Difference between revisions of "Seminoma"
Jump to navigation
Jump to search
(→Images) |
|||
| (20 intermediate revisions by the same user not shown) | |||
| Line 6: | Line 6: | ||
| Micro = fried egg-like cells (clear or eosinophilic cytoplasm, central nucleus), lymphocytic infiltrate (common), +/-[[syncytiotrophoblast]]s (rare), +/-granulomas (uncommon) | | Micro = fried egg-like cells (clear or eosinophilic cytoplasm, central nucleus), lymphocytic infiltrate (common), +/-[[syncytiotrophoblast]]s (rare), +/-granulomas (uncommon) | ||
| Subtypes = | | Subtypes = | ||
| LMDDx = [[embryonal carcinoma]], [[ | | LMDDx = [[embryonal carcinoma]], [[GCNIS]], [[mixed germ cell tumour]], [[granulomatous orchitis]], [[testicular scar]], [[atrophic testis]] | ||
| Stains = | | Stains = | ||
| IHC = | | IHC = OCT4 +ve, [[CD117]] +ve, CD30 -ve | ||
| EM = | | EM = | ||
| Molecular = | | Molecular = | ||
| IF = | | IF = | ||
| Gross = solid, white/tan | | Gross = solid, white/tan | ||
| Grossing = [[ | | Grossing = [[orchiectomy grossing]] | ||
| Staging = [[testicular cancer staging]] | |||
| Site = [[testis]] | | Site = [[testis]] | ||
| Assdx = [[ | | Assdx = [[GCNIS]] | ||
| Syndromes = | | Syndromes = | ||
| Clinicalhx = | | Clinicalhx = | ||
| Line 21: | Line 22: | ||
| Symptoms = | | Symptoms = | ||
| Prevalence = | | Prevalence = | ||
| Bloodwork = LDH elevated, beta-hCG elevated | | Bloodwork = LDH elevated, beta-hCG normal or slightly elevated | ||
| Rads = | | Rads = | ||
| Endoscopy = | | Endoscopy = | ||
| Line 27: | Line 28: | ||
| Other = | | Other = | ||
| ClinDDx = other [[testis|testicular tumours]] ([[germ cell tumour]]s, [[lymphoma]]) | | ClinDDx = other [[testis|testicular tumours]] ([[germ cell tumour]]s, [[lymphoma]]) | ||
| Tx = | |||
}} | }} | ||
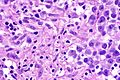
'''Seminoma''' is a common [[testis|testicular]] [[germ cell tumour]]. | '''Seminoma''' is a common [[testis|testicular]] [[germ cell tumour]]. | ||
It should ''not'' be confused with | It should ''not'' be confused with ''[[spermatocytic tumour]]'' (previously known as ''spermatocytic seminoma''). | ||
==General== | ==General== | ||
| Line 39: | Line 41: | ||
*Elevated serum LDH. | *Elevated serum LDH. | ||
*Normal serum alpha fetoprotein. | *Normal serum alpha fetoprotein. | ||
*Usually normal beta-hCG. | *Usually normal beta-hCG ''or'' slightly elevated.<ref name=pmid9311009>{{cite journal |authors=Hori K, Uematsu K, Yasoshima H, Yamada A, Sakurai K, Ohya M |title=Testicular seminoma with human chorionic gonadotropin production |journal=Pathol Int |volume=47 |issue=9 |pages=592–9 |date=September 1997 |pmid=9311009 |doi=10.1111/j.1440-1827.1997.tb04547.x |url=}}</ref> | ||
Note: | Note: | ||
| Line 45: | Line 47: | ||
===Epidemiology & etiology=== | ===Epidemiology & etiology=== | ||
*Arises from ''[[ | *Arises from ''[[germ cell neoplasia in situ]]'', abbreviated ''GCNIS'' (previously known as ''intratubular germ cell neoplasia''). | ||
==Gross== | ==Gross== | ||
| Line 61: | Line 63: | ||
*+/-Lymphoctyes - interspersed (very common). | *+/-Lymphoctyes - interspersed (very common). | ||
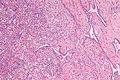
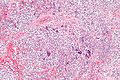
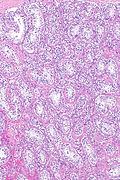
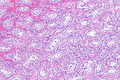
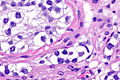
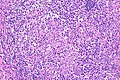
