theories of Origin and Clinical Implications |journal=J Clin Med |volume=9 |issue=6 |pages= |date=June 2020 |pmid=32570847 |pmc=7355596 |doi=10.3390/jcm9061905 |url=}}</ref> it may be less obvious to the surgeon. | |||
===Images=== | |||
<gallery> | |||
Image: Endometriosis,_abdominal_wall.jpg |Endometriosis in C-section scar at cut-up. (Ed Uthman/WC) | |||
</gallery> | |||
==Microscopic== | ==Microscopic== | ||
| Line 89: | Line 95: | ||
DDx: | DDx: | ||
*[[Adenocarcinoma]]. | *[[Adenocarcinoma]] - especially colorectal adenocarcinoma. | ||
*[[Endosalpingiosis]] - does not have stromal component. | *[[Endosalpingiosis]] - does not have stromal component. | ||
**In the GI tract, it classically expands the muscularis propria. | **In the GI tract, it classically expands the muscularis propria. | ||
| Line 109: | Line 115: | ||
==Immunohistochemical stains== | ==Immunohistochemical stains== | ||
Features:<ref>{{cite journal |authors=Jiang W, Roma AA, Lai K, Carver P, Xiao SY, Liu X |title=Endometriosis involving the mucosa of the intestinal tract: a clinicopathologic study of 15 cases |journal=Mod Pathol |volume=26 |issue=9 |pages=1270–8 |date=September 2013 |pmid=23579618 |doi=10.1038/modpathol.2013.51 |url=}}</ref> | |||
*ER +ve | *ER +ve | ||
*CK7 +ve | **Stains the epithelium. | ||
*[[CK20]] -ve - | *[[CK7]] +ve | ||
**Stains the epithelium. | |||
*[[CK20]] -ve | |||
**Used to exclude [[colorectal adenocarcinoma]]. | |||
*CDX2 -ve. | |||
**Used to exclude [[colorectal adenocarcinoma]]. | |||
*[[CD10]] +ve | |||
**Marks the stromal cells.<ref name=Ref_DCHH236>{{Ref DCHH|236}}</ref> | |||
==Sign out== | ==Sign out== | ||
Latest revision as of 14:51, 16 December 2024
| Endometriosis | |
|---|---|
| Diagnosis in short | |
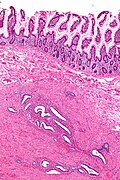
 Endometriosis of the ovary. H&E stain. | |
|
| |
| LM | at least 2 of 3: (1) endometrial glands, (2) endometrial stroma, (3) hemosiderin-laden macrophages |
| LM DDx | adenocarcinoma, endosalpingiosis |
| IHC | CK7 +ve, ER +ve, CD10 +ve (stroma), CK20 -ve, CDX2 -ve |
| Gross | chocolate cyst |
| Site | ovary, uterine ligaments, cul-de-sac, peritoneum, cervix, vagina, fallopian tubes, surgical scars, gastrointestinal tract |
|
| |
| Associated Dx | infertility, endometrioid adenocarcinoma of the ovary, clear cell adenocarcinoma of the ovary, seromucinous borderline tumour |
| Symptoms | +/-pelvic pain, +/-deep dyspareunia |
| Prevalence | common |
| Blood work | CA-125 mildly elevated |
| Prognosis | benign |
Endometriosis causes significant morbidity and is associated with increased risk of certain malignancies.
General
Pathophysiology
There are several theories for endometriosis, i.e. how it is that endometrial tissue gets found outside of the uterus:
- Retrograde menstruation - probably the most common.[1]
- Ectopic endometrial tissue.[2]
- Coelomic metaplasia.
- Hematogenous spread or lymphatic spread.
Clinical
- Associated with infertility.
- Pelvic pain.
- Deep dyspareunia.
- Affects approximately 10% of women of child bearing age.
- Associated with moderate elevation of (serum) CA-125.
Tumours associated with endometriosis
Endometriosis is associated with gynecologic tumours:
- Endometrioid adenocarcinoma of the ovary.[3]
- Clear cell carcinoma of the ovary.[4]
- Endocervical-like mucinous borderline tumour (EMBT).[5]
- Mixture of EMBT and serous borderline tumor = seromucinous borderline tumour.
Other tumours & decreased risk:[6]
- Increased: endocrine tumours, non-Hodgkin's lymphoma, brain tumours.
- Decreased: cervical cancer.
Rare stuff:
- There are case reports of endometriosis in men on estrogen therapy for prostate cancer.[7][8]
Gross
Appearance:
- Chocolate cyst = cyst containing light brown material.
Classic locations:
- Ovary - most common location according to Jenkins et al.[1]
- Utero-sacral ligament.[9]
- Cul-de-sac.[9]
- Broad ligament.
Note:
- The hierarchy of the most common sites, i.e. what is most common and what is the second most common etc., depends on the paper one reads, e.g. compare Jenkins et al[1] with Stegmann et al.[9]
- Robbins gives the order as: ovaries, uterine ligaments, rectovaginal septum, cul-de-sac, pelvic periteoneum, gastrointestinal tract, cervix, vagina, fallopian tubes, laparotomy scars.[10]
- Endometriosis can appear almost any where.
