Difference between revisions of "Papillary thyroid carcinoma"
m (→Micro) |
(BRAF) |
||
| (22 intermediate revisions by 3 users not shown) | |||
| Line 1: | Line 1: | ||
{{ Infobox diagnosis | {{ Infobox diagnosis | ||
| Name = {{PAGENAME}} | | Name = {{PAGENAME}} | ||
| Image = Papillary_thyroid_microcarcinoma_-_high_mag.jpg | | Image = Papillary_thyroid_microcarcinoma_-_high_mag.jpg | ||
| Width = | | Width = | ||
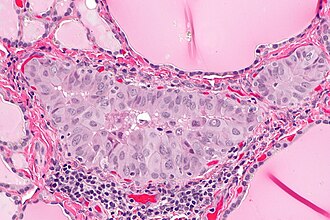
| Caption = Papillary thyroid carcinoma. [[H&E stain]]. | | Caption = Papillary thyroid carcinoma. [[H&E stain]]. | ||
| Micro = nuclear changes: nuclear membrane irregularities (e.g. raisinoid shape), +/-nuclear grooves, +/-[[nuclear pseudoinclusions]], +/-nuclear clearing, nuclear enlargement (usu. mild), nucleoli; architectural changes: overlap of nuclei, papillae (not required), +/-[[psammoma bodies]] | | Micro = nuclear changes: nuclear membrane irregularities (e.g. raisinoid shape), +/-nuclear grooves, +/-[[nuclear pseudoinclusions]], +/-nuclear clearing, nuclear enlargement (usu. mild), nucleoli; architectural changes: overlap of nuclei, papillae (not required), +/-[[psammoma bodies]] | ||
| Subtypes = [[Papillary thyroid carcinoma tall cell variant|tall cell variant]], [[Papillary thyroid carcinoma columnar cell variant|columnar cell variant]], [[Papillary thyroid carcinoma follicular variant|follicular variant]], [[Papillary thyroid carcinoma cribriform-morular variant|cribriform-morular variant]], [[Papillary thyroid carcinoma diffuse sclerosing variant|diffuse sclerosing variant]], [[Papillary thyroid carcinoma Warthin-like variant|Warthin-like variant]], [[Papillary thyroid carcinoma solid variant|solid variant]], [[Papillary thyroid carcinoma oncocytic variant|oncocytic variant]], others | | Subtypes = [[Papillary thyroid carcinoma tall cell variant|tall cell variant]], [[Papillary thyroid carcinoma columnar cell variant|columnar cell variant]], [[Papillary thyroid carcinoma follicular variant|follicular variant]], [[Papillary thyroid carcinoma cribriform-morular variant|cribriform-morular variant]], [[Papillary thyroid carcinoma diffuse sclerosing variant|diffuse sclerosing variant]], [[Papillary thyroid carcinoma Warthin-like variant|Warthin-like variant]], [[Papillary thyroid carcinoma solid variant|solid variant]], [[Papillary thyroid carcinoma oncocytic variant|oncocytic variant]], others | ||
| LMDDx = [[lymphocytic thyroiditis]] ([[Graves disease]], [[Hashimoto thyroiditis]]), [[solid cell nest of thyroid]], [[follicular thyroid carcinoma]], [[follicular thyroid adenoma]], [[adenomatoid nodule]] | | LMDDx = [[lymphocytic thyroiditis]] ([[Graves disease]], [[Hashimoto thyroiditis]]), [[solid cell nest of thyroid]], [[follicular thyroid carcinoma]], [[follicular thyroid adenoma]], [[adenomatoid nodule]], [[noninvasive follicular thyroid neoplasm with papillary-like nuclear features]] (NIFTP) | ||
| Stains = | | Stains = | ||
| IHC = HBME-1 +ve, | | IHC = HBME-1 +ve, [[CK19]] +ve, Galectin-3 +ve, thyroglobulin +ve, TTF-1 +ve | ||
| EM = | | EM = | ||
| Molecular = | | Molecular = BRAF mutation - commonly | ||
| IF = | | IF = | ||
| Gross = | | Gross = | ||
| Grossing = | | Grossing = | ||
| Staging = [[thyroid cancer staging]] | |||
| Site = [[thyroid gland]] | | Site = [[thyroid gland]] | ||
| Assdx = | | Assdx = | ||
| Line 76: | Line 77: | ||
*Nuclear inclusions are quite rare and not required to make the diagnosis -- but a very convincing feature if seen. | *Nuclear inclusions are quite rare and not required to make the diagnosis -- but a very convincing feature if seen. | ||
*Papillae may be seen in Graves disease. | *Papillae may be seen in Graves disease. | ||
