Difference between revisions of "Eosinophilic esophagitis"
Jump to navigation
Jump to search
m (→See also) |
(fix sp) |
||
| (16 intermediate revisions by the same user not shown) | |||
| Line 1: | Line 1: | ||
{{ Infobox diagnosis | |||
| Name = {{PAGENAME}} | |||
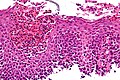
| Image = Eosinophilic_esophagitis_-_2_-_very_high_mag.jpg | |||
| Width = | |||
| Caption = Eosinophilic esophagitis. [[H&E stain]]. | |||
| Micro = mucosa with abundant eosinophils (60 per mm*mm), [[basal cell hyperplasia]] (three cells thick ''or'' >15% of epithelial thickness), papillae elongated (reach into the top 1/3 of the epithelial layer) | |||
| Subtypes = | |||
| LMDDx = [[GERD]] | |||
| Stains = | |||
| IHC = | |||
| EM = | |||
| Molecular = | |||
| IF = | |||
| Gross = | |||
| Grossing = | |||
| Site = [[esophagus]] | |||
| Assdx = atopy, [[celiac disease]] | |||
| Syndromes = | |||
| Clinicalhx = may be unresponsive to proton pump inhibitors (PPIs) | |||
| Signs = | |||
| Symptoms = similar to [[GERD]] | |||
| Prevalence = uncommon | |||
| Bloodwork = | |||
| Rads = | |||
| Endoscopy = trachealization of esophagus ([[AKA]] feline esophagus) | |||
| Prognosis = | |||
| Other = | |||
| ClinDDx = [[GERD]] | |||
}} | |||
'''Eosinophilic esophagitis''', abbreviated '''EE''', is relatively uncommon pathology of the [[esophagus]] with some similarities to [[gastroesophageal reflux disease]] (GERD). | '''Eosinophilic esophagitis''', abbreviated '''EE''', is relatively uncommon pathology of the [[esophagus]] with some similarities to [[gastroesophageal reflux disease]] (GERD). | ||
| Line 12: | Line 41: | ||
*Avoid exacerbating antigens. | *Avoid exacerbating antigens. | ||
*Topical corticosteroids, e.g. fluticasone. | *Topical corticosteroids, e.g. fluticasone. | ||
* | |||
Note on treatment: | |||
*The classic teaching was that EE does not respond to proton pump inhibitors; thinking on this has evolved.<ref name=pmid30009819/> | |||
Biopsies: | Biopsies: | ||
| Line 26: | Line 57: | ||
==Gross/endoscopic== | ==Gross/endoscopic== | ||
*'''Trachealization'''; | *'''Trachealization'''; esophagus looks like trachea.<ref name=pmid19636182>{{Cite journal | last1 = Al-Hussaini | first1 = AA. | last2 = Semaan | first2 = T. | last3 = El Hag | first3 = IA. | title = Esophageal trachealization: a feature of eosinophilic esophagitis. | journal = Saudi J Gastroenterol | volume = 15 | issue = 3 | pages = 193-5 | month = | year = | doi = 10.4103/1319-3767.54747 | PMID = 19636182 }} | ||
</ref> | </ref> | ||
**[[AKA]] ''feline esophagus''.<ref>URL: [http://www.ajronline.org/cgi/reprint/164/4/900.pdf http://www.ajronline.org/cgi/reprint/164/4/900.pdf]. Accessed on: 4 October 2010.</ref> | **[[AKA]] ''feline esophagus''.<ref>URL: [http://www.ajronline.org/cgi/reprint/164/4/900.pdf http://www.ajronline.org/cgi/reprint/164/4/900.pdf]. Accessed on: 4 October 2010.</ref> | ||
| Line 42: | Line 73: | ||
==Microscopic== | ==Microscopic== | ||
Features:<ref name=Ref_GLP19>{{Ref GLP|19}}</ref> | Features:<ref name=Ref_GLP19>{{Ref GLP|19}}</ref> | ||
