Difference between revisions of "Bone"
m (→Bone marrow) |
m (image) |
||
| (104 intermediate revisions by one other user not shown) | |||
| Line 3: | Line 3: | ||
Tumours often spread to bone and occasionally arise in bone. Bone tumours are dealt with in the ''[[bone tumours]]'' article. | Tumours often spread to bone and occasionally arise in bone. Bone tumours are dealt with in the ''[[bone tumours]]'' article. | ||
== | =Normal bone= | ||
* | ==Bone anatomy== | ||
** | *Epiphysis = rounded end of the bone. | ||
*Metaphysis = between epiphysis and diaphysis; contains ''epiphyseal plate'' - site of growth in childhood. | |||
*Diaphysis = shaft, mid-portion, contains [[bone marrow]]. | |||
*Osteoblasts | ===Image=== | ||
*Osteoclasts | <gallery> | ||
Image:EpiMetaDiaphyse.jpg | Bone. (WC) | |||
</gallery> | |||
==Bone histology== | |||
Two types (based on arrangement of collagen): | |||
# Woven bone. | |||
# Lamellar bone. | |||
===Woven bone=== | |||
*Always abnormal in adults. | |||
*Collagen arranged haphazardly - mechanically weak. | |||
Images: | |||
*[http://www.ajnr.org/cgi/content-nw/full/27/2/274/F4 Woven bone (ajnr.org)].<ref name=pmid16484391>{{cite journal |author=Lin DD, Gailloud P, McCarthy EF, Comi AM |title=Oromaxillofacial osseous abnormality in Sturge-Weber syndrome: case report and review of the literature |journal=AJNR Am J Neuroradiol |volume=27 |issue=2 |pages=274–7 |year=2006 |month=February |pmid=16484391 |doi= |url=}}</ref> | |||
*[http://www.brown.edu/Courses/Digital_Path/systemic_path/bone/paget.html Woven bone (brown.edu)]. | |||
===Lamellar bone=== | |||
[[File:Lamella bone H&E and under polarised light.gif|thumb|Animated GIF showing a photomicrograph of lamellar bone. The layers are accentuated under polarised light.]] | |||
*Collagen organized in layers (lamellae). | |||
===Woven versus lamellar=== | |||
*Easiest way to differentiate: polarize; lamellar bone has well-defined layers. | |||
==Bone cells== | |||
*Osteocytes. | |||
**Sit in lacunae. | |||
***Empty lacunae = necrotic bone. | |||
*Osteoblasts. | |||
**Make bone. | |||
*Osteoclasts. | |||
**Destroy bone. | |||
**Multinucleated. | |||
Memory device: 'b' before 'c'. | Memory device: 'b' before 'c'. | ||
==Bone marrow== | ==Bone marrow== | ||
{{Main|Haematopoiesis}} | {{Main|Haematopoiesis}} | ||
* | ===General=== | ||
*One of two ''[[primary lymphoid organs]]'' - the other one is the [[thymus]].<ref>URL: [http://www.life.umd.edu/classroom/bsci423/song/Lab1.html http://www.life.umd.edu/classroom/bsci423/song/Lab1.html]. Accessed on: 28 March 2012.</ref> | |||
Bone marrow biopsy adequacy:<ref name=pmid16477878>{{Cite journal | last1 = Rudzki | first1 = Z. | last2 = Partyła | first2 = T. | last3 = Okoń | first3 = K. | last4 = Stachura | first4 = J. | title = Adequacy of trephine bone marrow biopsies: the doctor and the patient make a difference. | journal = Pol J Pathol | volume = 56 | issue = 4 | pages = 187-95 | month = | year = 2005 | doi = | PMID = 16477878 }}</ref> | |||
*10 intertrabecular spaces or 10 mm. | |||
===Microscopic=== | |||
One should see three cell lines:<ref>URL: [http://emedicine.medscape.com/article/199003-overview http://emedicine.medscape.com/article/199003-overview]. Accessed on: 28 March 2012.</ref> | |||
#Erythroid (red cells). | |||
#Myeloid (white blood cells). | |||
#Megakaryocytic (platelets). | |||
Adipose tissue: | |||
*Fat content (%) ~= age in years.<ref>IAV. 26 Feb 2009.</ref> | |||
**e.g. 60 year old will have 60% fatty replacement. | |||
Identifying the lines:<ref>[http://upload.wikimedia.org/wikipedia/commons/6/69/Hematopoiesis_%28human%29_diagram.png http://upload.wikimedia.org/wikipedia/commons/6/69/Hematopoiesis_%28human%29_diagram.png]</ref> | Identifying the cell lines:<ref>[http://upload.wikimedia.org/wikipedia/commons/6/69/Hematopoiesis_%28human%29_diagram.png http://upload.wikimedia.org/wikipedia/commons/6/69/Hematopoiesis_%28human%29_diagram.png]</ref> | ||
#Megakaryocytes: | #Megakaryocytes: | ||
#*Big cells ~ 3x the size of a RBC. | #*Big cells ~ 3x the size of a [[RBC]]. | ||