*Thyroid tissue lateral to the jugular vein (often referred to as ''[[lateral aberrant thyroid tissue]]'') is generally considered metastatic thyroid carcinoma (papillary thyroid carcinoma) even if it looks benign.<ref name=pmid14452106>{{Cite journal | last1 = JOHNSON | first1 = RW. | last2 = SAHA | first2 = NC. | title = The so-called lateral aberrant thyroid. | journal = Br Med J | volume = 1 | issue = 5293 | pages = 1668-9 | month = Jun | year = 1962 | doi = | PMID = 14452106 | PMC = 1958877 }}</ref> | |||
**This dictum is disputed.<ref name=pmid17319317>{{Cite journal | last1 = Escofet | first1 = X. | last2 = Khan | first2 = AZ. | last3 = Mazarani | first3 = W. | last4 = Woods | first4 = WG. | title = Lessons to be learned: a case study approach. Lateral aberrant thyroid tissue: is it always malignant? | journal = J R Soc Promot Health | volume = 127 | issue = 1 | pages = 45-6 | month = Jan | year = 2007 | doi = | PMID = 17319317 }}</ref> | |||
**The level VI and VII [[lymph nodes]] are medial to the jugular. | |||
DDx: | DDx: | ||
| Line 146: | Line 150: | ||
DDx: | DDx: | ||
*[[Noninvasive follicular thyroid neoplasm with papillary-like nuclear features]] (NIFTP). | |||
*[[Follicular thyroid carcinoma]] - has a fibrous capsule and invasion though it. | *[[Follicular thyroid carcinoma]] - has a fibrous capsule and invasion though it. | ||
*[[Follicular thyroid adenoma]] - surrounded by a fibrous capsule. | *[[Follicular thyroid adenoma]] - surrounded by a fibrous capsule. | ||
| Line 151: | Line 156: | ||
Images: | Images: | ||
===Papillary thyroid carcinoma cribriform-morular variant=== | |||
=====General===== | =====General===== | ||
*Associated with [[familial adenomatous polyposis]] (FAP).<ref name=pmid18612695>{{cite journal |author=Groen EJ, Roos A, Muntinghe FL, ''et al.'' |title=Extra-intestinal manifestations of familial adenomatous polyposis |journal=Ann. Surg. Oncol. |volume=15 |issue=9 |pages=2439–50 |year=2008 |month=September |pmid=18612695 |pmc=2518080 |doi=10.1245/s10434-008-9981-3 |url=http://www.ncbi.nlm.nih.gov/pmc/articles/PMC2518080/?tool=pubmed}}</ref> | *Associated with [[familial adenomatous polyposis]] (FAP).<ref name=pmid18612695>{{cite journal |author=Groen EJ, Roos A, Muntinghe FL, ''et al.'' |title=Extra-intestinal manifestations of familial adenomatous polyposis |journal=Ann. Surg. Oncol. |volume=15 |issue=9 |pages=2439–50 |year=2008 |month=September |pmid=18612695 |pmc=2518080 |doi=10.1245/s10434-008-9981-3 |url=http://www.ncbi.nlm.nih.gov/pmc/articles/PMC2518080/?tool=pubmed}}</ref> | ||
| Line 161: | Line 163: | ||
=====Microscopic===== | =====Microscopic===== | ||
Features: | Features: | ||
* | *Circumscribed or even encapsulated neoplasm. | ||
*Morules - balls of | *Morules - interspersed balls of squamoid cells | ||
**No keritinization or intercellular bridges. | |||
**Homogenous, lightly eosinophilic glassy nuclei (biotin accumulation). | |||
*Follicles | |||
**[[Cribriform]], papillary, trabecular and solid patterns. | |||
**Columnar or cuboidal cells. | |||
**Little colloid | |||
**Papillary carcinoma nuclear features. | |||
<gallery> | |||
Image:Thyroid PapillaryCarcinoma CribriformMorularVariant MP3 13BR***.jpg|Thyroid - Papillary Carcinoma Cribriform Morular Variant - Medium power (SKB) | |||
Image:Thyroid PapillaryCarcinoma CribriformMorularVariant HP2 13BR***.jpg|Thyroid - Papillary Carcinoma Cribriform Morular Variant - High power (SKB) | |||
Image:Thyroid PapillaryCarcinoma CribriformMorularVariant HP3 13BR***.jpg|Thyroid - Papillary Carcinoma Cribriform Morular Variant - high power]] | |||
Image:Thyroid PapillaryCarcinoma CribriformMorularVariant P16 HP3 13BR***.jpg|Thyroid - Papillary Carcinoma Cribriform Morular Variant - High power (SKB) | |||
Image:Thyroid PapillaryCarcinoma CribriformMorularVariant CDX2 HP 13BR***.jpg|Thyroid - Papillary Carcinoma Cribriform Morular Variant - CDX2 (SKB) | |||