- A well-reported uncommon location is the abdominal wall post-caesarian section.[11]
- Intraluminal endometriosis in the Fallopian tube - is relatively common,[12] it may be less obvious to the surgeon.
Images
Microscopic
Criteria - need at least 2 / 3 for the diagnosis:[13]
- Endometrial glands - endometrial glands are classically: circular, with nuclei that are hyperchromatic & cigar-shaped.
- Endometrial stroma - endometrial stroma is classically: cellular and hyperchromatic (may resemble a lymphocytic infiltration on low power).
- Hemosiderin-laden macrophages - light brown, may be granular.
Notes:
- The epithelial component (1) may appear cuboidal in cysts or be sloughed-off, i.e. absent.
- The microscopic correlation of chocolate cyst is: light brown acellular material; this can be considered as a substitute for (3) - hemosiderin-laden macrophages.
- Epithelial component may have tubal metaplasia.[14]
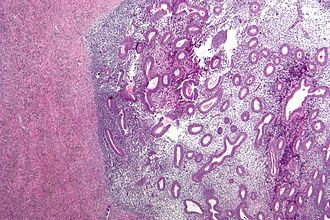
- Endometriosis may mimic cancer[15] - see images below.
- If it is just endometrial type glands - the stroma is missing... it is probably endosalpingiosis.
DDx:
- Adenocarcinoma - especially colorectal adenocarcinoma.
- Endosalpingiosis - does not have stromal component.
- In the GI tract, it classically expands the muscularis propria.
Images
Mimicking cancer:
www:
Immunohistochemical stains
Features:[16]
- ER +ve
- Stains the epithelium.
- CK7 +ve
- Stains the epithelium.
- CK20 -ve
- Used to exclude colorectal adenocarcinoma.
- CDX2 -ve.
- Used to exclude colorectal adenocarcinoma.
- CD10 +ve
- Marks the stromal cells.[17]
Sign out
Biopsy
OVARIAN FOSSA, RIGHT, BIOPSY: - ENDOMETRIOSIS. - FIBROADIPOSE TISSUE PARTIALLY COVERED BY MESOTHELIUM.
CYST WALL, OVARY LEFT, CYSTECTOMY: - ENDOMETRIOSIS.
CUL-DE-SAC, BIOPSY: - ENDOMETRIOSIS. COMMENT: A CD10 immunostain marks the endometrial-type stroma and confirms the presence of endometriosis.
Ovary and tube
OVARY AND FALLOPIAN TUBE, LEFT, SALPINO-OOPHORECTOMY: - OVARY WITH ENDOMETRIOSIS. - FALLOPIAN TUBE WITHIN NORMAL LIMITS. - NEGATIVE FOR MALIGNANCY.
TAH-USO
UTERUS, UTERINE TUBES, LEFT OVARY, TOTAL HYSTERECTOMY, BILATERAL SALPINGECTOMY AND LEFT OOPHRECTOMY: - LEIOMYOMATA WITH HYALINE CHANGE. - NONPROLIFERATIVE ENDOMETRIAL GLANDS WITH STROMAL DECIDUALIZATION, AND GLANDULAR DILATION. - LEFT OVARY WITH ENDOMETRIOSIS, SEE COMMENT. - LEFT UTERINE TUBE WITH ENDOMETRIOSIS, SEE COMMENT. - RIGHT UTERINE TUBE WITHIN NORMAL LIMITS. - UTERINE CERVIX WITHIN NORMAL LIMITS. - NEGATIVE FOR MALIGNANCY. COMMENT: The presence of endometrial stroma was demonstrated with CD10 immunostaining, thus confirming the presence of endometriosis.
TAH-BSO
UTERINE CERVIX, UTERUS, UTERINE TUBES AND OVARIES, TOTAL HYSTERECTOMY AND BILATERAL SALPINGOOPHERECTOMY: - UTERINE CERVIX WITHIN NORMAL LIMITS. - PROLIFERATIVE PHASE ENDOMETRIUM. - UTERUS WITH FIBROUS SEROSAL ADHESIONS. - LEFT UTERINE TUBE WITH ENDOMETRIOSIS. - RIGHT UTERINE TUBE WITHIN NORMAL LIMITS. - RIGHT AND LEFT OVARIES WITH ENDOMETRIOSIS.
Soft tissue abdominal wall mass
MASS, RIGHT LOWER ABDOMEN, EXCISION: - ENDOMETRIOMA. - SCAR. COMMENT: Immunostains confirm the presence of endometriosis (glandular component ER positive, endometrial-like stroma CD10 positive).
Micro
The sections show soft tissue with endometrial-type glands surrounded by endometrial-type stroma. Siderophages are present. No nuclear atypia is identified. Mitotic activity is not apparent.
See also
References
- ↑ 1.0 1.1 1.2 Jenkins, S.; Olive, DL.; Haney, AF. (Mar 1986). "Endometriosis: pathogenetic implications of the anatomic distribution.". Obstet Gynecol 67 (3): 335-8. PMID 3945444.