# | #[[Normoblast]]s (RBC precursors): | ||
#*Hyperchromatic, i.e. blue, nucleus. | #*Hyperchromatic, i.e. blue, nucleus. | ||
#Myeloid line: | #Myeloid line: | ||
| Line 38: | Line 73: | ||
#*Reniform nucleus, i.e. kidney bean shaped nucleus. | #*Reniform nucleus, i.e. kidney bean shaped nucleus. | ||
Note: | |||
*[http:// | *Lymphocytes are considered separately and typically spared in bone marrow failure.<ref>[http://emedicine.medscape.com/article/199003-overview http://emedicine.medscape.com/article/199003-overview]</ref> | ||
====Organization==== | ====Organization==== | ||
*Mature hematopoeitic cells at the centre (distant from bone). | *Mature hematopoeitic cells at the centre (distant from bone). | ||
*Immature hematopoeitic cells adjacent to the bone. | *Immature hematopoeitic cells adjacent to the bone. | ||
== | Note: | ||
=== | *Immediately adjacent to the bone (paratrabecular)... is where [[follicular lymphoma]] is classically found.<ref name=pmid17284114>{{Cite journal | last1 = Iancu | first1 = D. | last2 = Hao | first2 = S. | last3 = Lin | first3 = P. | last4 = Anderson | first4 = SK. | last5 = Jorgensen | first5 = JL. | last6 = McLaughlin | first6 = P. | last7 = Medeiros | first7 = LJ. | title = Follicular lymphoma in staging bone marrow specimens: correlation of histologic findings with the results of flow cytometry immunophenotypic analysis. | journal = Arch Pathol Lab Med | volume = 131 | issue = 2 | pages = 282-7 | month = Feb | year = 2007 | doi = 10.1043/1543-2165(2007)131[282:FLISBM]2.0.CO;2 | PMID = 17284114 }}</ref> | ||
General | **Image: [http://www.flickr.com/photos/euthman/5691578596/in/set-72057594114099781 Paratrabecular follicular lymphoma (flickr.com)]. | ||
===Images=== | |||
<gallery> | |||
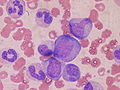
Image:Bone_marrow_WBC.JPG| Myeloid line. (WC) | |||
</gallery> | |||
===Sign out=== | |||
====Essentially normal==== | |||
<pre> | |||
Bone Marrow, Posterior Superior Iliac Spine, Biopsy: | |||
- Bone marrow with trilineage hematopoiesis. | |||
- Cellularity within normal limits for age. | |||
- Case will be sent to hematology for consultation and correlation | |||
with other testing. | |||
</pre> | |||
====Inadequate==== | |||
<pre> | |||
Right Posterior Superior Iliac Spine, Bone Marrow Biopsy: | |||
- Predominantly benign dense fibrous tissue with a small | |||
amount of laminar bone, and minute fragment of marrow (<2 mm). | |||
- Case will be sent to hematopathology for further assessment. | |||
</pre> | |||
=Benign variants= | |||
==Hyperostosis frontalis interna== | |||
*Extra-thick frontal bone.<ref>URL: [http://radiopaedia.org/articles/hyperostosis_frontalis_interna http://radiopaedia.org/articles/hyperostosis_frontalis_interna]. Accessed on: 29 September 2010.</ref> | |||
*No clinical significance -- just has to be recognized as a "nothing". | |||
=Infections= | |||
==Acute osteomyelitis== | |||
===General=== | |||
Pathophysiology/entry: | |||
*Hematogenous - often in children. | *Hematogenous - often in children. | ||
*Direct entry (skin defect) - adults with diabetes. | *Direct entry (skin defect) - adults with diabetes. | ||
==== | ===Microscopic=== | ||
* | Features: | ||
*[[PMN]]s. | |||
*Micro-organisms - esp. cocci. | |||
Image: | |||
*[http://osteomyelitis.stanford.edu/pages/histo_002.html Acute osteomyeelitis (stanford.edu)]. | |||
===Stains=== | |||
*[[Gram stain]]. | |||
=== | ==Chronic osteomyelitis== | ||
*Plasma cells. | ===General=== | ||
Most common organism: | |||
*''Staphylococcus aureus''.<ref name=pmid22046943>{{Cite journal | last1 = Hatzenbuehler | first1 = J. | last2 = Pulling | first2 = TJ. | title = Diagnosis and management of osteomyelitis. | journal = Am Fam Physician | volume = 84 | issue = 9 | pages = 1027-33 | month = Nov | year = 2011 | doi = | PMID = 22046943 | URL = http://www.aafp.org/link_out?pmid=22046943 }}</ref> | |||
Risk factors:<ref name=pmid22046943/> | |||
*[[Diabetes mellitus]]. | |||
*Peripheral vascular disease. | |||
===Microscopic=== | |||