Image:Thyroid PapillaryCarcinoma CribriformMorularVariant P16 HP 13BR***.jpg|Thyroid - Papillary Carcinoma Cribriform Morular Variant - p16 (SKB) | |||
Image:Thyroid PapillaryCarcinoma CribriformMorularVariant ER HP 13BR***.jpg|Thyroid - Papillary Carcinoma Cribriform Morular Variant - ER (SKB) | |||
Image:Thyroid PapillaryCarcinoma CribriformMorularVariant betaCatenin HP 13BR***.jpg|Thyroid - Papillary Carcinoma Cribriform Morular Variant - beta catenin (SKB) | |||
</gallery> | |||
DDX: | |||
*Papillary thyroid carcinoma | |||
*Papillary thyroid carcinoma, tall cell variant | |||
=====IHC===== | |||
*CDX2 - Highlights the morules (CDX2 is positive in the biotin rich nuclei associated with morule formation in a variety of situations)<ref>{{Cite journal | last1 = Wani | first1 = Y. | last2 = Notohara | first2 = K. | last3 = Nakatani | first3 = Y. | last4 = Matsuzaki | first4 = A. | title = Aberrant nuclear Cdx2 expression in morule-forming tumours in different organs, accompanied by cytoplasmic reactivity. | journal = Histopathology | volume = 55 | issue = 4 | pages = 465-8 | month = Oct | year = 2009 | doi = 10.1111/j.1365-2559.2009.03382.x | PMID = 19817898 }}</ref> | |||
*CD10 - Highlights the morules <ref>{{Cite journal | last1 = Cameselle-Teijeiro | first1 = J. | last2 = Alberte-Lista | first2 = L. | last3 = Chiarelli | first3 = S. | last4 = Buriticá | first4 = C. | last5 = Gonçalves | first5 = L. | last6 = González-Cámpora | first6 = R. | last7 = Nogales | first7 = FF. | title = CD10 is a characteristic marker of tumours forming morules with biotin-rich, optically clear nuclei that occur in different organs. | journal = Histopathology | volume = 52 | issue = 3 | pages = 389-92 | month = Feb | year = 2008 | doi = 10.1111/j.1365-2559.2007.02911.x | PMID = 18081818 }}</ref> | |||
*Beta-catenin - nuclear and cytoplasmic - all tumour cells. | |||
*Estrogen receptor - positive | |||
*TTF-1 - positive | |||
=====Molecular===== | |||
*Up-regulating disturbances in the Wnt signaling pathway promote formation of morules with optically clear biotin rich nuclei <ref>{{Cite journal | last1 = Gamachi | first1 = A. | last2 = Kashima | first2 = K. | last3 = Daa | first3 = T. | last4 = Nakatani | first4 = Y. | last5 = Tsujimoto | first5 = M. | last6 = Yokoyama | first6 = S. | title = Aberrant intranuclear localization of biotin, biotin-binding enzymes, and beta-catenin in pregnancy-related endometrium and morule-associated neoplastic lesions. | journal = Mod Pathol | volume = 16 | issue = 11 | pages = 1124-31 | month = Nov | year = 2003 | doi = 10.1097/01.MP.0000092953.20717.48 | PMID = 14614052 }}</ref> | |||
**Mutation of the beta-catenin gene | |||
**Mutation in APC | |||
*Examples | |||
***Well-differentiated fetal adenocarcinoma | |||
***Papillary thyroid carcinoma, cribriform morular variant (mutation in APC in familial variants) | |||
***Pancreatoblastoma | |||
====Papillary thyroid carcinoma diffuse sclerosing variant==== | ====Papillary thyroid carcinoma diffuse sclerosing variant==== | ||
| Line 211: | Line 252: | ||
Note: | Note: | ||
*CK19 +ve -- though ''not'' specific or sensitive. | *CK19 +ve -- though ''not'' specific or sensitive. | ||
<gallery> | |||
Image: Papillary thyroid carcinoma oncocytic variant -- low mag.jpg | PTC oncocytic - low mag. (WC) | |||
Image: Papillary thyroid carcinoma oncocytic variant -- intermed mag.jpg | PTC oncocytic - intermed mag. (WC) | |||
Image: Papillary thyroid carcinoma oncocytic variant -- high mag.jpg | PTC oncocytic - high mag. (WC) | |||
Image: Papillary thyroid carcinoma oncocytic variant -- very high mag.jpg | PTC oncocytic - very high mag. (WC) | |||
</gallery> | |||
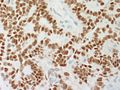
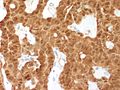
===IHC=== | ===IHC=== | ||
Thyroid versus something else: | Thyroid versus something else: | ||