*Mucosa with | *Mucosa with abundant eosinophils - the consensus on eosinophils per area is 60/mm*mm.<ref name=pmid30009819>{{cite journal |authors=Dellon ES, Liacouras CA, Molina-Infante J, Furuta GT, Spergel JM, Zevit N, Spechler SJ, Attwood SE, Straumann A, Aceves SS, Alexander JA, Atkins D, Arva NC, Blanchard C, Bonis PA, Book WM, Capocelli KE, Chehade M, Cheng E, Collins MH, Davis CM, Dias JA, Di Lorenzo C, Dohil R, Dupont C, Falk GW, Ferreira CT, Fox A, Gonsalves NP, Gupta SK, Katzka DA, Kinoshita Y, Menard-Katcher C, Kodroff E, Metz DC, Miehlke S, Muir AB, Mukkada VA, Murch S, Nurko S, Ohtsuka Y, Orel R, Papadopoulou A, Peterson KA, Philpott H, Putnam PE, Richter JE, Rosen R, Rothenberg ME, Schoepfer A, Scott MM, Shah N, Sheikh J, Souza RF, Strobel MJ, Talley NJ, Vaezi MF, Vandenplas Y, Vieira MC, Walker MM, Wechsler JB, Wershil BK, Wen T, Yang GY, Hirano I, Bredenoord AJ |title=Updated International Consensus Diagnostic Criteria for Eosinophilic Esophagitis: Proceedings of the AGREE Conference |journal=Gastroenterology |volume=155 |issue=4 |pages=1022–1033.e10 |date=October 2018 |pmid=30009819 |pmc=6174113 |doi=10.1053/j.gastro.2018.07.009 |url=}}</ref> | ||
*[[Basal cell hyperplasia]]. | *[[Basal cell hyperplasia]]. | ||
**Three cells thick ''or'' >15% of epithelial thickness. | **Three cells thick ''or'' >15% of epithelial thickness. | ||
| Line 48: | Line 79: | ||
**Papillae that reach into the top 1/3 of the epithelial layer - definition for GERD.<ref name=Ref_PBoD804>{{Ref PBoD|804}}</ref> | **Papillae that reach into the top 1/3 of the epithelial layer - definition for GERD.<ref name=Ref_PBoD804>{{Ref PBoD|804}}</ref> | ||
Note: | |||
* | *Many microscopes have an eye piece diameter of 22 mm. Thus, the field area (for a "HPF") with the 40x objective is ~0.2376 mm*mm. This works out to approximately 15 eosinophils/HPF. | ||
* | |||
DDx:<ref name=Ref_Odze244>{{Ref Odze|244}}</ref> | DDx:<ref name=Ref_Odze244>{{Ref Odze|244}}</ref> | ||
| Line 65: | Line 90: | ||
===Images=== | ===Images=== | ||
<gallery> | <gallery> | ||
Image: | Image:Eosinophilic esophagitis - intermed mag.jpg | Intermed. mag. (WC) | ||
Image: | Image:Eosinophilic esophagitis - high mag.jpg | High mag. (WC) | ||
Image:Eosinophilic esophagitis - very high mag.jpg | Very high mag. (WC) | |||
Image:Eosinophilic esophagitis - 2 - high mag.jpg | High mag. (WC) | |||
Image:Eosinophilic esophagitis - 2 - very high mag.jpg | Very high mag. (WC) | |||
</gallery> | </gallery> | ||
====www==== | |||
*[http://www.ncbi.nlm.nih.gov/pmc/articles/PMC2841420/figure/F0003/ Eosinophilic esophagitis (nih.gov)]. | *[http://www.ncbi.nlm.nih.gov/pmc/articles/PMC2841420/figure/F0003/ Eosinophilic esophagitis (nih.gov)]. | ||
*[http://www.archivesofpathology.org/action/showFullPopup?id=i1543-2165-134-6-815-f03&doi=10.1043%2F1543-2165-134.6.815 EE versus GERD (archivesofpathology.org)].<ref name=pmid20524860/> | *[http://www.archivesofpathology.org/action/showFullPopup?id=i1543-2165-134-6-815-f03&doi=10.1043%2F1543-2165-134.6.815 EE versus GERD (archivesofpathology.org)].<ref name=pmid20524860/> | ||
*[http://www.medunigraz.at/23798 Eosinophilic esophagitis - nice pictures (medunigraz.at)]. | |||