Features: | |||
*Plasma cells - '''key feature'''. | |||
**May be sterile, i.e. no organisms. | **May be sterile, i.e. no organisms. | ||
*+/-Fibrosis. | |||
*+/-Necrotic bone - bone with empty lacunae. | |||
*+/-[[Amyloid]]. | |||
**~10% of patients in one series.<ref name=pmid2071276>{{Cite journal | last1 = Alabi | first1 = ZO. | last2 = Ojo | first2 = OS. | last3 = Odesanmi | first3 = WO. | title = Secondary amyloidosis in chronic osteomyelitis. | journal = Int Orthop | volume = 15 | issue = 1 | pages = 21-2 | month = | year = 1991 | doi = | PMID = 2071276 }}</ref> | |||
Image: | |||
*[http://osteomyelitis.stanford.edu/pages/histo_001.html Chronic osteomyelitis (stanford.edu)]. | |||
===Sign out=== | |||
<pre> | |||
LOWER LEG, RIGHT, BELOW KNEE AMPUTATION: | |||
- ACUTE AND CHRONIC OSTEOMYELITIS. | |||
- MODERATE ATHEROSCLEROSIS. | |||
- SKIN ULCERATION. | |||
- SOFT TISSUE SURGICAL MARGIN WITH FAT NECROSIS AND MUSCULAR ATROPHY. | |||
- NEGATIVE FOR MALIGNANCY. | |||
</pre> | |||
<pre> | |||
TRAPEZIUM, RIGHT HAND, REMOVAL: | |||
- DEGENERATIVE JOINT DISEASE. | |||
- MARROW SPACE WITH FIBROSIS AND SCATTERED LYMPHOCYTES AND PLASMA CELLS, | |||
COMPATIBLE WITH MILD CHRONIC OSTEOMYELITIS. | |||
- NO MICROORGANISMS APPARENT WITH ROUTINE STAINS. | |||
- NEGATIVE FOR MALIGNANCY. | |||
</pre> | |||
=Bone tumours= | |||
{{Main|Bone tumours}} | {{Main|Bone tumours}} | ||
This is a big topic. It is dealt with in a separate article. | This is a big topic. It is dealt with in a separate article. | ||
| Line 64: | Line 174: | ||
The bone tumour article covers tumour mimics, e.g. brown cell tumour. | The bone tumour article covers tumour mimics, e.g. brown cell tumour. | ||
=Fractures= | |||
{{Main| | {{Main|Bone fractures}} | ||
This is dealt with in the ''forensic pathology'' article. | This is dealt with in the ''forensic pathology'' article. | ||
==See also= | =Others= | ||
The following is a collection of stuff that doesn't really fit in another category or is just weird. | |||
A general DDx for cystic bone lesions is found on ''radipedia.com''.<ref>URL: [http://radipedia.com/WikiMedia/index.php?title=Benign_cystic_bone_lesions http://radipedia.com/WikiMedia/index.php?title=Benign_cystic_bone_lesions]. Accessed on: 15 March 2011.</ref> | |||
==Sequestrum== | |||
{{Main|Sequestrum}} | |||
==Osteoarthritis== | |||
{{Main|Osteoarthritis}} | |||
This keeps orthopaedic surgeons busy. | |||
==Aneurysmal bone cyst== | |||
{{Main|Aneurysmal bone cyst}} | |||
==Myositis ossificans== | |||
*[[AKA]] ''fibro-osseous pseudotumour of digits''.<ref name=Ref_WMSP607>{{Ref WMSP|607}}</ref> | |||
===General=== | |||
Epidemiology: | |||
*Young people. | |||
*History of trauma - typically. | |||
*Extremities - digits (fingers, toes). | |||
Notes: | |||
*Histologically "worrisome" (for malignancy) - due to high cellularity.<ref name=Ref_WMSP607>{{Ref WMSP|607}}</ref> | |||
===Microscopic=== | |||
Features:<ref name=Ref_WMSP607>{{Ref WMSP|607}}</ref> | |||
*High cellularity. | |||
*Low mitotic activity. | |||
*No atypical mitoses. | |||
*No hyperchromasia. | |||
Other features:<ref>IAV. 9 December 2010.</ref> | |||
*Low power diagnosis: | |||
**Lesion is well-circumscribed. | |||
**Normal muscle is adjacent to the lesion - '''key feature'''. | |||
DDx: | |||
*[[Heterotopic ossification]] - bone, not cellular, no inflammation. | |||
Images: | |||
*[http://path.upmc.edu/cases/case72/micro.html Myositis ossificans (upmc.edu)]. | |||
==Paget disease of the bone== | |||
{{Main|Paget's disease of the bone}} | |||
==Fibrous dysplasia== | |||
*[[AKA]] ''osteitis fibrosa''. | |||
{{Main|Fibrous dysplasia}} | |||
==Desmoplastic fibroma== | |||
*'''Not''' to be confused with ''[[desmoplastic fibroblastoma]]''. | |||
===General=== | |||
*Rare. | |||
===Microscopic=== | |||
Features:<ref>URL: [http://www.bonetumor.org/tumors-fibrous-tissue/desmoplastic-fibroma http://www.bonetumor.org/tumors-fibrous-tissue/desmoplastic-fibroma]. Accessed on: 14 April 2011.</ref> | |||
*Lamellar bone. | |||
*Fibrotic marrow space with: | |||