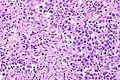
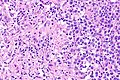
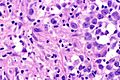
*+/-[[Syncytiotrophoblast]]s, [[AKA]] ''syncytiotrophoblastic giant cells'' (STGCs),<ref name=Ref_GUP542>{{Ref GUP|542}}</ref> present in ~10-20% of seminoma.<ref>URL: [http://www.webpathology.com/image.asp?case=31&n=10 http://www.webpathology.com/image.asp?case=31&n=10]. Accessed on: 22 May 2012.</ref> | *+/-[[Syncytiotrophoblast]]s, [[AKA]] ''syncytiotrophoblastic giant cells'' (STGCs),<ref name=Ref_GUP542>{{Ref GUP|542}}</ref> present in ~10-20% of seminoma.<ref>URL: [http://www.webpathology.com/image.asp?case=31&n=10 http://www.webpathology.com/image.asp?case=31&n=10]. Accessed on: 22 May 2012.</ref> | ||
**Large + irregular, vesicular nuclei. | **Large + irregular, [[vesicular nuclei]]. | ||
**Eosinophilic vacuolated cytoplasm (contains hCG). | **Eosinophilic vacuolated cytoplasm (contains hCG). | ||
***Syncytiotrophoblasts = closest to mom in normal [[chorionic villi]] - covers cytotrophoblast.<ref>URL: [http://upload.wikimedia.org/wikipedia/commons/4/45/Gray37.png http://upload.wikimedia.org/wikipedia/commons/4/45/Gray37.png]. Accessed on: 31 May 2010.</ref> | ***Syncytiotrophoblasts = closest to mom in normal [[chorionic villi]] - covers cytotrophoblast.<ref>URL: [http://upload.wikimedia.org/wikipedia/commons/4/45/Gray37.png http://upload.wikimedia.org/wikipedia/commons/4/45/Gray37.png]. Accessed on: 31 May 2010.</ref> | ||
| Line 70: | Line 72: | ||
*Approximately 24% of Stage I seminomas have [[lymphovascular invasion]].<ref name=pmid23275274>{{Cite journal | last1 = Soper | first1 = MS. | last2 = Hastings | first2 = JR. | last3 = Cosmatos | first3 = HA. | last4 = Slezak | first4 = JM. | last5 = Wang | first5 = R. | last6 = Lodin | first6 = K. | title = Observation versus adjuvant radiation or chemotherapy in the management of stage I seminoma: clinical outcomes and prognostic factors for relapse in a large US cohort. | journal = Am J Clin Oncol | volume = 37 | issue = 4 | pages = 356-9 | month = Aug | year = 2014 | doi = 10.1097/COC.0b013e318277d839 | PMID = 23275274 }}</ref> | *Approximately 24% of Stage I seminomas have [[lymphovascular invasion]].<ref name=pmid23275274>{{Cite journal | last1 = Soper | first1 = MS. | last2 = Hastings | first2 = JR. | last3 = Cosmatos | first3 = HA. | last4 = Slezak | first4 = JM. | last5 = Wang | first5 = R. | last6 = Lodin | first6 = K. | title = Observation versus adjuvant radiation or chemotherapy in the management of stage I seminoma: clinical outcomes and prognostic factors for relapse in a large US cohort. | journal = Am J Clin Oncol | volume = 37 | issue = 4 | pages = 356-9 | month = Aug | year = 2014 | doi = 10.1097/COC.0b013e318277d839 | PMID = 23275274 }}</ref> | ||
**Stage I = Tx N0 M0.<ref>URL: [http://emedicine.medscape.com/article/2006777-overview http://emedicine.medscape.com/article/2006777-overview]. Accessed on: October 8, 2014.</ref> | **Stage I = Tx N0 M0.<ref>URL: [http://emedicine.medscape.com/article/2006777-overview http://emedicine.medscape.com/article/2006777-overview]. Accessed on: October 8, 2014.</ref> | ||
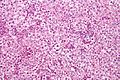
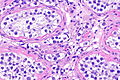
