Difference between revisions of "Ditzels"
(more SO) |
|||
| (218 intermediate revisions by the same user not shown) | |||
| Line 1: | Line 1: | ||
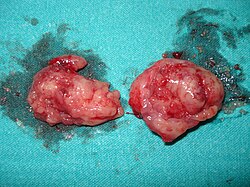
[[Image:Tonsillectomy tonsils.JPEG|thumb|right|220px|Tonsils (at [[cut-up]]) are a common ditzel. ([[WC]]/Katotomichelakis ''et al.'')]] | |||
This article collects '''ditzels''', which are, in the context of [[pathology]], little specimens that are typically one or two slides and usually of little interest.<ref>{{Ref TPoSP|37}}</ref> | This article collects '''ditzels''', which are, in the context of [[pathology]], little specimens that are typically one or two slides and usually of little interest.<ref>{{Ref TPoSP|37}}</ref> | ||
The challenge in ditzels is not falling asleep... so one misses the unexpected (subtle) tumour. | The challenge in ditzels is not falling asleep... so one misses the unexpected (subtle) tumour. | ||
= | =The big table of ditzels= | ||
= | {| class="wikitable sortable" | ||
! Specimen | |||
! Typical context (diagnosis) | |||
! System | |||
|- | |||
| [[Hernia sac]] | |||
| hernia | |||
| [[Gastrointestinal pathology]] | |||
|- | |||
| [[Stoma]] (reversal) | |||
| bowel obstruction, perforated viscus ([[peritonitis]]) | |||
| [[Gastrointestinal pathology]] | |||
|- | |||
| [[Sleeve gastrectomy]] | |||
| [[obesity]] | |||
| [[Gastrointestinal pathology]] | |||
|- | |||
| [[Vertebral disc]] | |||
| herniated disc | |||
| [[Neuropathology]] | |||
|- | |||
| [[Bands of Ladd]] | |||
| [[bands of Ladd]] | |||
| [[Paediatric pathology]] | |||
|- | |||
| [[Cholesteatoma]] | |||
| [[cholesteatoma]] | |||
| [[Paediatric pathology]] | |||
|- | |||
| [[Femoral head]] | |||
| [[hip fracture]], hip [[osteoarthritis|OA]] | |||
| Orthopaedic | |||
|- | |||
| [[Bone reamings]] | |||
| [[hip fracture]] | |||
| Orthopaedic | |||
|- | |||
| [[Tonsil]] | |||
| [[tonsillitis]] | |||
| [[Head and neck pathology]] | |||
|- | |||
| [[Leg amputation]] | |||
| [[atherosclerotic peripheral vascular disease]], trauma | |||
| [[Cardiovascular pathology]] | |||
|- | |||
| [[Lipoma]] | |||
| lipoma | |||
| [[Soft tissue pathology]] | |||
|- | |||
| [[Heterotopic ossification]] | |||
| contractures | |||
| [[Soft tissue pathology]] | |||
|- | |||
| Uterine tubes ([[tubal ligation]]) | |||
| completed family | |||
| [[Gynecologic pathology]] | |||
|- | |||
| [[Pressure ulcer]] ([[AKA]] decubitus ulcer) | |||
| [[ulcer]], immobility | |||
| [[Dermatopathology]] | |||
|- | |||
| Vas deferens ([[vasectomy]]) | |||
| completed family | |||
| [[Genitourinary pathology]] | |||
|- | |||
| [[Uvula]] | |||
| [[obstructive sleep apnea]] | |||
| [[Head and neck pathology]] | |||
|- | |||
| [[Stapes]] | |||
| [[otosclerosis]] | |||
| [[Head and neck pathology]] | |||
|- | |||
| [[Abdominal pannus]] | |||
| [[obesity]] | |||
| [[Dermatopathology]] (?) | |||
|- | |||
| [[Abdominal fat pad biopsy|Abdominal fat]] | |||
| query [[amyloidosis]] | |||
| [[Haematopathology]] (?) | |||
|- | |||
| [[Breast prosthesis]] | |||
| breast cancer/cosmesis | |||
| [[Breast pathology]] | |||
|- | |||
| [[Empyema peel]] | |||
| decortication for [[pneumonia]] | |||
| [[Pulmonary pathology]] | |||
|- | |||
| [[Bursa]] | |||
| [[bursitis]] | |||
| Orthopaedic | |||
|- | |||
| [[Gastric band]] | |||
| [[obesity]] | |||
| [[Gastrointestinal pathology]] | |||
|- | |||
| Small bowel excised during [[Roux-en-Y gastric bypass]] | |||
| [[obesity]] | |||
| [[Gastrointestinal pathology]] | |||
|- | |||
| [[Uterine isthmocele]]/cesarean scar defect | |||
| post-cesarean section | |||
| [[Gynecologic pathology]] | |||
|- | |||
| [[Distal interosseous nerve]] (''[[posterior interosseous nerve]] of wrist'' and ''[[anterior interosseous nerve]] of wrist'') | |||
| chronic hand pain, as may be seen in [[rheumatoid arthritis]] | |||
| [[Neuropathology]] | |||
|- | |||
| [[Palmar fascia]] | |||
| [[palmar fibromatosis]] (Dupuytren's contracture) | |||
| Plastic surgery | |||
|- | |||
| Soft tissue of hand or wrist | |||
| [[Ganglion cyst]] | |||
| Plastic surgery | |||
|- <!-- | |||
| Specimen | |||
| Typical context (diagnosis) | |||
| System --> | |||
|} | |||
=Gastrointestinal pathology= | =Gastrointestinal pathology= | ||
==Hernia sac== | ==Hernia sac== | ||
:''Inguinal hernia'' redirects here. | |||
===General=== | ===General=== | ||
*Hernia repair. | *Hernia repair (herniorrhaphy). | ||
*Pathologic findings are very unusual and if present known to the surgeon. | *Pathologic findings are very unusual and if present known to the surgeon. | ||
**Thus, it has been advocated that one ought not examine 'em.<ref name=pmid14986035>{{cite journal |author=Siddiqui K, Nazir Z, Ali SS, Pervaiz S |title=Is routine histological evaluation of pediatric hernial sac necessary? |journal=Pediatr. Surg. Int. |volume=20 |issue=2 |pages=133–5 |year=2004 |month=February |pmid=14986035 |doi=10.1007/s00383-003-1106-2 |url=}}</ref><ref name=pmid9694100>{{cite journal |author=Partrick DA, Bensard DD, Karrer FM, Ruyle SZ |title=Is routine pathological evaluation of pediatric hernia sacs justified? |journal=J. Pediatr. Surg. |volume=33 |issue=7 |pages=1090–2; discussion 1093–4 |year=1998 |month=July |pmid=9694100 |doi= |url=}}</ref> | **Thus, it has been advocated that one ought not examine 'em.<ref name=pmid14986035>{{cite journal |author=Siddiqui K, Nazir Z, Ali SS, Pervaiz S |title=Is routine histological evaluation of pediatric hernial sac necessary? |journal=Pediatr. Surg. Int. |volume=20 |issue=2 |pages=133–5 |year=2004 |month=February |pmid=14986035 |doi=10.1007/s00383-003-1106-2 |url=}}</ref><ref name=pmid9694100>{{cite journal |author=Partrick DA, Bensard DD, Karrer FM, Ruyle SZ |title=Is routine pathological evaluation of pediatric hernia sacs justified? |journal=J. Pediatr. Surg. |volume=33 |issue=7 |pages=1090–2; discussion 1093–4 |year=1998 |month=July |pmid=9694100 |doi= |url=}}</ref> | ||
| Line 68: | Line 157: | ||
====Mesothelial lining present==== | ====Mesothelial lining present==== | ||
<pre> | |||
Submitted as "Hernia Sac", Excision: | |||
- Benign fibroadipose tissue partially covered by mesothelium, consistent | |||
with hernia sac. | |||
- NEGATIVE for malignancy. | |||
</pre> | |||
======Block letters====== | |||
<pre> | <pre> | ||
SOFT TISSUE ("HERNIA SAC"), RESECTION/HERNIA REPAIR: | SOFT TISSUE ("HERNIA SAC"), RESECTION/HERNIA REPAIR: | ||
| Line 80: | Line 177: | ||
INFLAMMATION AND REACTIVE CHANGES -- CONSISTENT WITH HERNIA SAC. | INFLAMMATION AND REACTIVE CHANGES -- CONSISTENT WITH HERNIA SAC. | ||
- NEGATIVE FOR MALIGNANCY. | - NEGATIVE FOR MALIGNANCY. | ||
</pre> | |||
=====Gross only===== | |||
<pre> | |||
SOFT TISSUE, RIGHT INGUINAL, HERNIA REPAIR: | |||
- HERNIA SAC (GROSS ONLY). | |||
</pre> | |||
<pre> | |||
SOFT TISSUE, LEFT INGUINAL, HERNIA REPAIR: | |||
- HERNIA SAC (GROSS ONLY). | |||
</pre> | </pre> | ||
==Stoma== | ==Stoma== | ||
:''Ostomy'', ''ileostomy'' and ''colostomy'' redirect here. | |||
===General=== | |||
:See: ''[[Colon]]'' and ''[[Small intestine]]''. | :See: ''[[Colon]]'' and ''[[Small intestine]]''. | ||
*Reversal of ''ileostomy'' or ''colostomy''. | *Reversal of ''ileostomy'' or ''colostomy''. | ||
**The (generic) encompassing term for ''ileostomy'' and ''colostomy'' is ''ostomy''.<ref>URL: [http://www.nlm.nih.gov/medlineplus/ostomy.html http://www.nlm.nih.gov/medlineplus/ostomy.html]. Accessed on: 27 January 2013.</ref> | |||
Stomas are | Stomas are created for a number of reasons: | ||
*Perforated viscous/peritonitis. | *Perforated viscous/peritonitis. | ||
**Trauma. | **Trauma. | ||
| Line 99: | Line 209: | ||
**+/-Fibromuscular hyperplasia of the lamina propria and submucosa. | **+/-Fibromuscular hyperplasia of the lamina propria and submucosa. | ||
*Skin. | *Skin. | ||
**Typically has findings of mild irritation: | |||
***Mild dermal inflammation (usu. lymphocyte predominant). | |||
***[[Acanthosis]] (thickened ''[[stratum spinosum]]''). | |||
***Hypergranulosis (thickened ''[[stratum granulosum]]''). | |||
***Hyperkeratosis (thickened ''[[stratum corneum]]''). | |||
Notes: | Notes: | ||
| Line 108: | Line 223: | ||
===Sign out=== | ===Sign out=== | ||