**Collagen. | |||
**Low cellularity. | |||
**Spindle cells without significant atypia. | |||
DDx: | |||
*[[Fibrous dysplasia]] - has woven bone. | |||
*Low grade [[fibrosarcoma]]. | |||
==Gaucher disease== | |||
{{Main|Gaucher disease}} | |||
===General=== | |||
*May present as a fracture. | |||
===Microscopic=== | |||
*Macrophages in the marrow space with a "crumpled tissue paper" appearance. | |||
==Langerhans cell histiocytosis of bone== | |||
*[[AKA]] ''eosinophilic granuloma of bone''. | |||
{{Main|Langerhans cell histiocytosis}} | |||
===General=== | |||
*Rare. | |||
*Children. | |||
===Microscopic=== | |||
Features: | |||
*Eosinophils. | |||
*Cerebriform and/or reniform macrophages. | |||
==Giant cell reparative granuloma== | |||
*[[AKA]] ''central [[giant cell]] granuloma'',<ref name=ijri>Shah UA, Shah AK, Kumar S. Giant cell reparative granuloma of the jaw: A case report. Indian J Radiol Imaging [serial online] 2006 [cited 2012 Feb 28];16:677-8. Available from: [http://www.ijri.org/text.asp?2006/16/4/677/32297 http://www.ijri.org/text.asp?2006/16/4/677/32297].</ref> abbreviated ''CGCG''. | |||
*[[AKA]] ''solid [[aneurysmal bone cyst]]''.<ref name=pmid22285042>{{Cite journal | last1 = Pan | first1 = Z. | last2 = Sanger | first2 = WG. | last3 = Bridge | first3 = JA. | last4 = Hunter | first4 = WJ. | last5 = Siegal | first5 = GP. | last6 = Wei | first6 = S. | title = A novel t(6;13)(q15;q34) translocation in a giant cell reparative granuloma (solid aneurysmal bone cyst). | journal = Hum Pathol | volume = | issue = | pages = | month = Jan | year = 2012 | doi = 10.1016/j.humpath.2011.10.003 | PMID = 22285042 }}</ref> | |||
===General=== | |||
*Lesion of the mandible and maxilla.<ref name=ijri/> | |||
===Radiology=== | |||
*Lytic lesion. | |||
===Microscopic=== | |||
Features:<ref name=ijri/> | |||
*Giant cells. | |||
*Fibroblasts. | |||
*Osteoid. | |||
*Hemosiderin-laden macrophages. | |||
DDx: | |||
*Peripheral giant cell granuloma - soft tissue counterpart of CGCG. | |||
*[[Giant cell tumour of bone]]. | |||
====Images==== | |||
<gallery> | |||
Image:Central_giant_cell_granuloma_-_intermed_mag.jpg | CGCG - intermed. mag. (WC/Nephron) | |||
Image:Central_giant_cell_granuloma_-_high_mag.jpg | CGCG - high mag. (WC/Nephron) | |||
</gallery> | |||
===Molecular=== | |||
Recurrent [[chromosomal translocation]]:<ref name=pmid22285042/> | |||
*t(16;17)(q22;p13). | |||
==Osteopetrosis== | |||
*[[AKA]] ''marble bone disease''.<ref name=pmid19232111>{{Cite journal | last1 = Stark | first1 = Z. | last2 = Savarirayan | first2 = R. | title = Osteopetrosis. | journal = Orphanet J Rare Dis | volume = 4 | issue = | pages = 5 | month = | year = 2009 | doi = 10.1186/1750-1172-4-5 | PMID = 19232111 | PMC = 2654865 }}</ref> | |||
===General=== | |||
*Rare. | |||
*Genetic - may be autosomal dominant, autosomal recessive or X-linked.<ref name=pmid19232111/> | |||
*Pancytopenias - due to oblieration of the marrow space. | |||
*[[bone fractures|Fractures]]. | |||
*Radiologic diagnosis. | |||
===Gross=== | |||
*Marbled appearance. | |||
*Thickening with obliteration of the marrow space. | |||
*Patchy (brown) surface due to vascularization/[[extramedullary hematopoiesis]].<ref name=Ref_AoGP469>{{Ref AoGP|469}}</ref> | |||
Image: | |||
*[http://www.uaz.edu.mx/histo/pathology/ed/ch_26/c26_s25.htm Osteopetrosis (uaz.edu.mx)]. | |||
===Microscopic=== | |||
Features:<ref name=pmid11264157/> | |||
*Abundant irregular (pink) bony trabeculae with layers of (blue-gray) [[cartilage]]. | |||
Image: | |||
*[http://bloodjournal.hematologylibrary.org/content/97/7/1947/F2.expansion.html Osteopetrosis (bloodjournal.hematologylibrary.org)].<ref name=pmid11264157>{{Cite journal | last1 = McMahon | first1 = C. | last2 = Will | first2 = A. | last3 = Hu | first3 = P. | last4 = Shah | first4 = GN. | last5 = Sly | first5 = WS. | last6 = Smith | first6 = OP. | title = Bone marrow transplantation corrects osteopetrosis in the carbonic anhydrase II deficiency syndrome. | journal = Blood | volume = 97 | issue = 7 | pages = 1947-50 | month = Apr | year = 2001 | doi = | PMID = 11264157 |URL = http://bloodjournal.hematologylibrary.org/content/97/7/1947.full }}</ref> | |||