==Sign out== | ==Sign out== | ||
<pre> | |||
A. Distal Esophagus, Biopsy: | |||
- Squamous mucosa with basal cell hyperplasia, abundant intraepithelial | |||
eosinophils, edema, and papillary elongation, see comment. | |||
- NEGATIVE for columnar type epithelium. | |||
- NEGATIVE for dysplasia. | |||
B. Mid Esophagus, Biopsy: | |||
- Squamous mucosa with basal cell hyperplasia, abundant intraepithelial | |||
eosinophils, edema, and papillary elongation, see comment. | |||
- NEGATIVE for dysplasia. | |||
COMMENT: | |||
There are approximately 35 eosinophils per 0.2376 mm*mm (1 HPF) in | |||
both Part A and Part B. | |||
The above findings are suggestive of eosinophilic esophagitis in the proper | |||
clinical context. | |||
</pre> | |||
===Block letters=== | |||
<pre> | <pre> | ||
ESOPHAGUS, DISTAL, BIOPSY: | ESOPHAGUS, DISTAL, BIOPSY: | ||
| Line 82: | Line 134: | ||
COMMENT: | COMMENT: | ||
There are approximately 65 eosinophils per 0.2376 mm*mm (1 HPF). | There are approximately 65 eosinophils per 0.2376 mm*mm (1 HPF). | ||
The above findings are suggestive of eosinophilic esophagitis in the proper | The above findings are suggestive of eosinophilic esophagitis in the proper | ||
| Line 108: | Line 153: | ||
compatible with gastroesophageal reflux; however, eosinophilic esophagitis is also a | compatible with gastroesophageal reflux; however, eosinophilic esophagitis is also a | ||
consideration. Clinical correlation is required. | consideration. Clinical correlation is required. | ||
</pre> | </pre> | ||
| Line 136: | Line 174: | ||
*[[Esophagus]]. | *[[Esophagus]]. | ||
*[[Eosinophilic colitis]]. | *[[Eosinophilic colitis]]. | ||
*[[Eosinophilic gastritis]]. | |||
==References== | ==References== | ||
Latest revision as of 22:59, 27 January 2022
| Eosinophilic esophagitis | |
|---|---|
| Diagnosis in short | |
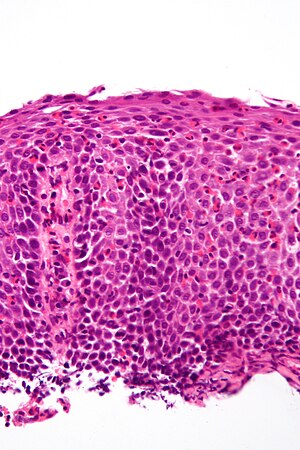 Eosinophilic esophagitis. H&E stain. | |
|
| |
| LM | mucosa with abundant eosinophils (60 per mm*mm), basal cell hyperplasia (three cells thick or >15% of epithelial thickness), papillae elongated (reach into the top 1/3 of the epithelial layer) |
| LM DDx | GERD |
| Site | esophagus |
|
| |
| Associated Dx | atopy, celiac disease |
| Clinical history | may be unresponsive to proton pump inhibitors (PPIs) |
| Symptoms | similar to GERD |
| Prevalence | uncommon |
| Endoscopy | trachealization of esophagus (AKA feline esophagus) |
| Clin. DDx | GERD |
Eosinophilic esophagitis, abbreviated EE, is relatively uncommon pathology of the esophagus with some similarities to gastroesophageal reflux disease (GERD).
General
- The current thinking is that it is a clinico-pathologic diagnosis.[1]
Clinical:
- Dysphagia[2] - classic presentation.
- Dyspepsia.
- Often mimics gastroesophageal reflux disease (GERD).[3]
Treatment:
- Avoid exacerbating antigens.
- Topical corticosteroids, e.g. fluticasone.
Note on treatment:
- The classic teaching was that EE does not respond to proton pump inhibitors; thinking on this has evolved.[4]
Biopsies:
- Should be taken from: upper, mid, lower and submitted in separate containers (eosinophilia present through-out-- to differentiate from GERD).