*Thyroglobulin +ve. | *Thyroglobulin +ve.<ref name=pmid23637102>{{Cite journal | last1 = Sathiyamoorthy | first1 = S. | last2 = Maleki | first2 = Z. | title = Cytomorphologic overlap of differentiated thyroid carcinoma and lung adenocarcinoma and diagnostic value of TTF-1 and TGB on cytologic material. | journal = Diagn Cytopathol | volume = 42 | issue = 1 | pages = 5-10 | month = Jan | year = 2014 | doi = 10.1002/dc.22997 | PMID = 23637102 }}</ref> | ||
*TTF-1 (thyroid transcription factor-1) +ve. | *TTF-1 ([[thyroid transcription factor-1]]) +ve. | ||
*CD15 +ve.{{fact}} | *CD15 +ve.{{fact}} | ||
PTC versus benign:<ref>{{Cite journal | last1 = Mataraci | first1 = EA. | last2 = Ozgüven | first2 = BY. | last3 = Kabukçuoglu | first3 = F. | title = Expression of cytokeratin 19, HBME-1 and galectin-3 in neoplastic and nonneoplastic thyroid lesions. | journal = Pol J Pathol | volume = 63 | issue = 1 | pages = 58-64 | month = Mar | year = 2012 | doi = | PMID = 22535608 }}</ref> | PTC versus benign:<ref>{{Cite journal | last1 = Mataraci | first1 = EA. | last2 = Ozgüven | first2 = BY. | last3 = Kabukçuoglu | first3 = F. | title = Expression of cytokeratin 19, HBME-1 and galectin-3 in neoplastic and nonneoplastic thyroid lesions. | journal = Pol J Pathol | volume = 63 | issue = 1 | pages = 58-64 | month = Mar | year = 2012 | doi = | PMID = 22535608 }}</ref> | ||
*HBME-1 +ve (strong, diffuse). | *HBME-1 +ve (strong, diffuse). | ||
*CK19 +ve (strong, diffuse). | *[[CK19]] +ve (strong, diffuse). | ||
*Galectin-3 +ve (strong, diffuse). | *Galectin-3 +ve (strong, diffuse). | ||
===Molecular=== | ===Molecular=== | ||
* | *BRAF mutation.<ref name=pmid35670964>{{cite journal |authors=Lam AK |title=Papillary Thyroid Carcinoma: Current Position in Epidemiology, Genomics, and Classification |journal=Methods Mol Biol |volume=2534 |issue= |pages=1–15 |date=2022 |pmid=35670964 |doi=10.1007/978-1-0716-2505-7_1 |url=}}</ref> | ||
====Tabular summary==== | ====Tabular summary==== | ||
| Line 273: | Line 321: | ||
- PAPILLARY THYROID MICROCARCINOMA. | - PAPILLARY THYROID MICROCARCINOMA. | ||
-- MARGINS NEGATIVE FOR MALIGNANCY. | -- MARGINS NEGATIVE FOR MALIGNANCY. | ||
-- TUMOUR SIZE ~ 1 | -- TUMOUR SIZE ~ 1 MILLIMETRE. | ||
-- NEGATIVE FOR LYMPHOVASCULAR INVASION. | -- NEGATIVE FOR LYMPHOVASCULAR INVASION. | ||
-- NEGATIVE FOR PERINEURAL INVASION. | -- NEGATIVE FOR PERINEURAL INVASION. | ||
| Line 281: | Line 329: | ||
B. LYMPH NODES, LEVEL 6 AND 7, LYMPH NODE DISSECTION: | B. LYMPH NODES, LEVEL 6 AND 7, LYMPH NODE DISSECTION: | ||
- TWO LYMPH NODES, NEGATIVE FOR MALIGNANCY ( 0 POSITIVE / 2 ). | - TWO LYMPH NODES, NEGATIVE FOR MALIGNANCY ( 0 POSITIVE / 2 ). | ||
</pre> | |||
<pre> | |||
THYROID GLAND, TOTAL THYROIDECTOMY: | |||
- INCIDENTAL PAPILLARY THYROID MICROCARCINOMA. | |||
-- MARGINS NEGATIVE FOR MALIGNANCY. | |||
-- TUMOUR SIZE ~ 1 MILLIMETRE. | |||
-- NEGATIVE FOR LYMPHOVASCULAR INVASION. | |||
-- NEGATIVE FOR PERINEURAL INVASION. | |||
- NODULAR HYPERPLASIA. | |||
- ONE PARATHYROID GLAND. | |||
</pre> | </pre> | ||
Latest revision as of 17:44, 9 May 2024
Papillary thyroid carcinoma, abbreviated PTC, is the most common thyroid gland malignancy. It usually has an indolent course.
General
Medical school memory device P's:
- Palpable lymph nodes.
- Popular - most common malignant neoplasm of the thyroid.
- Prognosis is good.
- Pre-Tx iodine scan.
- Post-Sx iodine scan.
- Psammoma bodies.
Notes:
- PTC is associated with radiation exposure.[1]
- Papillary thyroid microcarcinoma is defined as a tumour with a maximal dimension of 1.0 cm or less.[2]
Prognosis
Prognosis can be predicted by MAICS score. It which includes:[3]
- Metastases.
- Age.
- Invasion of surround tissues.
- Completeness of excision.
- Size of tumour.
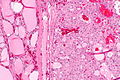
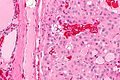
Microscopic
Features:
- Nuclear changes - key feature.