====Colostomy==== | |||
<pre> | <pre> | ||
COLOSTOMY, COLOSTOMY REVERSAL: | COLOSTOMY, COLOSTOMY REVERSAL: | ||
- LARGE BOWEL WALL WITH SUBMUCOSAL FIBROSIS -- OTHERWISE WITHIN NORMAL LIMITS. | - LARGE BOWEL WALL WITH SUBMUCOSAL FIBROSIS -- OTHERWISE WITHIN NORMAL LIMITS. | ||
- SKIN WITHOUT SIGNIFICANT PATHOLOGY. | |||
- NEGATIVE FOR DYSPLASIA AND NEGATIVE FOR MALIGNANCY. | |||
</pre> | |||
====Ileostomy==== | |||
<pre> | |||
Submitted as "Ileostomy", Excision: | |||
- Small bowel with submucosal fibrosis, otherwise within normal limits. | |||
- Skin without significant pathology. | |||
- NEGATIVE for dysplasia and NEGATIVE for malignancy. | |||
</pre> | |||
=====Alternate===== | |||
<pre> | |||
Submitted As "Ileostomy", Excision: | |||
- Consistent with ileostomy (small bowel, skin) without significant pathology. | |||
- NEGATIVE for dysplasia and NEGATIVE for malignancy. | |||
</pre> | |||
=====Block letters===== | |||
<pre> | |||
ILEOSTOMY, ILEOSTOMY REVERSAL: | |||
- SMALL BOWEL WALL WITH SUBMUCOSAL FIBROSIS -- OTHERWISE WITHIN NORMAL LIMITS. | |||
- SKIN WITHOUT SIGNIFICANT PATHOLOGY. | - SKIN WITHOUT SIGNIFICANT PATHOLOGY. | ||
- NEGATIVE FOR DYSPLASIA AND NEGATIVE FOR MALIGNANCY. | - NEGATIVE FOR DYSPLASIA AND NEGATIVE FOR MALIGNANCY. | ||
| Line 147: | Line 286: | ||
COMMENT: | COMMENT: | ||
The tissue was stained with desmin and S-100; it is positive for desmin. S-100 marks only small nerves fibres that innervate the muscle. | The tissue was stained with desmin and S-100; it is positive for desmin. S-100 marks only | ||
small nerves fibres that innervate the muscle. | |||
</pre> | </pre> | ||
| Line 155: | Line 295: | ||
*Associated with intestinal malrotation. | *Associated with intestinal malrotation. | ||
*Removed by ''Ladd's procedure''. | *Removed by ''Ladd's procedure''. | ||
*Usually associated with [[duodenal]] and (other) [[small bowel obstruction]]s.<ref name=pmid20223332>{{Cite journal | last1 = Raphaeli | first1 = T. | last2 = Parimi | first2 = C. | last3 = Mattix | first3 = K. | last4 = Javid | first4 = PJ. | title = Acute colonic obstruction from Ladd bands: a unique complication from intestinal malrotation. | journal = J Pediatr Surg | volume = 45 | issue = 3 | pages = 630-1 | month = Mar | year = 2010 | doi = 10.1016/j.jpedsurg.2009.12.026 | PMID = 20223332 }} | |||
</ref> | |||
===Microscopic=== | ===Microscopic=== | ||
Features: | Features: | ||
*Benign fibrous tissue. | *Benign fibrous tissue. | ||
===Sign out=== | |||
<pre> | |||
Adhesive band, Ladd's procedure: | |||
- Vascular fibrous tissue consistent with bands of Ladd. | |||
</pre> | |||
==Cholesteatoma== | ==Cholesteatoma== | ||
{{Main|Cholesteatoma}} | |||
=Genitourinary pathology= | =Genitourinary pathology= | ||
| Line 186: | Line 322: | ||
*[[Lichen sclerosus]], [[AKA]] ''balanitis xerotica obliterans''. | *[[Lichen sclerosus]], [[AKA]] ''balanitis xerotica obliterans''. | ||
*[[Lichen planus]]. | *[[Lichen planus]]. | ||
*Infection, e.g. [[syphilis]]. | *Infection, e.g. [[syphilis]], [[candidiasis]]. | ||
*[[Zoon balanitis]] - abundant [[plasma cell]]s. | |||
===Microscopic=== | ===Microscopic=== | ||
| Line 195: | Line 332: | ||
DDx: | DDx: | ||
*See ''[[Penis]]. | *See ''[[Penis]]. | ||
===Sign out=== | |||
<pre> | |||
Foreskin, Circumcision: | |||
- Benign squamous mucosa within normal limits, consistent with foreskin. | |||
</pre> | |||
<pre> | |||
A. Foreskin, Circumcision: | |||
- Benign squamous mucosa without significant histopathology, consistent with foreskin. | |||
</pre> | |||
<pre> | |||
Foreskin, Circumcision: | |||
- Benign squamous mucosa with mild patchy chronic inflammation at the epidermal-dermal interface. | |||
- NEGATIVE for dysplasia and NEGATIVE for malignancy. | |||
</pre> | |||
<pre> | |||
Foreskin, Circumcision: | |||
- Squamous mucosa with mild-to-moderate acute and chronic | |||
(lymphocytic) lichenoid inflammation. | |||
- NEGATIVE for evidence of lichen sclerosus. | |||
- NEGATIVE for dysplasia and NEGATIVE for malignancy. | |||
Comment: | |||
A PASD stain is NEGATIVE for micro-organisms. | |||
</pre> | |||
====Micro==== | |||
The section shows squamous mucosa with mild basal pigmentation and subepithelial fibrous tissue. The epithelium matures to the surface. Significant inflammation is ABSENT. Atypia is ABSENT. | |||
==Paraurethral cyst== | ==Paraurethral cyst== | ||
{{Main|Paraurethral cyst}} | |||
==Labia== | |||
===General=== | ===General=== | ||
* | *Operation ''labioplasty''. | ||
===Microscopic=== | ===Microscopic=== | ||
Features: | Features: | ||
* | *Squamous epithelium with compact keratin. | ||
*Fibrous stroma. | |||
===Sign out=== | |||
<pre> | |||
LABIA MINORA, RIGHT, LABIOPLASTY: | |||
- BENIGN SKIN WITH A THIN LAYER OF COMPACT KERATIN FIBROTIC STROMA -- CONSISTENT | |||
WITH LABIA MINORA. | |||
</pre> | |||
=Head and neck pathology= | =Head and neck pathology= | ||
==Tonsillitis== | ==Tonsillitis== | ||
:'' | {{Main|Tonsillitis}} | ||
{{Main|Tonsil}} | |||
==Obstructive sleep apnea== | |||
:''Uvula'' redirects here. | |||
*Abbreviated ''OSA''. | |||
===General=== | ===General=== | ||
* | *Clinical diagnosis. | ||
* | *May be treated with a resection of the uvula.<ref name=pmid19467416>{{Cite journal | last1 = Shin | first1 = SH. | last2 = Ye | first2 = MK. | last3 = Kim | first3 = CG. | title = Modified uvulopalatopharyngoplasty for the treatment of obstructive sleep apnea-hypopnea syndrome: resection of the musculus uvulae. | journal = Otolaryngol Head Neck Surg | volume = 140 | issue = 6 | pages = 924-9 | month = Jun | year = 2009 | doi = 10.1016/j.otohns.2009.01.020 | PMID = 19467416 }}</ref> | ||
*Associated with [[obesity]].<ref name=pmid23299507>{{Cite journal | last1 = Sarkhosh | first1 = K. | last2 = Switzer | first2 = NJ. | last3 = El-Hadi | first3 = M. | last4 = Birch | first4 = DW. | last5 = Shi | first5 = X. | last6 = Karmali | first6 = S. | title = The Impact of Bariatric Surgery on Obstructive Sleep Apnea: A Systematic Review. | journal = Obes Surg | volume = | issue = | pages = | month = Jan | year = 2013 | doi = 10.1007/s11695-012-0862-2 | PMID = 23299507 }}</ref> | |||
=== | |||
===Microscopic=== | ===Microscopic=== | ||
Features: | Features: | ||
* | *Benign oropharyneal mucosa (stratified squamous epithelium). | ||
*+/- | *+/-Skeletal muscle. | ||
*+/-[[Salivary gland]]s (minor) - mucinous. | |||
* | |||
===Sign out=== | ===Sign out=== | ||
<pre> | <pre> | ||
UVULA, RESECTION: | |||
- | - OROPHARYNGEAL MUCOSA, CONSISTENT WITH UVULA. | ||
</pre> | </pre> | ||
| Line 259: | Line 411: | ||
{{Main|Cardiovascular pathology}} | {{Main|Cardiovascular pathology}} | ||
==Vascular thrombus== | ==Vascular thrombus== | ||
{{Main|Vascular thrombus}} | |||
==Leg amputation== | |||
{{Main|Leg amputation}} | |||
=== | ==Toe amputation== | ||
===General - overview=== | |||
*Like leg ampuations. | |||
* | |||
=== | ===Sign out=== | ||
:See ''[[Ditzels#Atherosclerotic peripheral vascular disease]]''. | |||
==Finger amputation== | |||
* | ===General - overview=== | ||
*Similar to [[toe amputation]]s. | |||
May be done due to: | |||
* | *Contractures leading to ulcerations. | ||
*[[Scleroderma]] - leading to ischemia.<ref name=pmid3584887>{{Cite journal | last1 = Jones | first1 = NF. | last2 = Imbriglia | first2 = JE. | last3 = Steen | first3 = VD. | last4 = Medsger | first4 = TA. | title = Surgery for scleroderma of the hand. | journal = J Hand Surg Am | volume = 12 | issue = 3 | pages = 391-400 | month = May | year = 1987 | doi = | PMID = 3584887 }}</ref> | |||
===Sign out=== | ===Sign out=== | ||
:See ''[[Ditzels#Atherosclerotic peripheral vascular disease]]''. | |||
==Atherosclerotic peripheral vascular disease== | ==Atherosclerotic peripheral vascular disease== | ||
:''Diabetic foot'' redirects here. | |||
*[[AKA]] ''peripheral vascular disease''. | |||
{{Main|Atherosclerosis}} | {{Main|Atherosclerosis}} | ||
===General=== | ===General=== | ||
| Line 326: | Line 443: | ||
===Gross=== | ===Gross=== | ||
*+/-Ulceration. | *+/-Ulceration. | ||
*+/-Gangrene - black skin - subclassified: | *+/-[[Gangrene]] - black skin - subclassified: | ||