- ↑ Signorile, PG.; Baldi, F.; Bussani, R.; D'Armiento, M.; De Falco, M.; Baldi, A. (2009). "Ectopic endometrium in human foetuses is a common event and sustains the theory of müllerianosis in the pathogenesis of endometriosis, a disease that predisposes to cancer.". J Exp Clin Cancer Res 28: 49. doi:10.1186/1756-9966-28-49. PMID 19358700.
- ↑ Nagle CM, Olsen CM, Webb PM, Jordan SJ, Whiteman DC, Green AC (November 2008). "Endometrioid and clear cell ovarian cancers: a comparative analysis of risk factors". Eur. J. Cancer 44 (16): 2477-84. doi:10.1016/j.ejca.2008.07.009. PMID 18707869.
- ↑ Kawaguchi R, Tsuji Y, Haruta S, et al. (October 2008). "Clinicopathologic features of ovarian cancer in patients with ovarian endometrioma". J. Obstet. Gynaecol. Res. 34 (5): 872–7. doi:10.1111/j.1447-0756.2008.00849.x. PMID 18834345.
- ↑ Moriya T, Mikami Y, Sakamoto K, et al. (December 2003). "Endocervical-like mucinous borderline tumors of the ovary: clinicopathological features and electron microscopic findings". Med Electron Microsc 36 (4): 240–6. doi:10.1007/s00795-003-0221-4. PMID 16228656.
- ↑ URL: http://www.medicalnewstoday.com/articles/3890.php. Accessed on: 26 September 2011.
- ↑ Fukunaga, M. (Jan 2012). "Paratesticular endometriosis in a man with a prolonged hormonal therapy for prostatic carcinoma.". Pathol Res Pract 208 (1): 59-61. doi:10.1016/j.prp.2011.10.007. PMID 22104297.
- ↑ Beckman, EN.; Pintado, SO.; Leonard, GL.; Sternberg, WH. (May 1985). "Endometriosis of the prostate.". Am J Surg Pathol 9 (5): 374-9. PMID 2418693.
- ↑ 9.0 9.1 9.2 Stegmann, BJ.; Sinaii, N.; Liu, S.; Segars, J.; Merino, M.; Nieman, LK.; Stratton, P. (Jun 2008). "Using location, color, size, and depth to characterize and identify endometriosis lesions in a cohort of 133 women.". Fertil Steril 89 (6): 1632-6. doi:10.1016/j.fertnstert.2007.05.042. PMID 17662280.
- ↑ Mitchell, Richard; Kumar, Vinay; Fausto, Nelson; Abbas, Abul K.; Aster, Jon (2011). Pocket Companion to Robbins & Cotran Pathologic Basis of Disease (8th ed.). Elsevier Saunders. pp. 524. ISBN 978-1416054542.
- ↑ Ozel, L.; Sagiroglu, J.; Unal, A.; Unal, E.; Gunes, P.; Baskent, E.; Aka, N.; Titiz, MI. et al. (Mar 2012). "Abdominal wall endometriosis in the cesarean section surgical scar: a potential diagnostic pitfall.". J Obstet Gynaecol Res 38 (3): 526-30. doi:10.1111/j.1447-0756.2011.01739.x. PMID 22381104.
- ↑ Hill CJ, Fakhreldin M, Maclean A, Dobson L, Nancarrow L, Bradfield A, Choi F, Daley D, Tempest N, Hapangama DK (June 2020). "Endometriosis and the Fallopian Tubes: Theories of Origin and Clinical Implications". J Clin Med 9 (6). doi:10.3390/jcm9061905. PMC 7355596. PMID 32570847. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7355596/.
- ↑ Tadrous, Paul.J. Diagnostic Criteria Handbook in Histopathology: A Surgical Pathology Vade Mecum (1st ed.). Wiley. pp. 239. ISBN 978-0470519035.
- ↑ Clement PB (July 2007). "The pathology of endometriosis: a survey of the many faces of a common disease emphasizing diagnostic pitfalls and unusual and newly appreciated aspects". Adv Anat Pathol 14 (4): 241–60. doi:10.1097/PAP.0b013e3180ca7d7b. PMID 17592255.
- ↑ Corben, AD.; Nehhozina, T.; Garg, K.; Vallejo, CE.; Brogi, E. (Aug 2010). "Endosalpingiosis in axillary lymph nodes: a possible pitfall in the staging of patients with breast carcinoma.". Am J Surg Pathol 34 (8): 1211-6. doi:10.1097/PAS.0b013e3181e5e03e. PMID 20631604.
- ↑ Jiang W, Roma AA, Lai K, Carver P, Xiao SY, Liu X (September 2013). "Endometriosis involving the mucosa of the intestinal tract: a clinicopathologic study of 15 cases". Mod Pathol 26 (9): 1270–8. doi:10.1038/modpathol.2013.51. PMID 23579618.
- ↑ Tadrous, Paul.J. Diagnostic Criteria Handbook in Histopathology: A Surgical Pathology Vade Mecum (1st ed.). Wiley. pp. 236. ISBN 978-0470519035.