- "Shrivelled nuclei"/"raisin" like nuclei, nuclei with a wavy ("textured", convoluted) nuclear membrane -- usu. easy to find.
- Nuclear pseudoinclusions -- usu. harder to find; have high specificity (nuclear pseudoinclusions appear as a result of the very convoluted nuclear membrane wrapping around parts of the cytoplasm; true nuclear inclusions in contrast are seen only in viral infections).
- Nuclear grooves, seen as a result of the highly "textured" nuclear membrane.
- Nuclear clearing (only on permanent section) - also known as "Orphan Annie eyes".
- Overlap of nuclei - "cells do not respect each other's borders" (easy to see at key feature at low power).
- Classically has papillae (nipple-like shape); papilla (definition): epithelium on fibrovascular core.
- Absence of papillae does not exclude diagnosis.
- Psammoma bodies.
- Circular, acellular, eosinophilic whorled bodies.
- Not necessary to make diagnosis - but very specific in the context of a specimen labeled "thyroid".
- Arise from infarction & calcification of papilla tips.[4]
Notes:
- Psammoma bodies are awesome if you see 'em, i.e. useful for arriving at the diagnosis.
- If there are no papillae structures -- you're unlikely to see psammoma bodies.
- At low power look for cellular areas/loss of follicles.
- Nuclear clearing seen in:
- Nuclear overlapping is easy to see at lower power-- should be the tip-off to look at high power for nuclear features.
- Nuclear inclusions are quite rare and not required to make the diagnosis -- but a very convincing feature if seen.
- Papillae may be seen in Graves disease.
- Thyroid tissue lateral to the jugular vein (often referred to as lateral aberrant thyroid tissue) is generally considered metastatic thyroid carcinoma (papillary thyroid carcinoma) even if it looks benign.[6]
- This dictum is disputed.[7]
- The level VI and VII lymph nodes are medial to the jugular.
DDx:
Subtypes of papillary thyroid carcinoma
There are many.
Poor prognosis variants:
Papillary thyroid carcinoma tall cell variant
General
- ~10% of PTC.[11]
- Often large > 6 cm.
Microscopic
Features:[12]
- 50% of cells with height 2x the width.[13]
- Eosinophilic cytoplasm.
- Well-defined cell borders.
- Nucleus stratified; basal location, i.e. closer to the basement membrane.
Negative:
- Nuclei not pseudostratified, if pseudostratified consider columnar cell variant.
Images:
Papillary thyroid carcinoma columnar cell variant
General
Epidemiology:
- Poor prognosis.
- Very rare.
Microscopic
Features:[15]
- Elongated nuclei (similar to colorectal adenocarcinoma) - key feature.
- +/-Pseudostratification of the nuclei (like in colorectal adenocarcinoma), differentiates from tall cell variant.
- Nuclear stratification - key feature.
- "Minimal" papillary features.
- "Tall cells".
- Clear-eosinophilic cytoplasm.
- Mitoses common.
Image: Columnar variant PTC (wiley.com).
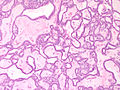
Papillary thyroid carcinoma follicular variant
General
- May be confused with follicular carcinoma or follicular adenoma.
- Pathologists often disagree about this diagnosis.[16]
Microscopic
Features:[17]
- Small tightly packed follicles - key feature.
- Hypereosinophilic colloid.
- Nuclear features of PTC.
- Large nuclei.
- Typically have less nuclear pseudoinclusions than the conventional type.
- +/-Fibrous capsule (common).
DDx:
- Noninvasive follicular thyroid neoplasm with papillary-like nuclear features (NIFTP).
- Follicular thyroid carcinoma - has a fibrous capsule and invasion though it.
- Follicular thyroid adenoma - surrounded by a fibrous capsule.
- Adenomatoid nodule - round nuclei, no nuclear features of PTC.
Images:
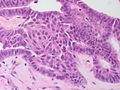
Papillary thyroid carcinoma cribriform-morular variant
General
- Associated with familial adenomatous polyposis (FAP).[18]
Microscopic
Features:
- Circumscribed or even encapsulated neoplasm.
- Morules - interspersed balls of squamoid cells
- No keritinization or intercellular bridges.
- Homogenous, lightly eosinophilic glassy nuclei (biotin accumulation).
- Follicles
- Cribriform, papillary, trabecular and solid patterns.
- Columnar or cuboidal cells.
- Little colloid
- Papillary carcinoma nuclear features.
DDX:
- Papillary thyroid carcinoma
- Papillary thyroid carcinoma, tall cell variant
IHC
- CDX2 - Highlights the morules (CDX2 is positive in the biotin rich nuclei associated with morule formation in a variety of situations)[19]
- CD10 - Highlights the morules [20]
- Beta-catenin - nuclear and cytoplasmic - all tumour cells.