==Osteoporosis== | |||
===General=== | |||
*Very common. | |||
*Associated with [[bone fractures|fractures]], esp. wrist, [[traumatic hip fracture|hip]] & vertebra.<ref name=pmid22537071>{{Cite journal | last1 = Lix | first1 = LM. | last2 = Azimaee | first2 = M. | last3 = Acan Osman | first3 = B. | last4 = Caetano | first4 = P. | last5 = Morin | first5 = S. | last6 = Metge | first6 = C. | last7 = Goltzman | first7 = D. | last8 = Kreiger | first8 = N. | last9 = Prior | first9 = J. | title = Osteoporosis-related fracture case definitions for population-based administrative data. | journal = BMC Public Health | volume = 12 | issue = 1 | pages = 301 | month = Apr | year = 2012 | doi = 10.1186/1471-2458-12-301 | PMID = 22537071 }}</ref> | |||
*Radiologic diagnosis - bone mineral density. | |||
Etiology:<ref name=Ref_PCPBoD8_617>{{Ref PCPBoD8|617}}</ref> | |||
*Primary (senile). | |||
*Secondary: | |||
**Endocrine: | |||
***Hyperparathyroidism. | |||
**Gastrointestinal: | |||
***Malabsorption, e.g. [[celiac disease]], [[cystic fibrosis]], [[Crohn's disease]]. | |||
***Starvation. | |||
**Psychiatric: | |||
***Anorexia nervosa. | |||
***Bulimia nervosa. | |||
**Neoplasia: | |||
***[[Multiple myeloma]]. | |||
**Drugs: | |||
***Systemic steroids.<ref name=pmid16243531>{{Cite journal | last1 = Dalle Carbonare | first1 = L. | last2 = Bertoldo | first2 = F. | last3 = Valenti | first3 = MT. | last4 = Zenari | first4 = S. | last5 = Zanatta | first5 = M. | last6 = Sella | first6 = S. | last7 = Giannini | first7 = S. | last8 = Cascio | first8 = VL. | title = Histomorphometric analysis of glucocorticoid-induced osteoporosis. | journal = Micron | volume = 36 | issue = 7-8 | pages = 645-52 | month = | year = 2005 | doi = 10.1016/j.micron.2005.07.009 | PMID = 16243531 }}</ref> | |||
===Gross=== | |||
*Decreased numbers of, abnormally thin, bony spicules. | |||
Images: | |||
*[http://www.sciencephoto.com/media/260363/enlarge Osteoporosis (sciencephoto.com)]. | |||
*[http://library.med.utah.edu/WebPath/TUTORIAL/OSTEO/OST005.html Osteoporosis (utah.edu)]. | |||
===Microscopic=== | |||
Features (femoral neck):<ref name=pmid18708176>{{Cite journal | last1 = Blain | first1 = H. | last2 = Chavassieux | first2 = P. | last3 = Portero-Muzy | first3 = N. | last4 = Bonnel | first4 = F. | last5 = Canovas | first5 = F. | last6 = Chammas | first6 = M. | last7 = Maury | first7 = P. | last8 = Delmas | first8 = PD. | title = Cortical and trabecular bone distribution in the femoral neck in osteoporosis and osteoarthritis. | journal = Bone | volume = 43 | issue = 5 | pages = 862-8 | month = Nov | year = 2008 | doi = 10.1016/j.bone.2008.07.236 | PMID = 18708176 }}</ref> | |||
*Thinner cortex. | |||
*Decreased trabecular thickness | |||
*Decreased number of trabeculae. | |||
Note: | |||
*One study looking at iliac bone biopsies suggests trabeculae are no different in osteoporosis.<ref name=pmid3414359>{{Cite journal | last1 = Chappard | first1 = D. | last2 = Alexandre | first2 = C. | last3 = Riffat | first3 = G. | title = Spatial distribution of trabeculae in iliac bone from 145 osteoporotic females. | journal = Acta Anat (Basel) | volume = 132 | issue = 2 | pages = 137-42 | month = | year = 1988 | doi = | PMID = 3414359 }}</ref> | |||
=See also= | |||
*[[Cartilage]]. | |||
*[[Chondro-osseous tumours]]. | |||
*[[Femoral head]]. | |||
*[[Spine]]. | |||
*[[Hematopathology]]. | *[[Hematopathology]]. | ||
*[[Soft tissue lesions]]. | *[[Soft tissue lesions]]. | ||
*[[Small round cell tumours]]. | *[[Small round cell tumours]]. | ||
=References= | |||
{{reflist|2}} | {{reflist|2}} | ||
[[Category: | =External links= | ||
*[http://www.medicalhistology.us/twiki/bin/view/Main/CartilageAndBoneAtlas08 Bone and cartilage histology (medicalhistology.us)]. | |||
[[Category:Bone]] | |||
Latest revision as of 21:39, 23 June 2018
Bone is a scaffold it bears weight and occasionally gets infected.