*Intertubular seminoma may ''not'' form a discrete mass and mimic a benign testis.<ref name=pmid15316315>{{Cite journal | last1 = Henley | first1 = JD. | last2 = Young | first2 = RH. | last3 = Wade | first3 = CL. | last4 = Ulbright | first4 = TM. | title = Seminomas with exclusive intertubular growth: a report of 12 clinically and grossly inconspicuous tumors. | journal = Am J Surg Pathol | volume = 28 | issue = 9 | pages = 1163-8 | month = Sep | year = 2004 | doi = | PMID = 15316315 }}</ref> | |||
DDx: | DDx: | ||
| Line 77: | Line 80: | ||
*[[Mixed germ cell tumour]]. | *[[Mixed germ cell tumour]]. | ||
*[[Choriocarcinoma]] - esp. if (multinucleated) syncytiotrophoblasts are present.<ref name=pmid157614>{{Cite journal | last1 = Hedinger | first1 = C. | last2 = von Hochstetter | first2 = AR. | last3 = Egloff | first3 = B. | title = Seminoma with syncytiotrophoblastic giant cells. A special form of seminoma. | journal = Virchows Arch A Pathol Anat Histol | volume = 383 | issue = 1 | pages = 59-67 | month = Jul | year = 1979 | doi = | PMID = 157614 }}</ref> | *[[Choriocarcinoma]] - esp. if (multinucleated) syncytiotrophoblasts are present.<ref name=pmid157614>{{Cite journal | last1 = Hedinger | first1 = C. | last2 = von Hochstetter | first2 = AR. | last3 = Egloff | first3 = B. | title = Seminoma with syncytiotrophoblastic giant cells. A special form of seminoma. | journal = Virchows Arch A Pathol Anat Histol | volume = 383 | issue = 1 | pages = 59-67 | month = Jul | year = 1979 | doi = | PMID = 157614 }}</ref> | ||
*Granulomatous orchitis - if [[granuloma]]s are present. | *[[Granulomatous orchitis]] - if [[granuloma]]s are present. | ||
*[[Testicular scar]] - seminomas may regress spontaneously. | *[[Testicular scar]] - seminomas may regress spontaneously. | ||
*[[Testicular atrophy]] - esp. for intertubular predominant seminoma.<ref name=pmid15316315>{{Cite journal | last1 = Henley | first1 = JD. | last2 = Young | first2 = RH. | last3 = Wade | first3 = CL. | last4 = Ulbright | first4 = TM. | title = Seminomas with exclusive intertubular growth: a report of 12 clinically and grossly inconspicuous tumors. | journal = Am J Surg Pathol | volume = 28 | issue = 9 | pages = 1163-8 | month = Sep | year = 2004 | doi = | PMID = 15316315 }}</ref> | |||
===Images=== | ===Images=== | ||
| Line 85: | Line 89: | ||
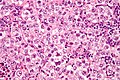
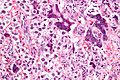
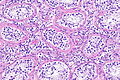
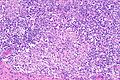
Image:Seminoma_intermed_mag.jpg |Seminoma - intermed. mag. (WC/Nephron) | Image:Seminoma_intermed_mag.jpg |Seminoma - intermed. mag. (WC/Nephron) | ||
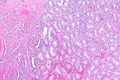
Image:Rete_testis_with_seminoma.jpg |Seminoma in the rete testis. (WC/Nephron) | Image:Rete_testis_with_seminoma.jpg |Seminoma in the rete testis. (WC/Nephron) | ||
</gallery> | |||
====Syncytiotrophoblasts==== | |||
<gallery> | |||
Image:Seminoma_with_syncytiotrophoblasts_-_intermed_mag.jpg |Seminoma with syncytiotrophoblasts - intermed. mag. (WC/Nephron) | Image:Seminoma_with_syncytiotrophoblasts_-_intermed_mag.jpg |Seminoma with syncytiotrophoblasts - intermed. mag. (WC/Nephron) | ||
Image:Seminoma_with_syncytiotrophoblasts_-_very_high_mag.jpg |Seminoma with syncytiotrophoblasts - very high mag. (WC/Nephron) | Image:Seminoma_with_syncytiotrophoblasts_-_very_high_mag.jpg |Seminoma with syncytiotrophoblasts - very high mag. (WC/Nephron) | ||
</gallery> | </gallery> | ||