- Estrogen receptor - positive
- TTF-1 - positive
Molecular
- Up-regulating disturbances in the Wnt signaling pathway promote formation of morules with optically clear biotin rich nuclei [21]
- Mutation of the beta-catenin gene
- Mutation in APC
- Examples
- Well-differentiated fetal adenocarcinoma
- Papillary thyroid carcinoma, cribriform morular variant (mutation in APC in familial variants)
- Pancreatoblastoma
Papillary thyroid carcinoma diffuse sclerosing variant
General
- Usually young adults, children.
Microscopic
Features:[22]
- Papillae - usu. prominent.
- Squamous morules - key features.[23]
- Lymphocytes - abundant.
- Fibrosis.
DDx:
- Lymphocytic thyroiditis (esp. Hashimoto's thyroiditis).
Papillary thyroid carcinoma Warthin-like variant
- Resembles Warthin tumour.
Microscopic
Features:[15]
- Eosinophilic cytoplasm.
- Lymphocytic thyroiditis.
- Papillae.
Papillary thyroid carcinoma solid variant
Features:[9]
- Some studies suggest this has a poor prognosis.
- More common in children.
- Associated with Chernobyl nuclear accident.
Microscopic
Features:
- Solid sheets >50% of tumour mass.[9]
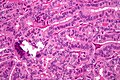
Papillary thyroid carcinoma oncocytic variant
Features:
- Possible association with autoimmune thyroiditis.[24]
Microscopic
Features:[24]
- Abundant oncocytic tumour cells with apical nuclei.
- Classic features of PTC:
- Grooves and and abundant pseudoinclusions.[25]
- >70% papillary architecture.[25]
- +/-Degenerative changes.
Note:
- CK19 +ve -- though not specific or sensitive.
IHC
Thyroid versus something else:
- Thyroglobulin +ve.[26]
- TTF-1 (thyroid transcription factor-1) +ve.
- CD15 +ve.[citation needed]
PTC versus benign:[27]
- HBME-1 +ve (strong, diffuse).
- CK19 +ve (strong, diffuse).
- Galectin-3 +ve (strong, diffuse).
Molecular
- BRAF mutation.[28]
Tabular summary
Molecular changes in papillary thyroid carcinoma as per Adeniran et al:[29]
| Molecular change | Frequency | Histology | Notes |
|---|---|---|---|
| BRAF point mutations | ~ 40% | tall cell variant | poorer prognosis, older individuals |
| RET/PTC rearrangments | ~ 20% | papillary architecture, psammoma bodies | younger individuals |
| RAS point mutations | ~ 15% | exclusively follicular variant | - |
Sign out
HEMITHYROID, RIGHT, COMPLETION OF TOTAL THYROIDECTOMY: - PAPILLARY THYROID CARCINOMA, FOLLICULAR VARIANT. -- TUMOUR SIZE: 4 MM (MAXIMAL). -- ARCHITECTURE: FOLLICULAR. -- CYTOMORPHOLOGY: CLASSICAL. -- HISTOLOGIC GRADE: G1 (WELL DIFFERENTIATED). -- NO TUMOUR CAPSULE IDENTIFIED. -- NEGATIVE FOR LYMPHOVASCULAR INVASION. -- NEGATIVE FOR PERINEURAL INVASION. -- NEGATIVE FOR EXTRATHYROIDAL EXTENSION. -- SURGICAL MARGINS NEGATIVE FOR MALIGNANCY.
Note:
- If it is a completion thyroidectomy and the staging changes one should do a full synoptic report.
Microcarcinoma
A. LEFT HEMITHYROID, THYROIDECTOMY COMPLETION: - PAPILLARY THYROID MICROCARCINOMA. -- MARGINS NEGATIVE FOR MALIGNANCY. -- TUMOUR SIZE ~ 1 MILLIMETRE. -- NEGATIVE FOR LYMPHOVASCULAR INVASION. -- NEGATIVE FOR PERINEURAL INVASION. - PALPATION THYROIDITIS, FOCAL. - NODULAR HYPERPLASIA. B. LYMPH NODES, LEVEL 6 AND 7, LYMPH NODE DISSECTION: - TWO LYMPH NODES, NEGATIVE FOR MALIGNANCY ( 0 POSITIVE / 2 ).
THYROID GLAND, TOTAL THYROIDECTOMY: - INCIDENTAL PAPILLARY THYROID MICROCARCINOMA. -- MARGINS NEGATIVE FOR MALIGNANCY. -- TUMOUR SIZE ~ 1 MILLIMETRE. -- NEGATIVE FOR LYMPHOVASCULAR INVASION. -- NEGATIVE FOR PERINEURAL INVASION. - NODULAR HYPERPLASIA. - ONE PARATHYROID GLAND.