Associations:
- Atopy.[5]
- Celiac disease.[6]
- Oral antigens, i.e. particular foods.[3]
- Familial association.[3]
- Young ~ 35 years old.[7]
- Male > female (3:1).[7]
Gross/endoscopic
DDx (endoscopic):
Image
Microscopic
Features:[5]
- Mucosa with abundant eosinophils - the consensus on eosinophils per area is 60/mm*mm.[4]
- Basal cell hyperplasia.
- Three cells thick or >15% of epithelial thickness.
- Papillae elongated.
- Papillae that reach into the top 1/3 of the epithelial layer - definition for GERD.[10]
Note:
- Many microscopes have an eye piece diameter of 22 mm. Thus, the field area (for a "HPF") with the 40x objective is ~0.2376 mm*mm. This works out to approximately 15 eosinophils/HPF.
DDx:[11]
- Gastroesophageal reflux disease - no mid and proximal involvement.
- Infectious esophagitis.
- Eosinophilic gastroenteritis.
- Hypereosinophilic syndrome.
Images
www
- Eosinophilic esophagitis (nih.gov).
- EE versus GERD (archivesofpathology.org).[1]
- Eosinophilic esophagitis - nice pictures (medunigraz.at).
Sign out
A. Distal Esophagus, Biopsy:
- Squamous mucosa with basal cell hyperplasia, abundant intraepithelial
eosinophils, edema, and papillary elongation, see comment.
- NEGATIVE for columnar type epithelium.
- NEGATIVE for dysplasia.
B. Mid Esophagus, Biopsy:
- Squamous mucosa with basal cell hyperplasia, abundant intraepithelial
eosinophils, edema, and papillary elongation, see comment.
- NEGATIVE for dysplasia.
COMMENT:
There are approximately 35 eosinophils per 0.2376 mm*mm (1 HPF) in
both Part A and Part B.
The above findings are suggestive of eosinophilic esophagitis in the proper
clinical context.
Block letters
ESOPHAGUS, DISTAL, BIOPSY: - SQUAMOUS MUCOSA WITH BASAL CELL HYPERPLASIA, ABUNDANT INTRAEPITHELIAL EOSINOPHILS, EDEMA, AND PAPILLARY ELONGATION, SEE COMMENT. - STAINS (PAS-D, GMS) NEGATIVE FOR MICROORGANISMS. - NEGATIVE FOR INTESTINAL METAPLASIA. - NEGATIVE FOR DYSPLASIA. COMMENT: There are approximately 65 eosinophils per 0.2376 mm*mm (1 HPF). The above findings are suggestive of eosinophilic esophagitis in the proper clinical context.
Patchy eosinophils
ESOPHAGUS (DISTAL), BIOPSY: - SQUAMOUS MUCOSA WITH BASAL CELL HYPERPLASIA, INTRAEPITHELIAL EDEMA AND ONLY FOCALLY ABUNDANT INTRAEPITHELIAL EOSINOPHILS, SEE COMMENT. - COLUMNAR EPITHELIUM WITH MODERATE CHRONIC INFLAMMATION, AND PANCREATIC ACINAR METAPLASIA. - NEGATIVE FOR INTESTINAL METAPLASIA. - NEGATIVE FOR DYSPLASIA AND NEGATIVE FOR MALIGNANCY. COMMENT: One high power field (field diameter 0.55 mm) has 25 eosinophils. The findings are compatible with gastroesophageal reflux; however, eosinophilic esophagitis is also a consideration. Clinical correlation is required.
Histology suggestive
ESOPHAGUS, BIOPSY: - SQUAMOUS MUCOSA WITH MARKED BASAL CELL HYPERPLASIA, FOCALLY ABUNDANT INTRAEPITHELIAL EOSINOPHILS, EDEMA, AND PAPILLARY ELONGATION, SEE COMMENT. - NEGATIVE FOR INTESTINAL METAPLASIA. - NEGATIVE FOR DYSPLASIA. COMMENT: Focally, there are approximately 35 eosinophils per 0.2376 mm*mm (1 HPF). The above findings raise the possibility of eosinophilic esophagitis; clinical correlation is suggested. A re-biopsy including a portion of the proximal esophagus could be considered.