**"Wet" = moist/oozing fluid. | **"Wet" = moist/oozing fluid. | ||
**"Dry" = shriveled, no moisture apparent. | **"Dry" = shriveled, no moisture apparent. | ||
*+/-Loss of hair. | *+/-Loss of hair. | ||
DDx - gross: | |||
*[[Malignant melanoma]]. | |||
Image: | Image: | ||
| Line 359: | Line 479: | ||
*Drug use, e.g. [[cocaine]].<ref name=pmid17059855>{{Cite journal | last1 = Dhawan | first1 = SS. | last2 = Wang | first2 = BW. | title = Four-extremity gangrene associated with crack cocaine abuse. | journal = Ann Emerg Med | volume = 49 | issue = 2 | pages = 186-9 | month = Feb | year = 2007 | doi = 10.1016/j.annemergmed.2006.08.001 | PMID = 17059855 }}</ref> | *Drug use, e.g. [[cocaine]].<ref name=pmid17059855>{{Cite journal | last1 = Dhawan | first1 = SS. | last2 = Wang | first2 = BW. | title = Four-extremity gangrene associated with crack cocaine abuse. | journal = Ann Emerg Med | volume = 49 | issue = 2 | pages = 186-9 | month = Feb | year = 2007 | doi = 10.1016/j.annemergmed.2006.08.001 | PMID = 17059855 }}</ref> | ||
*[[Chronic osteomyelitis]]. | *[[Chronic osteomyelitis]]. | ||
*[[Cholesterol embolism]]. | |||
===Sign out=== | ===Sign out=== | ||
====Forefoot amputation==== | |||
<pre> | |||
RIGHT FOREFOOT, AMPUTATION: | |||
- ULCERATED SKIN. | |||
- MODERATE-TO-SEVERE ATHEROSCLEROSIS. | |||
- BLOOD VESSEL WITH RECANALIZATION. | |||
- NEGATIVE FOR MALIGNANCY. | |||
</pre> | |||
====Leg amputation==== | |||
<pre> | <pre> | ||
LEFT LEG, BELOW KNEE AMPUTATION: | LEFT LEG, BELOW KNEE AMPUTATION: | ||
| Line 368: | Line 500: | ||
- MARROW CAVITY FIBROSIS WITH SIDEROPHAGES. | - MARROW CAVITY FIBROSIS WITH SIDEROPHAGES. | ||
- RESECTION MARGIN WITH VIABLE TISSUE. | - RESECTION MARGIN WITH VIABLE TISSUE. | ||
</pre> | |||
=====Revision===== | |||
<pre> | |||
SKIN AND SOFT TISSUE, RIGHT UPPER LEG, REVISION OF AMPUTATION: | |||
- ULCERATED SKIN WITH NECROTIC SOFT TISSUE WITH IMPETIGINIZATION, AND MICROABSCESS | |||
FORMATION. | |||
- SEVERE ATHEROSCLEROSIS. | |||
- NEGATIVE FOR MALIGNANCY. | |||
</pre> | |||
=====Leg amputation - gross only===== | |||
<pre> | |||
LOWER EXTREMITY, LEFT, BELOW THE KNEE AMPUTATION: | |||
- ULCERS AND ISCHEMIC CHANGES WITH FOCAL COMPLETE ARTERIAL OCCLUSION (GROSS ONLY). | |||
</pre> | |||
<pre> | |||
LEG, RIGHT, ABOVE THE KNEE AMPUTATION: | |||
- ULCERS AND ISCHEMIC CHANGES WITH EXTENSIVE ARTERIAL DISEASE (GROSS ONLY). | |||
</pre> | |||
<pre> | |||
LEG, RIGHT, ABOVE THE KNEE AMPUTATION: | |||
- EXTENSIVE ISCHEMIC CHANGES WITH SEVERE ARTERIAL DISEASE (GROSS ONLY). | |||
</pre> | |||
====Toe amputation==== | |||
=====Mild===== | |||
<pre> | |||
THIRD TOE, RIGHT, AMPUTATION: | |||
- SKIN WITH MARKED DERMAL FIBROSIS. | |||
- MILD ATHEROSCLEROSIS. | |||
- NEGATIVE FOR MALIGNANCY. | |||
</pre> | |||
<pre> | |||
SECOND TOE, RIGHT, AMPUTATION: | |||
- SKIN WITH MARKED DERMAL FIBROSIS AND ULCERATION WITH IMPETIGINIZATION. | |||
- MILD ATHEROSCLEROSIS. | |||
- NEGATIVE FOR MALIGNANCY. | |||
</pre> | |||
=====Moderate===== | |||
<pre> | |||
SECOND TOE, LEFT, AMPUTATION: | |||
- MODERATE ATHEROSCLEROSIS. | |||
- BONE WITH A FATTY BONE MARROW CAVITY WITH FOCAL FAT NECROSIS AND RARE PLASMA CELLS. | |||
- SKIN WITH FIBROUS DERMIS AND A NON-SPECIFIC DERMAL PERIVASCULAR LYMPHOPLASMACYTIC | |||
INFILTRATE. | |||
</pre> | |||
<pre> | |||
SECOND TOE, LEFT, AMPUTATION: | |||
- MODERATE ATHEROSCLEROSIS. | |||
- BONE WITH A FATTY BONE MARROW CAVITY WITH FOCAL FAT NECROSIS AND RARE PLASMA CELLS. | |||
- SKIN WITH FIBROUS DERMIS AND NON-SPECIFIC PERIVASCULAR LYMPHOPLASMACYTIC DERMAL INFILTRATE. | |||
</pre> | |||
=====Severe===== | |||
<pre> | |||
SECOND AND THIRD TOE, LEFT, AMPUTATION: | |||
- SEVERE ATHEROSCLEROSIS. | |||
- ACUTE AND CHRONIC OSTEOMYELITIS. | |||
- GANGRENE. | |||
</pre> | |||
<pre> | |||
GREAT TOE, LEFT, AMPUTATION: | |||
- GANGRENE. | |||
- SEVERE ATHEROSCLEROSIS. | |||
- ULCERATED SKIN AND CHRONIC ISCHEMIC CHANGES. | |||
- BONE WITH NO SIGNIFICANT PATHOLOGY. | |||
- NEGATIVE FOR MALIGNANCY. | |||
</pre> | |||
<pre> | |||
GREAT TOE, RIGHT, AMPUTATION: | |||
- GANGRENE. | |||
- ATHEROSCLEROSIS. | |||
- NECROTIC BONE WITH ABUNDANT COCCI ORGANISMS AND NEUTROPHILS | |||
WITHIN THE MARROW CAVITY. | |||
- NEGATIVE FOR MALIGNANCY. | |||
</pre> | </pre> | ||
| Line 402: | Line 617: | ||
==Heterotopic ossification== | ==Heterotopic ossification== | ||
*Abbreviated ''HO''. | *Abbreviated ''HO''. | ||
{{Main|Heterotopic ossification}} | |||
==Lumbar bone== | |||
===General=== | |||
*May be seen in the context of laminectomies to treat cauda equina syndrome. | |||
===Microscopic=== | |||
Features: | |||
*Degenerative fibrocartilage: | |||
**Multiple chondrocytes in one pocket (lacuna) - regenerative change. | |||
**Degenerative cartilage. | |||
*Non-vital bone: | |||
**Empty lacuna. | |||
DDx: | |||
*Occult malignancy. | |||
===Sign out=== | |||
<pre> | |||
LUMBAR BONE, DECOMPRESSION: | |||
- BONE AND VERTEBRAL DISC FRAGMENTS WITH DEGENERATIVE CHANGES. | |||
- UNREMARKABLE BONE MARROW. | |||
- NEGATIVE FOR MALIGNANCY. | |||
</pre> | |||
==Bursa== | |||
:''Bursitis'' redirects here. | |||
===General=== | |||
*Uncommon specimen. | |||
*Septic bursitis is usually due to ''S. aureus''.<ref name=pmid23933823>{{Cite journal | last1 = Hanrahan | first1 = JA. | title = Recent developments in septic bursitis. | journal = Curr Infect Dis Rep | volume = 15 | issue = 5 | pages = 421-5 | month = Oct | year = 2013 | doi = 10.1007/s11908-013-0353-1 | PMID = 23933823 }}</ref> | |||
**Usually associated with trauma to the overlying skin.<ref name=pmid439118>{{Cite journal | last1 = Canoso | first1 = JJ. | last2 = Sheckman | first2 = PR. | title = Septic subcutaneous bursitis. Report of sixteen cases. | journal = J Rheumatol | volume = 6 | issue = 1 | pages = 96-102 | month = | year = | doi = | PMID = 439118 }}</ref> | |||
Indication: | |||
*Bursitis - may be treated with bursectomy.<ref>{{Cite journal | last1 = Dillon | first1 = JP. | last2 = Freedman | first2 = I. | last3 = Tan | first3 = JS. | last4 = Mitchell | first4 = D. | last5 = English | first5 = S. | title = Endoscopic bursectomy for the treatment of septic pre-patellar bursitis: a case series. | journal = Arch Orthop Trauma Surg | volume = 132 | issue = 7 | pages = 921-5 | month = Jul | year = 2012 | doi = 10.1007/s00402-012-1494-7 | PMID = 22426936 }}</ref> | |||
Note: | |||
*Most bursitis is managed conservatively.<ref name=pmid21814140>{{Cite journal | last1 = Lustenberger | first1 = DP. | last2 = Ng | first2 = VY. | last3 = Best | first3 = TM. | last4 = Ellis | first4 = TJ. | title = Efficacy of treatment of trochanteric bursitis: a systematic review. | journal = Clin J Sport Med | volume = 21 | issue = 5 | pages = 447-53 | month = Sep | year = 2011 | doi = 10.1097/JSM.0b013e318221299c | PMID = 21814140 }}</ref> | |||
===Microscopic=== | |||
Features: | |||
*Dense connective tissue. | |||
*Fibroadipose tissue. | |||
===Sign out=== | |||
====No apparent inflammation==== | |||
<pre> | |||
BURSA, RIGHT HIP, BURSECTOMY: | |||
- BENIGN DENSE CONNECTIVE TISSUE WITH CALCIFICATIONS, AND FIBROADIPOSE TISSUE. | |||
- NO SIGNIFICANT INFLAMMATION. | |||
- NEGATIVE FOR MALIGNANCY. | |||
</pre> | |||
<pre> | |||
BURSA, LEFT TROCHANTERIC, BURSECTOMY: | |||
- BENIGN DENSE CONNECTIVE TISSUE AND BENIGN FIBROADIPOSE TISSUE. | |||
- NO SIGNIFICANT INFLAMMATION. | |||
- NEGATIVE FOR MALIGNANCY. | |||
</pre> | |||
==Rotator cuff tear== | |||
===General=== | |||
*Surgically repaired. | |||
*[[Clinical diagnosis]]. | |||
===Microscopic=== | |||
Features:<ref>{{Cite journal | last1 = Longo | first1 = UG. | last2 = Berton | first2 = A. | last3 = Khan | first3 = WS. | last4 = Maffulli | first4 = N. | last5 = Denaro | first5 = V. | title = Histopathology of rotator cuff tears. | journal = Sports Med Arthrosc | volume = 19 | issue = 3 | pages = 227-36 | month = Sep | year = 2011 | doi = 10.1097/JSA.0b013e318213bccb | PMID = 21822106 }}</ref> | |||
*Collagen degeneration. | |||
*Disordered arrangement of collagen fibres. | |||
**Wavy fibres. | |||
**Separation of the fibres. | |||
*+/-Inflammation - associated with smaller tears. | |||
*+/-Decreased cellularity - associated with larger tears. | |||