Lymph node dissection
A. NECK, RIGHT LEVEL 2 AND 3, LYMPH NODE DISSECTION: - ONE LYMPH NODE POSITIVE FOR PAPILLARY THYROID CARCINOMA ( 1 POSITIVE / 4 ). B. NECK, RIGHT LEVEL 4, LYMPH NODE DISSECTION: - TWO LYMPH NODES, NEGATIVE FOR MALIGNANCY ( 0 POSITIVE / 2 ). C. NECK, RIGHT LEVEL 6 AND 7, LYMPH NODE DISSECTION: - ONE LYMPH NODE POSITIVE FOR PAPILLARY THYROID CARCINOMA ( 1 POSITIVE / 3 ).
Micro
The sections show lymph nodes with tumour that has a papillary architecture. The tumour cell nuclei are enlarged and overlap. They also have nuclear grooves, nucleoli and abundant pseudoinclusions. The chromatin of the tumour cells has a powdery appearance.
See also
References
- ↑ Mills, Stacey E; Carter, Darryl; Greenson, Joel K; Oberman, Harold A; Reuter, Victor E (2004). Sternberg's Diagnostic Surgical Pathology (4th ed.). Lippincott Williams & Wilkins. pp. 564. ISBN 978-0781740517.
- ↑ Sethom, A.; Riahi, I.; Riahi, K.; Akkari, K.; Benzarti, S.; Miled, I.; Chebbi, MK. (Jan 2011). "[Management of thyroid microcarcinoma. Report of 13 cases].". Tunis Med 89 (1): 23-5. PMID 21267823.
- ↑ Hay, ID.; Thompson, GB.; Grant, CS.; Bergstralh, EJ.; Dvorak, CE.; Gorman, CA.; Maurer, MS.; McIver, B. et al. (Aug 2002). "Papillary thyroid carcinoma managed at the Mayo Clinic during six decades (1940-1999): temporal trends in initial therapy and long-term outcome in 2444 consecutively treated patients.". World J Surg 26 (8): 879-85. doi:10.1007/s00268-002-6612-1. PMID 12016468.
- ↑ Mills, Stacey E; Carter, Darryl; Greenson, Joel K; Oberman, Harold A; Reuter, Victor E (2004). Sternberg's Diagnostic Surgical Pathology (4th ed.). Lippincott Williams & Wilkins. pp. 565. ISBN 978-0781740517.
- ↑ Mills, Stacey E; Carter, Darryl; Greenson, Joel K; Oberman, Harold A; Reuter, Victor E (2004). Sternberg's Diagnostic Surgical Pathology (4th ed.). Lippincott Williams & Wilkins. pp. 566. ISBN 978-0781740517.
- ↑ JOHNSON, RW.; SAHA, NC. (Jun 1962). "The so-called lateral aberrant thyroid.". Br Med J 1 (5293): 1668-9. PMC 1958877. PMID 14452106. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1958877/.
- ↑ Escofet, X.; Khan, AZ.; Mazarani, W.; Woods, WG. (Jan 2007). "Lessons to be learned: a case study approach. Lateral aberrant thyroid tissue: is it always malignant?". J R Soc Promot Health 127 (1): 45-6. PMID 17319317.
- ↑ Baloch, ZW.; LiVolsi, VA. (Jun 2006). "Cytologic and architectural mimics of papillary thyroid carcinoma. Diagnostic challenges in fine-needle aspiration and surgical pathology specimens.". Am J Clin Pathol 125 Suppl: S135-44. PMID 16830963.
- ↑ 9.0 9.1 9.2 9.3 9.4 Gonzalez-Gonzalez, R.; Bologna-Molina, R.; Carreon-Burciaga, RG.; Gómezpalacio-Gastelum, M.; Molina-Frechero, N.; Salazar-Rodríguez, S. (2011). "Papillary thyroid carcinoma: differential diagnosis and prognostic values of its different variants: review of the literature.". ISRN Oncol 2011: 915925. doi:10.5402/2011/915925. PMC 3302055. PMID 22432054. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3302055/.
- ↑ URL: http://emedicine.medscape.com/article/849000-overview#a0104. Accessed on: 1 May 2012.
- ↑ Mills, Stacey E; Carter, Darryl; Greenson, Joel K; Reuter, Victor E; Stoler, Mark H (2009). Sternberg's Diagnostic Surgical Pathology (5th ed.). Lippincott Williams & Wilkins. pp. 505. ISBN 978-0781779425.
- ↑ Urano M, Kiriyama Y, Takakuwa Y, Kuroda M (April 2009). "Tall cell variant of papillary thyroid carcinoma: Its characteristic features demonstrated by fine-needle aspiration cytology and immunohistochemical study". Diagn. Cytopathol.. doi:10.1002/dc.21086. PMID 19373912.
- ↑ 13.0 13.1 Ghossein R, Livolsi VA (November 2008). "Papillary thyroid carcinoma tall cell variant". Thyroid 18 (11): 1179–81. doi:10.1089/thy.2008.0164. PMID 18925842.
- ↑ S. Raphael. 17 January 2011.
- ↑ 15.0 15.1 Mills, Stacey E; Carter, Darryl; Greenson, Joel K; Reuter, Victor E; Stoler, Mark H (2009). Sternberg's Diagnostic Surgical Pathology (5th ed.). Lippincott Williams & Wilkins. pp. 506. ISBN 978-0781779425.