Tumours often spread to bone and occasionally arise in bone. Bone tumours are dealt with in the bone tumours article.
Normal bone
Bone anatomy
- Epiphysis = rounded end of the bone.
- Metaphysis = between epiphysis and diaphysis; contains epiphyseal plate - site of growth in childhood.
- Diaphysis = shaft, mid-portion, contains bone marrow.
Image
Bone histology
Two types (based on arrangement of collagen):
- Woven bone.
- Lamellar bone.
Woven bone
- Always abnormal in adults.
- Collagen arranged haphazardly - mechanically weak.
Images:
Lamellar bone
- Collagen organized in layers (lamellae).
Woven versus lamellar
- Easiest way to differentiate: polarize; lamellar bone has well-defined layers.
Bone cells
- Osteocytes.
- Sit in lacunae.
- Empty lacunae = necrotic bone.
- Sit in lacunae.
- Osteoblasts.
- Make bone.
- Osteoclasts.
- Destroy bone.
- Multinucleated.
Memory device: 'b' before 'c'.
Bone marrow
General
- One of two primary lymphoid organs - the other one is the thymus.[2]
Bone marrow biopsy adequacy:[3]
- 10 intertrabecular spaces or 10 mm.
Microscopic
One should see three cell lines:[4]
- Erythroid (red cells).
- Myeloid (white blood cells).
- Megakaryocytic (platelets).
Adipose tissue:
- Fat content (%) ~= age in years.[5]
- e.g. 60 year old will have 60% fatty replacement.
Identifying the cell lines:[6]
- Megakaryocytes:
- Big cells ~ 3x the size of a RBC.
- Normoblasts (RBC precursors):
- Hyperchromatic, i.e. blue, nucleus.
- Myeloid line:
- Granules.
- Reniform nucleus, i.e. kidney bean shaped nucleus.
Note:
- Lymphocytes are considered separately and typically spared in bone marrow failure.[7]
Organization
- Mature hematopoeitic cells at the centre (distant from bone).
- Immature hematopoeitic cells adjacent to the bone.
Note:
- Immediately adjacent to the bone (paratrabecular)... is where follicular lymphoma is classically found.[8]
Images
Sign out
Essentially normal
Bone Marrow, Posterior Superior Iliac Spine, Biopsy: - Bone marrow with trilineage hematopoiesis. - Cellularity within normal limits for age. - Case will be sent to hematology for consultation and correlation with other testing.
Inadequate
Right Posterior Superior Iliac Spine, Bone Marrow Biopsy: - Predominantly benign dense fibrous tissue with a small amount of laminar bone, and minute fragment of marrow (<2 mm). - Case will be sent to hematopathology for further assessment.
Benign variants
Hyperostosis frontalis interna
- Extra-thick frontal bone.[9]
- No clinical significance -- just has to be recognized as a "nothing".
Infections
Acute osteomyelitis
General
Pathophysiology/entry:
- Hematogenous - often in children.
- Direct entry (skin defect) - adults with diabetes.
Microscopic
Features:
- PMNs.
- Micro-organisms - esp. cocci.
Image:
Stains
Chronic osteomyelitis
General
Most common organism:
- Staphylococcus aureus.[10]
Risk factors:[10]
- Diabetes mellitus.
- Peripheral vascular disease.
Microscopic
Features:
- Plasma cells - key feature.
- May be sterile, i.e. no organisms.
- +/-Fibrosis.
- +/-Necrotic bone - bone with empty lacunae.
- +/-Amyloid.
- ~10% of patients in one series.[11]
Image:
Sign out
LOWER LEG, RIGHT, BELOW KNEE AMPUTATION: - ACUTE AND CHRONIC OSTEOMYELITIS. - MODERATE ATHEROSCLEROSIS. - SKIN ULCERATION. - SOFT TISSUE SURGICAL MARGIN WITH FAT NECROSIS AND MUSCULAR ATROPHY. - NEGATIVE FOR MALIGNANCY.
TRAPEZIUM, RIGHT HAND, REMOVAL: - DEGENERATIVE JOINT DISEASE. - MARROW SPACE WITH FIBROSIS AND SCATTERED LYMPHOCYTES AND PLASMA CELLS, COMPATIBLE WITH MILD CHRONIC OSTEOMYELITIS. - NO MICROORGANISMS APPARENT WITH ROUTINE STAINS. - NEGATIVE FOR MALIGNANCY.
Bone tumours
This is a big topic. It is dealt with in a separate article.