*+/-Fatty replacement.<ref name=pmid24084435>{{Cite journal | last1 = Kuzel | first1 = BR. | last2 = Grindel | first2 = S. | last3 = Papandrea | first3 = R. | last4 = Ziegler | first4 = D. | title = Fatty infiltration and rotator cuff atrophy. | journal = J Am Acad Orthop Surg | volume = 21 | issue = 10 | pages = 613-23 | month = Oct | year = 2013 | doi = 10.5435/JAAOS-21-10-613 | PMID = 24084435 }}</ref> | |||
===Sign out=== | |||
<pre> | |||
RIGHT SHOULDER ACROMIOM AND BURSAE, EXCISION: | |||
- UNREMARKABLE BONE (GROSS ONLY). | |||
- BENIGN SOFT TISSUE. | |||
</pre> | |||
<pre> | |||
"BURSA AND ACROMION", LEFT SHOULDER, ROTATOR CUFF REPAIR: | |||
- BENIGN DENSE CONNECTIVE TISSUE AND BENIGN FIBROADIPOSE TISSUE. | |||
- NO SIGNIFICANT INFLAMMATION. | |||
- NO BONE IDENTIFIED. | |||
- NEGATIVE FOR MALIGNANCY. | |||
</pre> | |||
<pre> | |||
"BURSA AND ACROMION", LEFT SHOULDER, ROTATOR CUFF REPAIR: | |||
- BENIGN DENSE WAVY CONNECTIVE TISSUE WITH FIBRE SEPARATION. | |||
- BENIGN FIBROADIPOSE TISSUE. | |||
- NO SIGNIFICANT INFLAMMATION. | |||
- NO BONE IDENTIFIED. | |||
- NEGATIVE FOR MALIGNANCY. | |||
</pre> | |||
=Other= | |||
==Breast prosthesis== | |||
*[[AKA]] ''breast implants''. | |||
{{Main|Breast prostheses}} | |||
==De Quervain syndrome== | |||
:Should ''not'' be confused with ''[[De Quervain's thyroiditis]]'' (subacute granulomatous thryoiditis). | |||
*[[AKA]] ''de Quervain tenosynovitis'',<ref name=pmid23405595>{{Cite journal | last1 = Gigante | first1 = MR. | last2 = Martinotti | first2 = I. | last3 = Cirla | first3 = PE. | title = [Computer work and De Quervain's tenosynovitis: an evidence based approach]. | journal = G Ital Med Lav Ergon | volume = 34 | issue = 3 Suppl | pages = 116-8 | month = | year = | doi = | PMID = 23405595 }}</ref> and ''de Quervain disease''. | |||
===General=== | |||
*Benign. | |||
*[[Tenosynovitis]] of the thumb. | |||
*Clinical diagnosis.<ref name=pmid18063716>{{Cite journal | last1 = Ilyas | first1 = AM. | last2 = Ilyas | first2 = A. | last3 = Ast | first3 = M. | last4 = Schaffer | first4 = AA. | last5 = Thoder | first5 = J. | title = De quervain tenosynovitis of the wrist. | journal = J Am Acad Orthop Surg | volume = 15 | issue = 12 | pages = 757-64 | month = Dec | year = 2007 | doi = | PMID = 18063716 }}</ref> | |||
Clinical: | |||
*Pain. | |||
Treatment:<ref name=pmid18063716/> | |||
*Steroid. | |||
*Surgery. | |||
===Microscopic=== | |||
Features: | |||
*Dense connective tissue consistent with tendon. | |||
===Sign out=== | |||
====Not apparent==== | |||
<pre> | |||
FIRST EXTENSOR COMPARTMENT, RIGHT HAND, BIOPSY: | |||
- DENSE CONNECTIVE TISSUE CONSISTENT WITH TENDON. | |||
- FIBROUS TISSUE. | |||
</pre> | |||
==Tenosynovitis== | |||
{{Main|Tenosynovitis}} | |||
==Otosclerosis== | |||
:''Stapes'' redirects here. | |||
===General=== | ===General=== | ||
* | *Clinical diagnosis. | ||
</ref> | *Causes conductive hearing loss.<ref name=pmid17245017>{{Cite journal | last1 = Declau | first1 = F. | last2 = van Spaendonck | first2 = M. | last3 = Timmermans | first3 = JP. | last4 = Michaels | first4 = L. | last5 = Liang | first5 = J. | last6 = Qiu | first6 = JP. | last7 = van de Heyning | first7 = P. | title = Prevalence of histologic otosclerosis: an unbiased temporal bone study in Caucasians. | journal = Adv Otorhinolaryngol | volume = 65 | issue = | pages = 6-16 | month = | year = 2007 | doi = 10.1159/000098663 | PMID = 17245017 }}</ref> | ||
* | *Etiology - genetic. | ||
*May be | **Over half a dozen genes have been identified.<ref name=omim166800>{{OMIM|166800}}</ref><ref name=omim605727>{{OMIM|605727}}</ref> | ||
**Classically described as ''autosomal dominant''. | |||
Treatment: | |||
*Stapedectomy (removal of the stapes).<ref name=pmid22771999>{{Cite journal | last1 = Redfors | first1 = YD. | last2 = Gröndahl | first2 = HG. | last3 = Hellgren | first3 = J. | last4 = Lindfors | first4 = N. | last5 = Nilsson | first5 = I. | last6 = Möller | first6 = C. | title = Otosclerosis: anatomy and pathology in the temporal bone assessed by multi-slice and cone-beam CT. | journal = Otol Neurotol | volume = 33 | issue = 6 | pages = 922-7 | month = Aug | year = 2012 | doi = 10.1097/MAO.0b013e318259b38c | PMID = 22771999 }}</ref> | |||
===Microscopic=== | |||
Features (temporal bone):<ref name=pmid620199>{{Cite journal | title = Otosclerosis. | journal = Br Med J | volume = 1 | issue = 6105 | pages = 63-4 | month = Jan | year = 1978 | doi = | PMID = 620199 | PMC = 1602666 | URL = http://www.ncbi.nlm.nih.gov/pmc/articles/PMC1602666/?page=1 }}</ref> | |||
*Classically divided into four phases: | |||
*#Osteoclastic phase: | |||
*#*Large spaces form in bone marrow. | |||
*#Replacement phase: | |||
*#*Bone replaced by basophilic web-like tissue. | |||
*#Fibril phase: | |||
*#*Fibrils deposited. | |||
*#Lamellar phase: | |||
*#*[[Lamellar bone]] forms around the blood vessels. | |||
Features - (stapes): | |||
*Unremarkable bone.{{fact}} | |||
DDx: | |||
*[[Avascular necrosis]] ~ 25% of cases diagnosed as ''otosclerosis''.<ref name=pmid620199/> | |||
**May be due to [[fat embolism]]. | |||
Note: | |||
*Avascular necrosis of the stapes crura and otosclerosis together is considered rare.<ref>{{Cite journal | last1 = Erdoglija | first1 = M. | last2 = Sotirovic | first2 = J. | last3 = Jacimovic | first3 = V. | last4 = Vukomanovic | first4 = B. | title = Avascular necrosis of stapes crura in one case of operated otosclerosis. | journal = Acta Medica (Hradec Kralove) | volume = 55 | issue = 4 | pages = 193-7 | month = | year = 2012 | doi = | PMID = 23631292 | URL = ftp://orbis.lfhk.cuni.cz/Acta_Medica/2012/2012_193.pdf}}</ref> | |||
Images: | |||
*[http://commons.wikimedia.org/wiki/File:Gray918.png Stapes - sketch (WC)]. | |||
===Sign out=== | |||
<pre> | |||
STAPES, RIGHT, STAPEDECTOMY: | |||
- BENIGN BONE CONSISTENT WITH STAPES. | |||
</pre> | |||
<pre> | |||
STAPES, RIGHT, STAPEDECTOMY: | |||
- UNREMARKABLE BONE CONSISTENT WITH STAPES. | |||
</pre> | |||
====Missed stapes==== | |||
<pre> | |||
STAPES, RIGHT, STAPEDECTOMY: | |||
- BENIGN FIBROFATTY TISSUE. | |||
- NO BONE IDENTIFIED. | |||
</pre> | |||
===External links=== | |||
*[http://otopathologynetwork.org/tbimages/chapter15/?page=3 Otosclerosis (otopathologynetwork.org)]. | |||
==Abdominal pannus== | |||
*[[AKA]] ''pannus'', ''panniculus'' and ''pannona''. | |||
{{Main|Abdominal pannus}} | |||
==Empyema== | |||
:''Empyema peel'' and ''pleural peel'' redirect here. | |||
===General=== | |||
*Empyemas are often managed surgically.<ref name=pmid10197399>{{Cite journal | last1 = Ferguson | first1 = MK. | title = Surgical management of intrapleural infections. | journal = Semin Respir Infect | volume = 14 | issue = 1 | pages = 73-81 | month = Mar | year = 1999 | doi = | PMID = 10197399 }}</ref> | |||
*Classically, divided into three stages.<ref name=pmid20628845>{{Cite journal | last1 = Shiraishi | first1 = Y. | title = Surgical treatment of chronic empyema. | journal = Gen Thorac Cardiovasc Surg | volume = 58 | issue = 7 | pages = 311-6 | month = Jul | year = 2010 | doi = 10.1007/s11748-010-0599-6 | PMID = 20628845 }}</ref><ref>{{Cite journal | last1 = Hamm | first1 = H. | last2 = Light | first2 = RW. | title = Parapneumonic effusion and empyema. | journal = Eur Respir J | volume = 10 | issue = 5 | pages = 1150-6 | month = May | year = 1997 | doi = | PMID = 9163661 | url = http://erj.ersjournals.com/content/10/5/1150.long }}</ref> | |||
**I - ''exudative stage'' (acute). | |||
**II - ''fibropurulent stage'' (acute). | |||
**III - ''organizational stage'' (chronic). | |||
Etiologies - common: | |||
* | *[[Pneumonia]] - most common. | ||
* | *Iatrogenic. | ||
* | *Trauma. | ||
===Microscopic=== | ===Microscopic=== | ||
Features: | Features: | ||
* | *Neutrophils (pus) - '''key feature'''. | ||
* | *Lymphocytes. | ||
*Plasma cells. | |||
*Reactive fibroblasts. | |||
*Reactive mesothelial cells - not common. | |||
DDx: | DDx: | ||
*[[ | *[[Malignant mesothelioma]] - should have infiltrative growth. | ||
*[[ | *[[Fibrosing pleuritis]]. | ||
===Sign out=== | ===Sign out=== | ||
<pre> | <pre> | ||
A. Right Pleural, Pleural Peel: | |||