- ↑ Daniels, GH.. "What if many follicular variant papillary thyroid carcinomas are not malignant? A review of follicular variant papillary thyroid carcinoma and a proposal for a new classification.". Endocr Pract 17 (5): 768-87. doi:10.4158/EP10407.RA. PMID 21940284.
- ↑ Thompson, Lester D. R. (2006). Endocrine Pathology: A Volume in Foundations in Diagnostic Pathology Series (1st ed.). Churchill Livingstone. pp. 88. ISBN 978-0443066856.
- ↑ Groen EJ, Roos A, Muntinghe FL, et al. (September 2008). "Extra-intestinal manifestations of familial adenomatous polyposis". Ann. Surg. Oncol. 15 (9): 2439–50. doi:10.1245/s10434-008-9981-3. PMC 2518080. PMID 18612695. http://www.ncbi.nlm.nih.gov/pmc/articles/PMC2518080/?tool=pubmed.
- ↑ Wani, Y.; Notohara, K.; Nakatani, Y.; Matsuzaki, A. (Oct 2009). "Aberrant nuclear Cdx2 expression in morule-forming tumours in different organs, accompanied by cytoplasmic reactivity.". Histopathology 55 (4): 465-8. doi:10.1111/j.1365-2559.2009.03382.x. PMID 19817898.
- ↑ Cameselle-Teijeiro, J.; Alberte-Lista, L.; Chiarelli, S.; Buriticá, C.; Gonçalves, L.; González-Cámpora, R.; Nogales, FF. (Feb 2008). "CD10 is a characteristic marker of tumours forming morules with biotin-rich, optically clear nuclei that occur in different organs.". Histopathology 52 (3): 389-92. doi:10.1111/j.1365-2559.2007.02911.x. PMID 18081818.
- ↑ Gamachi, A.; Kashima, K.; Daa, T.; Nakatani, Y.; Tsujimoto, M.; Yokoyama, S. (Nov 2003). "Aberrant intranuclear localization of biotin, biotin-binding enzymes, and beta-catenin in pregnancy-related endometrium and morule-associated neoplastic lesions.". Mod Pathol 16 (11): 1124-31. doi:10.1097/01.MP.0000092953.20717.48. PMID 14614052.
- ↑ Kumar, Vinay; Abbas, Abul K.; Fausto, Nelson; Aster, Jon (2009). Robbins and Cotran pathologic basis of disease (8th ed.). Elsevier Saunders. pp. 1122. ISBN 978-1416031215.
- ↑ Hirokawa, M.; Kuma, S.; Miyauchi, A.; Qian, ZR.; Nakasono, M.; Sano, T.; Kakudo, K.. "Morules in cribriform-morular variant of papillary thyroid carcinoma: Immunohistochemical characteristics and distinction from squamous metaplasia.". APMIS 112 (4-5): 275-82. doi:10.1111/j.1600-0463.2004.apm11204-0508.x. PMID 15233643.
- ↑ 24.0 24.1 Berho, M.; Suster, S. (Jan 1997). "The oncocytic variant of papillary carcinoma of the thyroid: a clinicopathologic study of 15 cases.". Hum Pathol 28 (1): 47-53. PMID 9013831.
- ↑ 25.0 25.1 Thompson, Lester D. R. (2006). Endocrine Pathology: A Volume in Foundations in Diagnostic Pathology Series (1st ed.). Churchill Livingstone. pp. 86. ISBN 978-0443066856.
- ↑ Sathiyamoorthy, S.; Maleki, Z. (Jan 2014). "Cytomorphologic overlap of differentiated thyroid carcinoma and lung adenocarcinoma and diagnostic value of TTF-1 and TGB on cytologic material.". Diagn Cytopathol 42 (1): 5-10. doi:10.1002/dc.22997. PMID 23637102.
- ↑ Mataraci, EA.; Ozgüven, BY.; Kabukçuoglu, F. (Mar 2012). "Expression of cytokeratin 19, HBME-1 and galectin-3 in neoplastic and nonneoplastic thyroid lesions.". Pol J Pathol 63 (1): 58-64. PMID 22535608.
- ↑ Lam AK (2022). "Papillary Thyroid Carcinoma: Current Position in Epidemiology, Genomics, and Classification". Methods Mol Biol 2534: 1–15. doi:10.1007/978-1-0716-2505-7_1. PMID 35670964.
- ↑ Adeniran, AJ.; Zhu, Z.; Gandhi, M.; Steward, DL.; Fidler, JP.; Giordano, TJ.; Biddinger, PW.; Nikiforov, YE. (Feb 2006). "Correlation between genetic alterations and microscopic features, clinical manifestations, and prognostic characteristics of thyroid papillary carcinomas.". Am J Surg Pathol 30 (2): 216-22. PMID 16434896.