See also
References
- ↑ 1.0 1.1 Genevay, M.; Rubbia-Brandt, L.; Rougemont, AL. (Jun 2010). "Do eosinophil numbers differentiate eosinophilic esophagitis from gastroesophageal reflux disease?". Arch Pathol Lab Med 134 (6): 815-25. doi:10.1043/1543-2165-134.6.815. PMID 20524860. http://www.archivesofpathology.org/doi/full/10.1043/1543-2165-134.6.815.
- ↑ URL: http://www.medicinenet.com/eosinophilic_esophagitis/page2.htm#tocc. Accessed on: 1 December 2009.
- ↑ 3.0 3.1 3.2 Rothenberg, ME. (Oct 2009). "Biology and treatment of eosinophilic esophagitis.". Gastroenterology 137 (4): 1238-49. doi:10.1053/j.gastro.2009.07.007. PMID 19596009.
- ↑ 4.0 4.1 Dellon ES, Liacouras CA, Molina-Infante J, Furuta GT, Spergel JM, Zevit N, Spechler SJ, Attwood SE, Straumann A, Aceves SS, Alexander JA, Atkins D, Arva NC, Blanchard C, Bonis PA, Book WM, Capocelli KE, Chehade M, Cheng E, Collins MH, Davis CM, Dias JA, Di Lorenzo C, Dohil R, Dupont C, Falk GW, Ferreira CT, Fox A, Gonsalves NP, Gupta SK, Katzka DA, Kinoshita Y, Menard-Katcher C, Kodroff E, Metz DC, Miehlke S, Muir AB, Mukkada VA, Murch S, Nurko S, Ohtsuka Y, Orel R, Papadopoulou A, Peterson KA, Philpott H, Putnam PE, Richter JE, Rosen R, Rothenberg ME, Schoepfer A, Scott MM, Shah N, Sheikh J, Souza RF, Strobel MJ, Talley NJ, Vaezi MF, Vandenplas Y, Vieira MC, Walker MM, Wechsler JB, Wershil BK, Wen T, Yang GY, Hirano I, Bredenoord AJ (October 2018). "Updated International Consensus Diagnostic Criteria for Eosinophilic Esophagitis: Proceedings of the AGREE Conference". Gastroenterology 155 (4): 1022–1033.e10. doi:10.1053/j.gastro.2018.07.009. PMC 6174113. PMID 30009819. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6174113/.
- ↑ 5.0 5.1 Iacobuzio-Donahue, Christine A.; Montgomery, Elizabeth A. (2005). Gastrointestinal and Liver Pathology: A Volume in the Foundations in Diagnostic Pathology Series (1st ed.). Churchill Livingstone. pp. 19. ISBN 978-0443066573.
- ↑ Leslie C, Mews C, Charles A, Ravikumara M (April 2010). "Celiac disease and eosinophilic esophagitis: a true association". J. Pediatr. Gastroenterol. Nutr. 50 (4): 397–9. doi:10.1097/MPG.0b013e3181a70af4. PMID 19841598.
- ↑ 7.0 7.1 Dellon, ES.; Erichsen, R.; Pedersen, L.; Shaheen, NJ.; Baron, JA.; Sørensen, HT.; Vyberg, M. (Jan 2013). "Development and validation of a registry-based definition of eosinophilic esophagitis in Denmark.". World J Gastroenterol 19 (4): 503-10. doi:10.3748/wjg.v19.i4.503. PMID 23382628.
- ↑ Al-Hussaini, AA.; Semaan, T.; El Hag, IA.. "Esophageal trachealization: a feature of eosinophilic esophagitis.". Saudi J Gastroenterol 15 (3): 193-5. doi:10.4103/1319-3767.54747. PMID 19636182.
- ↑ URL: http://www.ajronline.org/cgi/reprint/164/4/900.pdf. Accessed on: 4 October 2010.
- ↑ Cotran, Ramzi S.; Kumar, Vinay; Fausto, Nelson; Nelso Fausto; Robbins, Stanley L.; Abbas, Abul K. (2005). Robbins and Cotran pathologic basis of disease (7th ed.). St. Louis, Mo: Elsevier Saunders. pp. 804. ISBN 0-7216-0187-1.
- ↑ Odze, Robert D.; Goldblum, John R. (2009). Surgical pathology of the GI tract, liver, biliary tract and pancreas (2nd ed.). Saunders. pp. 244. ISBN 978-1416040590.