- | - Proliferative fibroblasts with marked reactive changes. | ||
- Necro-inflammatory debris. | |||
- NEGATIVE for evidence of malignancy. | |||
B. Right Lung, Biopsy: | |||
- Necro-inflammatory debris and reactive pleural changes. | |||
- Infarcted lung parenchyma. | |||
- NEGATIVE for evidence of malignancy. | |||
</pre> | |||
====Block letters==== | |||
<pre> | |||
PLEURA, LEFT, DECORTICATION: | |||
- MIXED INFLAMMATORY INFILTRATE WITH ABUNDANT NEUTROPHILS. | |||
- REACTIVE FIBROBLASTS AND FIBRIN. | |||
- NO MICROORGANISMS APPARENT WITH H&E STAINING. | |||
- NEGATIVE FOR MALIGNANCY. | - NEGATIVE FOR MALIGNANCY. | ||
</pre> | </pre> | ||
====Micro==== | ====Not labelled as a peel==== | ||
The sections show | <pre> | ||
Left Lung, Biopsy: | |||
- Fibrin, neutrophils, necrotic tissue and a fibroblastic | |||
response, compatible with empyema peel. | |||
- NO viable lung parenchyma identified. | |||
- NEGATIVE for evidence of malignancy. | |||
</pre> | |||
==Toenail== | |||
===General=== | |||
*Relatively common. | |||
Indications for removal: | |||
*Ingrown<ref name=pmid23227941>{{Cite journal | last1 = Küçüktaş | first1 = M. | last2 = Kutlubay | first2 = Z. | last3 = Yardimci | first3 = G. | last4 = Khatib | first4 = R. | last5 = Tüzün | first5 = Y. | title = Comparison of effectiveness of electrocautery and cryotherapy in partial matrixectomy after partial nail extraction in the treatment of ingrown nails. | journal = Dermatol Surg | volume = 39 | issue = 2 | pages = 274-80 | month = Feb | year = 2013 | doi = 10.1111/dsu.12068 | PMID = 23227941 }}</ref> - typically great toe.<ref name=pmid24063180>{{Cite journal | last1 = Jia | first1 = C. | last2 = Li | first2 = P. | last3 = Wu | first3 = Y. | last4 = Qiu | first4 = Y. | last5 = Cao | first5 = L. | last6 = Chang | first6 = C. | last7 = Zhang | first7 = Y. | title = [Modified surgical repair of severe ingrown toenail]. | journal = Zhongguo Xiu Fu Chong Jian Wai Ke Za Zhi | volume = 27 | issue = 7 | pages = 869-71 | month = Jul | year = 2013 | doi = | PMID = 24063180 }}</ref> | |||
*Onychomycosis - [[fungus|fungal]] infection.<ref name=pmid12752134>{{Cite journal | last1 = Reisberger | first1 = EM. | last2 = Abels | first2 = C. | last3 = Landthaler | first3 = M. | last4 = Szeimies | first4 = RM. | title = Histopathological diagnosis of onychomycosis by periodic acid-Schiff-stained nail clippings. | journal = Br J Dermatol | volume = 148 | issue = 4 | pages = 749-54 | month = Apr | year = 2003 | doi = | PMID = 12752134 }}</ref> | |||
*Pigmented lesion. | |||
**Exclude melanoma.<ref name=pmid23153047>{{Cite journal | last1 = Fanti | first1 = PA. | last2 = Dika | first2 = E. | last3 = Misciali | first3 = C. | last4 = Vaccari | first4 = S. | last5 = Barisani | first5 = A. | last6 = Piraccini | first6 = BM. | last7 = Cavrin | first7 = G. | last8 = Maibach | first8 = HI. | last9 = Patrizi | first9 = A. | title = Nail apparatus melanoma: is trauma a coincidence? Is this peculiar tumor a real acral melanoma? | journal = Cutan Ocul Toxicol | volume = 32 | issue = 2 | pages = 150-3 | month = Jun | year = 2013 | doi = 10.3109/15569527.2012.740118 | PMID = 23153047 }}</ref> | |||
===Microscopic=== | |||
Features: | |||
*Nail plate - paucicellular, dense connective tissue. | |||
*Keratinized squamous epithelium. | |||
*+/-Cocci organisms. | |||
DDx: | |||
*[[Malignant melanoma]]. | |||
*Trauma. | |||
*[[Fungus|Fungal infection]] ([[candidiasis]]). | |||
*Bacteria infection, e.g. [[Pseudomonas]] (causes green nails). | |||
===Stains=== | |||
For pigmented lesion: | |||
*[[Prussian blue stain]] - trauma +ve, melanocytic lesion -ve. | |||
*[[Fontana-Masson stain]] - trauma -ve, melanocytic lesion usu. +ve. | |||
Query fungal infection: | |||
*[[PAS]] +ve for fungal organisms.<ref name=pmid12752134>{{Cite journal | last1 = Reisberger | first1 = EM. | last2 = Abels | first2 = C. | last3 = Landthaler | first3 = M. | last4 = Szeimies | first4 = RM. | title = Histopathological diagnosis of onychomycosis by periodic acid-Schiff-stained nail clippings. | journal = Br J Dermatol | volume = 148 | issue = 4 | pages = 749-54 | month = Apr | year = 2003 | doi = | PMID = 12752134 }}</ref> | |||
===Sign out=== | |||
====Pigmented nail==== | |||
<pre> | |||
PARTIAL NAIL PLATE, RIGHT THIRD TOE, SCISSOR EXCISION: | |||
- NAIL PLATE AND THIN LAYER OF KERATINIZED SQUAMOUS EPITHELIUM WITH | |||
PARAKERATOSIS AND FIBRIN. | |||
- NO APPARENT PIGMENT. | |||
- NO EVIDENCE OF MALIGNANCY. | |||
</pre> | |||
=====Micro===== | |||
The sections show a paucicellular nail plate, and a thin layer of squamous epithelium with | |||
keratinization and partial retention of the nuclei (parakeratosis). There is also a small | |||
amount of fibrin. No pigmentation is apparent with Prussian blue and Fontana-Masson | |||
staining. No melanocytes are apparent. No nuclear atypia is apparent. No mitotic activity | |||
is identified. No microorganisms are apparent. No significant inflammation is apparent. | |||
====Query infection==== | |||
<pre> | |||
GREAT TOENAIL, RIGHT, EXCISION: | |||
- NAIL PLATE AND THIN LAYER OF KERATINIZED SQUAMOUS EPITHELIUM. | |||
- SMALL CLUSTERS OF COCCI, FOCAL. | |||
- NO APPARENT FUNGAL ORGANISMS WITH PASF STAIN. | |||
- NO EVIDENCE OF MALIGNANCY. | |||
</pre> | |||
====Fungal organisms present==== | |||
<pre> | |||
GREAT TOE NAIL, RIGHT, REMOVAL: | |||
- NAIL PLATE AND THIN LAYER OF KERATINIZED SQUAMOUS EPITHELIUM WITH | |||
PARAKERATOSIS AND SCANT SUBEPITHELIAL TISSUE. | |||
- FUNGAL ORGANISMS CONSISTENT WITH CANDIDA, DEMONSTRATED WITH PASF STAIN. | |||
- SMALL CLUSTERS OF COCCI, FOCAL. | |||
- NO EVIDENCE OF MALIGNANCY. | |||
</pre> | |||
==Canal of Nuck cyst== | |||
===General=== | |||
*Canal of Nuck is the female equivalent of the male ''processus vaginalis''.<ref name=pmid36295514/> | |||
*Women/girls only pathology - can be thought of as inguinal hernia in women. | |||
*Very rare pathology.<ref name=pmid36295514>{{cite journal |authors=Kohlhauser M, Pirsch JV, Maier T, Viertler C, Fegerl R |title=The Cyst of the Canal of Nuck: Anatomy, Diagnostic and Treatment of a Very Rare Diagnosis-A Case Report of an Adult Woman and Narrative Review of the Literature |journal=Medicina (Kaunas) |volume=58 |issue=10 |pages= |date=September 2022 |pmid=36295514 |pmc=9609622 |doi=10.3390/medicina58101353 |url=}}</ref> | |||
===Sign out=== | |||
<pre> | |||
A. Submitted as "Canal of Nuck Cyst", Excision:: | |||
- Benign fibroadipose tissue partially covered by mesothelium with inflammation, | |||
compatible with clinical impression of canal of Nuck cyst. | |||
- NEGATIVE for malignancy. | |||
</pre> | |||
==Palmar fascia== | |||
{{Main|Palmar fascia}} | |||
=See also= | =See also= | ||
| Line 440: | Line 961: | ||
[[Category:Basics]] | [[Category:Basics]] | ||
[[Category:Ditzels]] | |||
Latest revision as of 17:02, 2 July 2024
This article collects ditzels, which are, in the context of pathology, little specimens that are typically one or two slides and usually of little interest.[1]
The challenge in ditzels is not falling asleep... so one misses the unexpected (subtle) tumour.
The big table of ditzels
Gastrointestinal pathology
Hernia sac
- Inguinal hernia redirects here.
General
- Hernia repair (herniorrhaphy).
- Pathologic findings are very unusual and if present known to the surgeon.
Microscopic
Features:
- Fibrous tissue.
- +/-Adipose tissue.
- +/-Mesothelial cells.
Notes:
- One should not see vas deferens.
- Things worthy of some comment: granulation tissue, inflammation.
Sign out
Incarcerated without mesothelium
SOFT TISSUE ("HERNIA SAC"), RESECTION/HERNIA REPAIR:
- FIBROADIPOSE TISSUE WITH FAT NECROSIS -- CONSISTENT WITH HERNIA SAC.
- NEGATIVE FOR MALIGNANCY.
Micro
The sections show fibrofatty tissue with hemosiderin-laden macrophages, plump activated fibroblasts with pale staining nuclei, histiocytes with small nuclei and abundant grey vacuolated cytoplasm, fat necrosis and focal necrosis of the fibrous tissue.
Mesothelial lining present
Submitted as "Hernia Sac", Excision: - Benign fibroadipose tissue partially covered by mesothelium, consistent with hernia sac. - NEGATIVE for malignancy.