The bone tumour article covers tumour mimics, e.g. brown cell tumour.
Fractures
This is dealt with in the forensic pathology article.
Others
The following is a collection of stuff that doesn't really fit in another category or is just weird.
A general DDx for cystic bone lesions is found on radipedia.com.[12]
Sequestrum
Osteoarthritis
This keeps orthopaedic surgeons busy.
Aneurysmal bone cyst
Myositis ossificans
General
Epidemiology:
- Young people.
- History of trauma - typically.
- Extremities - digits (fingers, toes).
Notes:
- Histologically "worrisome" (for malignancy) - due to high cellularity.[13]
Microscopic
Features:[13]
- High cellularity.
- Low mitotic activity.
- No atypical mitoses.
- No hyperchromasia.
Other features:[14]
- Low power diagnosis:
- Lesion is well-circumscribed.
- Normal muscle is adjacent to the lesion - key feature.
DDx:
- Heterotopic ossification - bone, not cellular, no inflammation.
Images:
Paget disease of the bone
Fibrous dysplasia
- AKA osteitis fibrosa.
Desmoplastic fibroma
- Not to be confused with desmoplastic fibroblastoma.
General
- Rare.
Microscopic
Features:[15]
- Lamellar bone.
- Fibrotic marrow space with:
- Collagen.
- Low cellularity.
- Spindle cells without significant atypia.
DDx:
- Fibrous dysplasia - has woven bone.
- Low grade fibrosarcoma.
Gaucher disease
General
- May present as a fracture.
Microscopic
- Macrophages in the marrow space with a "crumpled tissue paper" appearance.
Langerhans cell histiocytosis of bone
- AKA eosinophilic granuloma of bone.
General
- Rare.
- Children.
Microscopic
Features:
- Eosinophils.
- Cerebriform and/or reniform macrophages.
Giant cell reparative granuloma
- AKA central giant cell granuloma,[16] abbreviated CGCG.
- AKA solid aneurysmal bone cyst.[17]
General
- Lesion of the mandible and maxilla.[16]
Radiology
- Lytic lesion.
Microscopic
Features:[16]
- Giant cells.
- Fibroblasts.
- Osteoid.
- Hemosiderin-laden macrophages.
DDx:
- Peripheral giant cell granuloma - soft tissue counterpart of CGCG.
- Giant cell tumour of bone.
Images
Molecular
Recurrent chromosomal translocation:[17]
- t(16;17)(q22;p13).
Osteopetrosis
General
- Rare.
- Genetic - may be autosomal dominant, autosomal recessive or X-linked.[18]
- Pancytopenias - due to oblieration of the marrow space.
- Fractures.
- Radiologic diagnosis.
Gross
- Marbled appearance.
- Thickening with obliteration of the marrow space.
- Patchy (brown) surface due to vascularization/extramedullary hematopoiesis.[19]
Image:
Microscopic
Features:[20]
- Abundant irregular (pink) bony trabeculae with layers of (blue-gray) cartilage.
Image:
Osteoporosis
General
- Very common.
- Associated with fractures, esp. wrist, hip & vertebra.[21]
- Radiologic diagnosis - bone mineral density.
Etiology:[22]
- Primary (senile).
- Secondary:
- Endocrine:
- Hyperparathyroidism.
- Gastrointestinal:
- Malabsorption, e.g. celiac disease, cystic fibrosis, Crohn's disease.
- Starvation.
- Psychiatric:
- Anorexia nervosa.
- Bulimia nervosa.
- Neoplasia:
- Drugs:
- Systemic steroids.[23]
- Endocrine:
Gross
- Decreased numbers of, abnormally thin, bony spicules.
Images:
Microscopic
Features (femoral neck):[24]
- Thinner cortex.
- Decreased trabecular thickness
- Decreased number of trabeculae.
Note:
- One study looking at iliac bone biopsies suggests trabeculae are no different in osteoporosis.[25]
See also
- Cartilage.
- Chondro-osseous tumours.
- Femoral head.
- Spine.
- Hematopathology.
- Soft tissue lesions.
- Small round cell tumours.
References
- ↑ Lin DD, Gailloud P, McCarthy EF, Comi AM (February 2006). "Oromaxillofacial osseous abnormality in Sturge-Weber syndrome: case report and review of the literature". AJNR Am J Neuroradiol 27 (2): 274–7. PMID 16484391.
- ↑ URL: http://www.life.umd.edu/classroom/bsci423/song/Lab1.html. Accessed on: 28 March 2012.
- ↑ Rudzki, Z.; Partyła, T.; Okoń, K.; Stachura, J. (2005). "Adequacy of trephine bone marrow biopsies: the doctor and the patient make a difference.". Pol J Pathol 56 (4): 187-95. PMID 16477878.
- ↑ URL: http://emedicine.medscape.com/article/199003-overview. Accessed on: 28 March 2012.
- ↑ IAV. 26 Feb 2009.