Block letters
SOFT TISSUE ("HERNIA SAC"), RESECTION/HERNIA REPAIR:
- FIBROADIPOSE TISSUE PARTIALLY COVERED BY MESOTHELIUM -- CONSISTENT WITH HERNIA SAC.
- NEGATIVE FOR MALIGNANCY.
Inflamed
SOFT TISSUE ("HERNIA SAC"), LEFT, RESECTION/HERNIA REPAIR:
- FIBROADIPOSE TISSUE PARTIALLY COVERED BY MESOTHELIUM WITH FOCAL CHRONIC
INFLAMMATION AND REACTIVE CHANGES -- CONSISTENT WITH HERNIA SAC.
- NEGATIVE FOR MALIGNANCY.
Gross only
SOFT TISSUE, RIGHT INGUINAL, HERNIA REPAIR: - HERNIA SAC (GROSS ONLY).
SOFT TISSUE, LEFT INGUINAL, HERNIA REPAIR: - HERNIA SAC (GROSS ONLY).
Stoma
- Ostomy, ileostomy and colostomy redirect here.
General
- See: Colon and Small intestine.
- Reversal of ileostomy or colostomy.
- The (generic) encompassing term for ileostomy and colostomy is ostomy.[4]
Stomas are created for a number of reasons:
- Perforated viscous/peritonitis.
- Trauma.
- Colorectal adenocarcinoma.
- Diverticulosis.
Microscopic
Features:
- Colonic-type or small intestinal-type bowel wall.
- Lymphoid hyperplasia (abundant lymphocytes) - very common.
- +/-Fibromuscular hyperplasia of the lamina propria and submucosa.
- Skin.
- Typically has findings of mild irritation:
- Mild dermal inflammation (usu. lymphocyte predominant).
- Acanthosis (thickened stratum spinosum).
- Hypergranulosis (thickened stratum granulosum).
- Hyperkeratosis (thickened stratum corneum).
- Typically has findings of mild irritation:
Notes:
- One is looking for malignancy (e.g. colorectal carcinoma), especially if that is in the history.
DDx:
Sign out
Colostomy
COLOSTOMY, COLOSTOMY REVERSAL: - LARGE BOWEL WALL WITH SUBMUCOSAL FIBROSIS -- OTHERWISE WITHIN NORMAL LIMITS. - SKIN WITHOUT SIGNIFICANT PATHOLOGY. - NEGATIVE FOR DYSPLASIA AND NEGATIVE FOR MALIGNANCY.
Ileostomy
Submitted as "Ileostomy", Excision: - Small bowel with submucosal fibrosis, otherwise within normal limits. - Skin without significant pathology. - NEGATIVE for dysplasia and NEGATIVE for malignancy.
Alternate
Submitted As "Ileostomy", Excision:
- Consistent with ileostomy (small bowel, skin) without significant pathology.
- NEGATIVE for dysplasia and NEGATIVE for malignancy.
Block letters
ILEOSTOMY, ILEOSTOMY REVERSAL: - SMALL BOWEL WALL WITH SUBMUCOSAL FIBROSIS -- OTHERWISE WITHIN NORMAL LIMITS. - SKIN WITHOUT SIGNIFICANT PATHOLOGY. - NEGATIVE FOR DYSPLASIA AND NEGATIVE FOR MALIGNANCY.
Vagus nerve
General
- Seen from vagotomy.
Typical indication:
- Gastric outlet obstruction.[5]
Notes:
- Left vagus nerve -> anterior vagal trunk.
- Right vagus nerve -> posterior vagal trunk.
Microscopic
Features:
- Peripheral nerve.
DDx:
- Smooth muscle.
IHC
- S-100 +ve.
- Desmin -ve.
Sign out
A. VAGUS NERVE, POSTERIOR, VAGOTOMY: - PERIPHERAL NERVE WITHIN NORMAL LIMITS. B. VAGUS NERVE, ANTERIOR, VAGOTOMY: - SMOOTH MUSCLE WITHIN NORMAL LIMITS. - PERIPHERAL NERVE NOT IDENTIFIED, SEE COMMENT. COMMENT: The tissue was stained with desmin and S-100; it is positive for desmin. S-100 marks only small nerves fibres that innervate the muscle.
Pediatric
Bands of Ladd
General
- Associated with intestinal malrotation.
- Removed by Ladd's procedure.
- Usually associated with duodenal and (other) small bowel obstructions.[6]
Microscopic
Features:
- Benign fibrous tissue.
Sign out
Adhesive band, Ladd's procedure: - Vascular fibrous tissue consistent with bands of Ladd.
Cholesteatoma
Genitourinary pathology
Foreskin
General
Indications:
Main considerations:
- Squamous cell carcinoma.
- Lichen sclerosus, AKA balanitis xerotica obliterans.
- Lichen planus.
- Infection, e.g. syphilis, candidiasis.
- Zoon balanitis - abundant plasma cells.
Microscopic
Features:
- Usu. fibrotic dermis.
- +/-Inflammation.
DDx:
- See Penis.
Sign out
Foreskin, Circumcision: - Benign squamous mucosa within normal limits, consistent with foreskin.
A. Foreskin, Circumcision: - Benign squamous mucosa without significant histopathology, consistent with foreskin.
Foreskin, Circumcision: - Benign squamous mucosa with mild patchy chronic inflammation at the epidermal-dermal interface. - NEGATIVE for dysplasia and NEGATIVE for malignancy.
Foreskin, Circumcision: - Squamous mucosa with mild-to-moderate acute and chronic (lymphocytic) lichenoid inflammation. - NEGATIVE for evidence of lichen sclerosus. - NEGATIVE for dysplasia and NEGATIVE for malignancy. Comment: A PASD stain is NEGATIVE for micro-organisms.
Micro
The section shows squamous mucosa with mild basal pigmentation and subepithelial fibrous tissue. The epithelium matures to the surface. Significant inflammation is ABSENT. Atypia is ABSENT.
Paraurethral cyst
Labia
General
- Operation labioplasty.
Microscopic
Features:
- Squamous epithelium with compact keratin.
- Fibrous stroma.
Sign out
LABIA MINORA, RIGHT, LABIOPLASTY: - BENIGN SKIN WITH A THIN LAYER OF COMPACT KERATIN FIBROTIC STROMA -- CONSISTENT WITH LABIA MINORA.
Head and neck pathology
Tonsillitis
Obstructive sleep apnea
- Uvula redirects here.
- Abbreviated OSA.
General
Microscopic
Features:
- Benign oropharyneal mucosa (stratified squamous epithelium).
- +/-Skeletal muscle.
- +/-Salivary glands (minor) - mucinous.
Sign out
UVULA, RESECTION: - OROPHARYNGEAL MUCOSA, CONSISTENT WITH UVULA.
Cardiovascular pathology
Vascular thrombus
Leg amputation
Toe amputation
General - overview
- Like leg ampuations.
Sign out
Finger amputation
General - overview
- Similar to toe amputations.
May be done due to:
- Contractures leading to ulcerations.
- Scleroderma - leading to ischemia.[9]
Sign out
Atherosclerotic peripheral vascular disease
- Diabetic foot redirects here.
- AKA peripheral vascular disease.
General
- Very strong association with diabetes mellitus.
Gross
- +/-Ulceration.
- +/-Gangrene - black skin - subclassified:
- "Wet" = moist/oozing fluid.
- "Dry" = shriveled, no moisture apparent.
- +/-Loss of hair.
DDx - gross:
Image:
Sections - grossing:
- Resection margin (check for viability).
- Gangrenous area.
- Blood vessels.
- Bone (check for osteomyelitis).
Microscopic
Features:
- Atherosclerosis.
- Coagulative necrosis (gangrene).
- Inflammation (wet gangrene).
- Neutrophils.
- Lymphocytes.
- Plasma cells.
- +/-Thrombosis.
- +/-Chronic osteomyelitis.
- +/-Reactive fibroblasts.
Note:
- Ischemia may be associated with marked nuclear changes. Uninitiated eyes may think they are seeing a sarcoma.
DDx:
- Vasculitis associated with a connective tissue disorder.
- Drug use, e.g. cocaine.[10]
- Chronic osteomyelitis.
- Cholesterol embolism.
Sign out
Forefoot amputation
RIGHT FOREFOOT, AMPUTATION: - ULCERATED SKIN. - MODERATE-TO-SEVERE ATHEROSCLEROSIS. - BLOOD VESSEL WITH RECANALIZATION. - NEGATIVE FOR MALIGNANCY.
Leg amputation
LEFT LEG, BELOW KNEE AMPUTATION: - MODERATE-TO-SEVERE ATHEROSCLEROSIS. - COAGULATIVE NECROSIS OF SOFT TISSUE. - NECROTIC BONE. - MARROW CAVITY FIBROSIS WITH SIDEROPHAGES. - RESECTION MARGIN WITH VIABLE TISSUE.
Revision
SKIN AND SOFT TISSUE, RIGHT UPPER LEG, REVISION OF AMPUTATION: - ULCERATED SKIN WITH NECROTIC SOFT TISSUE WITH IMPETIGINIZATION, AND MICROABSCESS FORMATION. - SEVERE ATHEROSCLEROSIS. - NEGATIVE FOR MALIGNANCY.
Leg amputation - gross only
LOWER EXTREMITY, LEFT, BELOW THE KNEE AMPUTATION: - ULCERS AND ISCHEMIC CHANGES WITH FOCAL COMPLETE ARTERIAL OCCLUSION (GROSS ONLY).
LEG, RIGHT, ABOVE THE KNEE AMPUTATION: - ULCERS AND ISCHEMIC CHANGES WITH EXTENSIVE ARTERIAL DISEASE (GROSS ONLY).
LEG, RIGHT, ABOVE THE KNEE AMPUTATION: - EXTENSIVE ISCHEMIC CHANGES WITH SEVERE ARTERIAL DISEASE (GROSS ONLY).
Toe amputation
Mild
THIRD TOE, RIGHT, AMPUTATION: - SKIN WITH MARKED DERMAL FIBROSIS. - MILD ATHEROSCLEROSIS. - NEGATIVE FOR MALIGNANCY.
SECOND TOE, RIGHT, AMPUTATION: - SKIN WITH MARKED DERMAL FIBROSIS AND ULCERATION WITH IMPETIGINIZATION. - MILD ATHEROSCLEROSIS. - NEGATIVE FOR MALIGNANCY.
Moderate
SECOND TOE, LEFT, AMPUTATION: - MODERATE ATHEROSCLEROSIS. - BONE WITH A FATTY BONE MARROW CAVITY WITH FOCAL FAT NECROSIS AND RARE PLASMA CELLS. - SKIN WITH FIBROUS DERMIS AND A NON-SPECIFIC DERMAL PERIVASCULAR LYMPHOPLASMACYTIC INFILTRATE.
SECOND TOE, LEFT, AMPUTATION: - MODERATE ATHEROSCLEROSIS. - BONE WITH A FATTY BONE MARROW CAVITY WITH FOCAL FAT NECROSIS AND RARE PLASMA CELLS. - SKIN WITH FIBROUS DERMIS AND NON-SPECIFIC PERIVASCULAR LYMPHOPLASMACYTIC DERMAL INFILTRATE.
Severe
SECOND AND THIRD TOE, LEFT, AMPUTATION: - SEVERE ATHEROSCLEROSIS. - ACUTE AND CHRONIC OSTEOMYELITIS. - GANGRENE.
GREAT TOE, LEFT, AMPUTATION: - GANGRENE. - SEVERE ATHEROSCLEROSIS. - ULCERATED SKIN AND CHRONIC ISCHEMIC CHANGES. - BONE WITH NO SIGNIFICANT PATHOLOGY. - NEGATIVE FOR MALIGNANCY.
GREAT TOE, RIGHT, AMPUTATION: - GANGRENE. - ATHEROSCLEROSIS. - NECROTIC BONE WITH ABUNDANT COCCI ORGANISMS AND NEUTROPHILS WITHIN THE MARROW CAVITY. - NEGATIVE FOR MALIGNANCY.
Orthopaedic
Femoral head
Bone reamings
General
- Taken during the surgical repair of a fracture, e.g. intramedullary nail placement.
- Done to rule-out a pathologic fracture; considered reliable for detecting malignancy.[11]
- Hassan et al.[12] advocate against their use, suggesting the yield is low and a biopsy should be preferred.
Microscopic
Features:[13]
- Fragments of bone (scattered trabeculae).
- Necrotic bone = bone with empty lacunae, i.e. lacunae missing osteocytes.
- Bone marrow.
- Megakaryocytes - large cells, multinucleated, eosinophilic cytoplasm.
- Nucleated RBCs - perfectly round, dense nucleus, bright red cytoplasm.
- Myeloid cells and precursors.
- Adipocytes.
DDx:
- Metastatic carcinoma.
Sign out
BONE, LEFT FEMUR, REAMINGS: - FEATURES CONSISTENT WITH A RECENT FRACTURE. - NEGATIVE FOR MALIGNANCY.
Heterotopic ossification
- Abbreviated HO.
Lumbar bone
General
- May be seen in the context of laminectomies to treat cauda equina syndrome.
Microscopic
Features:
- Degenerative fibrocartilage:
- Multiple chondrocytes in one pocket (lacuna) - regenerative change.
- Degenerative cartilage.
- Non-vital bone:
- Empty lacuna.
DDx:
- Occult malignancy.
Sign out
LUMBAR BONE, DECOMPRESSION: - BONE AND VERTEBRAL DISC FRAGMENTS WITH DEGENERATIVE CHANGES. - UNREMARKABLE BONE MARROW. - NEGATIVE FOR MALIGNANCY.
Bursa
- Bursitis redirects here.
General
- Uncommon specimen.
- Septic bursitis is usually due to S. aureus.[14]
- Usually associated with trauma to the overlying skin.[15]
Indication:
- Bursitis - may be treated with bursectomy.[16]
Note:
- Most bursitis is managed conservatively.[17]
Microscopic
Features:
- Dense connective tissue.
- Fibroadipose tissue.
Sign out
No apparent inflammation
BURSA, RIGHT HIP, BURSECTOMY: - BENIGN DENSE CONNECTIVE TISSUE WITH CALCIFICATIONS, AND FIBROADIPOSE TISSUE. - NO SIGNIFICANT INFLAMMATION. - NEGATIVE FOR MALIGNANCY.
BURSA, LEFT TROCHANTERIC, BURSECTOMY: - BENIGN DENSE CONNECTIVE TISSUE AND BENIGN FIBROADIPOSE TISSUE. - NO SIGNIFICANT INFLAMMATION. - NEGATIVE FOR MALIGNANCY.
Rotator cuff tear
General
- Surgically repaired.
- Clinical diagnosis.
Microscopic
Features:[18]
- Collagen degeneration.
- Disordered arrangement of collagen fibres.
- Wavy fibres.
- Separation of the fibres.
- +/-Inflammation - associated with smaller tears.
- +/-Decreased cellularity - associated with larger tears.
- +/-Fatty replacement.[19]
Sign out
RIGHT SHOULDER ACROMIOM AND BURSAE, EXCISION: - UNREMARKABLE BONE (GROSS ONLY). - BENIGN SOFT TISSUE.
"BURSA AND ACROMION", LEFT SHOULDER, ROTATOR CUFF REPAIR: - BENIGN DENSE CONNECTIVE TISSUE AND BENIGN FIBROADIPOSE TISSUE. - NO SIGNIFICANT INFLAMMATION. - NO BONE IDENTIFIED. - NEGATIVE FOR MALIGNANCY.
"BURSA AND ACROMION", LEFT SHOULDER, ROTATOR CUFF REPAIR: - BENIGN DENSE WAVY CONNECTIVE TISSUE WITH FIBRE SEPARATION. - BENIGN FIBROADIPOSE TISSUE. - NO SIGNIFICANT INFLAMMATION. - NO BONE IDENTIFIED. - NEGATIVE FOR MALIGNANCY.
Other
Breast prosthesis
- AKA breast implants.
De Quervain syndrome
- Should not be confused with De Quervain's thyroiditis (subacute granulomatous thryoiditis).
General
- Benign.
- Tenosynovitis of the thumb.
- Clinical diagnosis.[21]
Clinical:
- Pain.
Treatment:[21]
- Steroid.
- Surgery.
Microscopic
Features:
- Dense connective tissue consistent with tendon.
Sign out
Not apparent
FIRST EXTENSOR COMPARTMENT, RIGHT HAND, BIOPSY: - DENSE CONNECTIVE TISSUE CONSISTENT WITH TENDON. - FIBROUS TISSUE.
Tenosynovitis
Otosclerosis
- Stapes redirects here.
General
- Clinical diagnosis.
- Causes conductive hearing loss.[22]
- Etiology - genetic.
Treatment:
- Stapedectomy (removal of the stapes).[25]
Microscopic
Features (temporal bone):[26]
- Classically divided into four phases:
- Osteoclastic phase:
- Large spaces form in bone marrow.
- Replacement phase:
- Bone replaced by basophilic web-like tissue.
- Fibril phase:
- Fibrils deposited.
- Lamellar phase:
- Lamellar bone forms around the blood vessels.
- Osteoclastic phase:
Features - (stapes):
- Unremarkable bone.[citation needed]
DDx:
- Avascular necrosis ~ 25% of cases diagnosed as otosclerosis.[26]
- May be due to fat embolism.
Note:
- Avascular necrosis of the stapes crura and otosclerosis together is considered rare.[27]
Images:
Sign out
STAPES, RIGHT, STAPEDECTOMY: - BENIGN BONE CONSISTENT WITH STAPES.
STAPES, RIGHT, STAPEDECTOMY: - UNREMARKABLE BONE CONSISTENT WITH STAPES.
Missed stapes
STAPES, RIGHT, STAPEDECTOMY: - BENIGN FIBROFATTY TISSUE. - NO BONE IDENTIFIED.
External links
Abdominal pannus
- AKA pannus, panniculus and pannona.
Empyema
- Empyema peel and pleural peel redirect here.
General
- Empyemas are often managed surgically.[28]
- Classically, divided into three stages.[29][30]
- I - exudative stage (acute).
- II - fibropurulent stage (acute).
- III - organizational stage (chronic).
Etiologies - common:
- Pneumonia - most common.
- Iatrogenic.
- Trauma.
Microscopic
Features:
- Neutrophils (pus) - key feature.
- Lymphocytes.
- Plasma cells.
- Reactive fibroblasts.
- Reactive mesothelial cells - not common.
DDx:
- Malignant mesothelioma - should have infiltrative growth.
- Fibrosing pleuritis.
Sign out
A. Right Pleural, Pleural Peel:
- Proliferative fibroblasts with marked reactive changes.
- Necro-inflammatory debris.
- NEGATIVE for evidence of malignancy.
B. Right Lung, Biopsy:
- Necro-inflammatory debris and reactive pleural changes.
- Infarcted lung parenchyma.
- NEGATIVE for evidence of malignancy.
Block letters
PLEURA, LEFT, DECORTICATION: - MIXED INFLAMMATORY INFILTRATE WITH ABUNDANT NEUTROPHILS. - REACTIVE FIBROBLASTS AND FIBRIN. - NO MICROORGANISMS APPARENT WITH H&E STAINING. - NEGATIVE FOR MALIGNANCY.
Not labelled as a peel
Left Lung, Biopsy: - Fibrin, neutrophils, necrotic tissue and a fibroblastic response, compatible with empyema peel. - NO viable lung parenchyma identified. - NEGATIVE for evidence of malignancy.
Toenail
General
- Relatively common.
Indications for removal:
- Ingrown[31] - typically great toe.[32]
- Onychomycosis - fungal infection.[33]
- Pigmented lesion.
- Exclude melanoma.[34]
Microscopic
Features:
- Nail plate - paucicellular, dense connective tissue.
- Keratinized squamous epithelium.
- +/-Cocci organisms.
DDx:
- Malignant melanoma.
- Trauma.
- Fungal infection (candidiasis).
- Bacteria infection, e.g. Pseudomonas (causes green nails).
Stains
For pigmented lesion:
- Prussian blue stain - trauma +ve, melanocytic lesion -ve.
- Fontana-Masson stain - trauma -ve, melanocytic lesion usu. +ve.
Query fungal infection:
Sign out
Pigmented nail
PARTIAL NAIL PLATE, RIGHT THIRD TOE, SCISSOR EXCISION: - NAIL PLATE AND THIN LAYER OF KERATINIZED SQUAMOUS EPITHELIUM WITH PARAKERATOSIS AND FIBRIN. - NO APPARENT PIGMENT. - NO EVIDENCE OF MALIGNANCY.
Micro
The sections show a paucicellular nail plate, and a thin layer of squamous epithelium with keratinization and partial retention of the nuclei (parakeratosis). There is also a small amount of fibrin. No pigmentation is apparent with Prussian blue and Fontana-Masson staining. No melanocytes are apparent. No nuclear atypia is apparent. No mitotic activity is identified. No microorganisms are apparent. No significant inflammation is apparent.
Query infection
GREAT TOENAIL, RIGHT, EXCISION: - NAIL PLATE AND THIN LAYER OF KERATINIZED SQUAMOUS EPITHELIUM. - SMALL CLUSTERS OF COCCI, FOCAL. - NO APPARENT FUNGAL ORGANISMS WITH PASF STAIN. - NO EVIDENCE OF MALIGNANCY.