- ↑ http://upload.wikimedia.org/wikipedia/commons/6/69/Hematopoiesis_%28human%29_diagram.png
- ↑ http://emedicine.medscape.com/article/199003-overview
- ↑ Iancu, D.; Hao, S.; Lin, P.; Anderson, SK.; Jorgensen, JL.; McLaughlin, P.; Medeiros, LJ. (Feb 2007). "Follicular lymphoma in staging bone marrow specimens: correlation of histologic findings with the results of flow cytometry immunophenotypic analysis.". Arch Pathol Lab Med 131 (2): 282-7. doi:10.1043/1543-2165(2007)131[282:FLISBM]2.0.CO;2. PMID 17284114.
- ↑ URL: http://radiopaedia.org/articles/hyperostosis_frontalis_interna. Accessed on: 29 September 2010.
- ↑ 10.0 10.1 Hatzenbuehler, J.; Pulling, TJ. (Nov 2011). "Diagnosis and management of osteomyelitis.". Am Fam Physician 84 (9): 1027-33. PMID 22046943.
- ↑ Alabi, ZO.; Ojo, OS.; Odesanmi, WO. (1991). "Secondary amyloidosis in chronic osteomyelitis.". Int Orthop 15 (1): 21-2. PMID 2071276.
- ↑ URL: http://radipedia.com/WikiMedia/index.php?title=Benign_cystic_bone_lesions. Accessed on: 15 March 2011.
- ↑ 13.0 13.1 13.2 Humphrey, Peter A; Dehner, Louis P; Pfeifer, John D (2008). The Washington Manual of Surgical Pathology (1st ed.). Lippincott Williams & Wilkins. pp. 607. ISBN 978-0781765275.
- ↑ IAV. 9 December 2010.
- ↑ URL: http://www.bonetumor.org/tumors-fibrous-tissue/desmoplastic-fibroma. Accessed on: 14 April 2011.
- ↑ 16.0 16.1 16.2 Shah UA, Shah AK, Kumar S. Giant cell reparative granuloma of the jaw: A case report. Indian J Radiol Imaging [serial online] 2006 [cited 2012 Feb 28];16:677-8. Available from: http://www.ijri.org/text.asp?2006/16/4/677/32297.
- ↑ 17.0 17.1 Pan, Z.; Sanger, WG.; Bridge, JA.; Hunter, WJ.; Siegal, GP.; Wei, S. (Jan 2012). "A novel t(6;13)(q15;q34) translocation in a giant cell reparative granuloma (solid aneurysmal bone cyst).". Hum Pathol. doi:10.1016/j.humpath.2011.10.003. PMID 22285042.
- ↑ 18.0 18.1 Stark, Z.; Savarirayan, R. (2009). "Osteopetrosis.". Orphanet J Rare Dis 4: 5. doi:10.1186/1750-1172-4-5. PMC 2654865. PMID 19232111. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2654865/.
- ↑ Rose, Alan G. (2008). Atlas of Gross Pathology with Histologic Correlation (1st ed.). Cambridge University Press. pp. 469. ISBN 978-0521868792.
- ↑ 20.0 20.1 McMahon, C.; Will, A.; Hu, P.; Shah, GN.; Sly, WS.; Smith, OP. (Apr 2001). "Bone marrow transplantation corrects osteopetrosis in the carbonic anhydrase II deficiency syndrome.". Blood 97 (7): 1947-50. PMID 11264157.
- ↑ Lix, LM.; Azimaee, M.; Acan Osman, B.; Caetano, P.; Morin, S.; Metge, C.; Goltzman, D.; Kreiger, N. et al. (Apr 2012). "Osteoporosis-related fracture case definitions for population-based administrative data.". BMC Public Health 12 (1): 301. doi:10.1186/1471-2458-12-301. PMID 22537071.
- ↑ Mitchell, Richard; Kumar, Vinay; Fausto, Nelson; Abbas, Abul K.; Aster, Jon (2011). Pocket Companion to Robbins & Cotran Pathologic Basis of Disease (8th ed.). Elsevier Saunders. pp. 617. ISBN 978-1416054542.
- ↑ Dalle Carbonare, L.; Bertoldo, F.; Valenti, MT.; Zenari, S.; Zanatta, M.; Sella, S.; Giannini, S.; Cascio, VL. (2005). "Histomorphometric analysis of glucocorticoid-induced osteoporosis.". Micron 36 (7-8): 645-52. doi:10.1016/j.micron.2005.07.009. PMID 16243531.
- ↑ Blain, H.; Chavassieux, P.; Portero-Muzy, N.; Bonnel, F.; Canovas, F.; Chammas, M.; Maury, P.; Delmas, PD. (Nov 2008). "Cortical and trabecular bone distribution in the femoral neck in osteoporosis and osteoarthritis.". Bone 43 (5): 862-8. doi:10.1016/j.bone.2008.07.236. PMID 18708176.
- ↑ Chappard, D.; Alexandre, C.; Riffat, G. (1988). "Spatial distribution of trabeculae in iliac bone from 145 osteoporotic females.". Acta Anat (Basel) 132 (2): 137-42. PMID 3414359.