Fungal organisms present
GREAT TOE NAIL, RIGHT, REMOVAL: - NAIL PLATE AND THIN LAYER OF KERATINIZED SQUAMOUS EPITHELIUM WITH PARAKERATOSIS AND SCANT SUBEPITHELIAL TISSUE. - FUNGAL ORGANISMS CONSISTENT WITH CANDIDA, DEMONSTRATED WITH PASF STAIN. - SMALL CLUSTERS OF COCCI, FOCAL. - NO EVIDENCE OF MALIGNANCY.
Canal of Nuck cyst
General
- Canal of Nuck is the female equivalent of the male processus vaginalis.[35]
- Women/girls only pathology - can be thought of as inguinal hernia in women.
- Very rare pathology.[35]
Sign out
A. Submitted as "Canal of Nuck Cyst", Excision:: - Benign fibroadipose tissue partially covered by mesothelium with inflammation, compatible with clinical impression of canal of Nuck cyst. - NEGATIVE for malignancy.
Palmar fascia
See also
References
- ↑ Weedman Molavi, Diana (2008). The Practice of Surgical Pathology: A Beginner's Guide to the Diagnostic Process (1st ed.). Springer. pp. 37. ISBN 978-0387744858.
- ↑ Siddiqui K, Nazir Z, Ali SS, Pervaiz S (February 2004). "Is routine histological evaluation of pediatric hernial sac necessary?". Pediatr. Surg. Int. 20 (2): 133–5. doi:10.1007/s00383-003-1106-2. PMID 14986035.
- ↑ Partrick DA, Bensard DD, Karrer FM, Ruyle SZ (July 1998). "Is routine pathological evaluation of pediatric hernia sacs justified?". J. Pediatr. Surg. 33 (7): 1090–2; discussion 1093–4. PMID 9694100.
- ↑ URL: http://www.nlm.nih.gov/medlineplus/ostomy.html. Accessed on: 27 January 2013.
- ↑ Okawada, M.; Okazaki, T.; Takahashi, T.; Lane, GJ.; Yamataka, A. (2009). "Gastric outlet obstruction possibly secondary to ulceration in a 2-year-old girl: a case report.". Cases J 2 (1): 8. doi:10.1186/1757-1626-2-8. PMID 19123936.
- ↑ Raphaeli, T.; Parimi, C.; Mattix, K.; Javid, PJ. (Mar 2010). "Acute colonic obstruction from Ladd bands: a unique complication from intestinal malrotation.". J Pediatr Surg 45 (3): 630-1. doi:10.1016/j.jpedsurg.2009.12.026. PMID 20223332.
- ↑ Shin, SH.; Ye, MK.; Kim, CG. (Jun 2009). "Modified uvulopalatopharyngoplasty for the treatment of obstructive sleep apnea-hypopnea syndrome: resection of the musculus uvulae.". Otolaryngol Head Neck Surg 140 (6): 924-9. doi:10.1016/j.otohns.2009.01.020. PMID 19467416.
- ↑ Sarkhosh, K.; Switzer, NJ.; El-Hadi, M.; Birch, DW.; Shi, X.; Karmali, S. (Jan 2013). "The Impact of Bariatric Surgery on Obstructive Sleep Apnea: A Systematic Review.". Obes Surg. doi:10.1007/s11695-012-0862-2. PMID 23299507.
- ↑ Jones, NF.; Imbriglia, JE.; Steen, VD.; Medsger, TA. (May 1987). "Surgery for scleroderma of the hand.". J Hand Surg Am 12 (3): 391-400. PMID 3584887.
- ↑ Dhawan, SS.; Wang, BW. (Feb 2007). "Four-extremity gangrene associated with crack cocaine abuse.". Ann Emerg Med 49 (2): 186-9. doi:10.1016/j.annemergmed.2006.08.001. PMID 17059855.
- ↑ Clarke, AM.; Rogers, S.; Douglas, DL. (Dec 1993). "Closed intramedullary biopsy for metastatic disease.". J R Coll Surg Edinb 38 (6): 368-9. PMID 7509409.
- ↑ Hassan, K.; Kalra, S.; Moran, C. (Aug 2007). "Intramedullary reamings for the histological diagnosis of suspected pathological fractures.". Surgeon 5 (4): 202-4. PMID 17849954.
- ↑ Tydings, JD.; Martino, LJ.; Kircher, M.; Alfred, RH.; Lozman, J. (Mar 1987). "Viability of intramedullary canal bone reamings for continued calcification.". Am J Surg 153 (3): 306-9. PMID 3548454.
- ↑ Hanrahan, JA. (Oct 2013). "Recent developments in septic bursitis.". Curr Infect Dis Rep 15 (5): 421-5. doi:10.1007/s11908-013-0353-1. PMID 23933823.
- ↑ Canoso, JJ.; Sheckman, PR.. "Septic subcutaneous bursitis. Report of sixteen cases.". J Rheumatol 6 (1): 96-102. PMID 439118.
- ↑ Dillon, JP.; Freedman, I.; Tan, JS.; Mitchell, D.; English, S. (Jul 2012). "Endoscopic bursectomy for the treatment of septic pre-patellar bursitis: a case series.". Arch Orthop Trauma Surg 132 (7): 921-5. doi:10.1007/s00402-012-1494-7. PMID 22426936.
- ↑ Lustenberger, DP.; Ng, VY.; Best, TM.; Ellis, TJ. (Sep 2011). "Efficacy of treatment of trochanteric bursitis: a systematic review.". Clin J Sport Med 21 (5): 447-53. doi:10.1097/JSM.0b013e318221299c. PMID 21814140.
- ↑ Longo, UG.; Berton, A.; Khan, WS.; Maffulli, N.; Denaro, V. (Sep 2011). "Histopathology of rotator cuff tears.". Sports Med Arthrosc 19 (3): 227-36. doi:10.1097/JSA.0b013e318213bccb. PMID 21822106.
- ↑ Kuzel, BR.; Grindel, S.; Papandrea, R.; Ziegler, D. (Oct 2013). "Fatty infiltration and rotator cuff atrophy.". J Am Acad Orthop Surg 21 (10): 613-23. doi:10.5435/JAAOS-21-10-613. PMID 24084435.
- ↑ Gigante, MR.; Martinotti, I.; Cirla, PE.. "[Computer work and De Quervain's tenosynovitis: an evidence based approach].". G Ital Med Lav Ergon 34 (3 Suppl): 116-8. PMID 23405595.
- ↑ 21.0 21.1 Ilyas, AM.; Ilyas, A.; Ast, M.; Schaffer, AA.; Thoder, J. (Dec 2007). "De quervain tenosynovitis of the wrist.". J Am Acad Orthop Surg 15 (12): 757-64. PMID 18063716.
- ↑ Declau, F.; van Spaendonck, M.; Timmermans, JP.; Michaels, L.; Liang, J.; Qiu, JP.; van de Heyning, P. (2007). "Prevalence of histologic otosclerosis: an unbiased temporal bone study in Caucasians.". Adv Otorhinolaryngol 65: 6-16. doi:10.1159/000098663. PMID 17245017.
- ↑ Online 'Mendelian Inheritance in Man' (OMIM) 166800
- ↑ Online 'Mendelian Inheritance in Man' (OMIM) 605727
- ↑ Redfors, YD.; Gröndahl, HG.; Hellgren, J.; Lindfors, N.; Nilsson, I.; Möller, C. (Aug 2012). "Otosclerosis: anatomy and pathology in the temporal bone assessed by multi-slice and cone-beam CT.". Otol Neurotol 33 (6): 922-7. doi:10.1097/MAO.0b013e318259b38c. PMID 22771999.
- ↑ 26.0 26.1 "Otosclerosis.". Br Med J 1 (6105): 63-4. Jan 1978. PMC 1602666. PMID 620199. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1602666/.
- ↑ Erdoglija, M.; Sotirovic, J.; Jacimovic, V.; Vukomanovic, B. (2012). "Avascular necrosis of stapes crura in one case of operated otosclerosis.". Acta Medica (Hradec Kralove) 55 (4): 193-7. PMID 23631292.
- ↑ Ferguson, MK. (Mar 1999). "Surgical management of intrapleural infections.". Semin Respir Infect 14 (1): 73-81. PMID 10197399.
- ↑ Shiraishi, Y. (Jul 2010). "Surgical treatment of chronic empyema.". Gen Thorac Cardiovasc Surg 58 (7): 311-6. doi:10.1007/s11748-010-0599-6. PMID 20628845.
- ↑ Hamm, H.; Light, RW. (May 1997). "Parapneumonic effusion and empyema.". Eur Respir J 10 (5): 1150-6. PMID 9163661. http://erj.ersjournals.com/content/10/5/1150.long.
- ↑ Küçüktaş, M.; Kutlubay, Z.; Yardimci, G.; Khatib, R.; Tüzün, Y. (Feb 2013). "Comparison of effectiveness of electrocautery and cryotherapy in partial matrixectomy after partial nail extraction in the treatment of ingrown nails.". Dermatol Surg 39 (2): 274-80. doi:10.1111/dsu.12068. PMID 23227941.
- ↑ Jia, C.; Li, P.; Wu, Y.; Qiu, Y.; Cao, L.; Chang, C.; Zhang, Y. (Jul 2013). "[Modified surgical repair of severe ingrown toenail].". Zhongguo Xiu Fu Chong Jian Wai Ke Za Zhi 27 (7): 869-71. PMID 24063180.
- ↑ 33.0 33.1 Reisberger, EM.; Abels, C.; Landthaler, M.; Szeimies, RM. (Apr 2003). "Histopathological diagnosis of onychomycosis by periodic acid-Schiff-stained nail clippings.". Br J Dermatol 148 (4): 749-54. PMID 12752134.
- ↑ Fanti, PA.; Dika, E.; Misciali, C.; Vaccari, S.; Barisani, A.; Piraccini, BM.; Cavrin, G.; Maibach, HI. et al. (Jun 2013). "Nail apparatus melanoma: is trauma a coincidence? Is this peculiar tumor a real acral melanoma?". Cutan Ocul Toxicol 32 (2): 150-3. doi:10.3109/15569527.2012.740118. PMID 23153047.
- ↑ 35.0 35.1 Kohlhauser M, Pirsch JV, Maier T, Viertler C, Fegerl R (September 2022). "The Cyst of the Canal of Nuck: Anatomy, Diagnostic and Treatment of a Very Rare Diagnosis-A Case Report of an Adult Woman and Narrative Review of the Literature". Medicina (Kaunas) 58 (10). doi:10.3390/medicina58101353. PMC 9609622. PMID 36295514. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC9609622/.