====Intertubular seminoma==== | |||
<gallery> | |||
Image: Intertubular seminoma -- very low mag.jpg | ITS - very low mag. (WC) | |||
Image: Intertubular seminoma -- low mag.jpg | ITS - low mag. (WC) | |||
Image: Intertubular seminoma - alt -- low mag.jpg | ITS - low mag. (WC) | |||
Image: Intertubular seminoma -- intermed mag.jpg | ITS - intermed. mag. (WC) | |||
Image: Intertubular seminoma -- high mag.jpg | ITS - high mag. (WC) | |||
Image: Intertubular seminoma -- very high mag.jpg | ITS - very high mag. (WC) | |||
</gallery> | |||
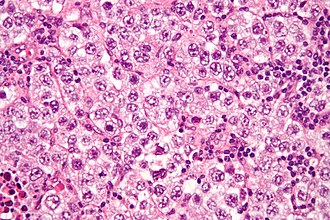
====Lymph node metastasis==== | |||
<gallery> | <gallery> | ||
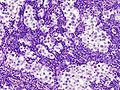
Image: Testicular seminoma (1) nodal metastasis.jpg | Seminoma in LN. (WC/KGH) | Image: Testicular seminoma (1) nodal metastasis.jpg | Seminoma in LN. (WC/KGH) | ||
Image: Testicular seminoma (2) nodal metastasis.jpg | Seminoma in LN. (WC/KGH) | Image: Testicular seminoma (2) nodal metastasis.jpg | Seminoma in LN. (WC/KGH) | ||
</gallery> | |||
====Seminoma with granulomas==== | |||
<gallery> | |||
Image: Seminoma with granulomas -- intermed mag.jpg | Seminoma with granulomas - intermed. mag. | |||
Image: Seminoma with granulomas -- high mag.jpg | Seminoma with granulomas - high mag. | |||
Image: Seminoma with granulomas -- very high mag.jpg | Seminoma with granulomas - very high mag. | |||
Image: Seminoma with granulomas --- low mag.jpg | Seminoma with granulomas - low mag. | |||
Image: Seminoma with granulomas --- intermed mag.jpg | Seminoma with granulomas - intermed. mag. | |||
Image: Seminoma with granulomas --- high mag.jpg | Seminoma with granulomas - high mag. | |||
Image: Seminoma with granulomas --- very high mag.jpg | Seminoma with granulomas - very high mag. | |||
</gallery> | </gallery> | ||
| Line 97: | Line 125: | ||
A general panel:<ref name=pmid24832161>{{cite journal |author=Ulbright TM, Tickoo SK, Berney DM, Srigley JR |title=Best practices recommendations in the application of immunohistochemistry in testicular tumors: report from the international society of urological pathology consensus conference |journal=Am. J. Surg. Pathol. |volume=38 |issue=8 |pages=e50–9 |year=2014 |month=August |pmid=24832161 |doi=10.1097/PAS.0000000000000233 |url=}}</ref> | A general panel:<ref name=pmid24832161>{{cite journal |author=Ulbright TM, Tickoo SK, Berney DM, Srigley JR |title=Best practices recommendations in the application of immunohistochemistry in testicular tumors: report from the international society of urological pathology consensus conference |journal=Am. J. Surg. Pathol. |volume=38 |issue=8 |pages=e50–9 |year=2014 |month=August |pmid=24832161 |doi=10.1097/PAS.0000000000000233 |url=}}</ref> | ||
*OCT4 +ve. | *OCT4 +ve. | ||
**Choriocarcinoma, yolk sac tumour and spermatocytic | **Choriocarcinoma, yolk sac tumour and [[spermatocytic tumour]] all -ve. | ||
*CD117 +ve. | *CD117 +ve. | ||
**-ve in embryonal carcinoma. | **-ve in embryonal carcinoma. | ||
| Line 116: | Line 144: | ||
*OCT3/4 +ve.<ref name=pmid20438407>{{Cite journal | last1 = Emerson | first1 = RE. | last2 = Ulbright | first2 = TM. | title = Intratubular germ cell neoplasia of the testis and its associated cancers: the use of novel biomarkers. | journal = Pathology | volume = 42 | issue = 4 | pages = 344-55 | month = Jun | year = 2010 | doi = 10.3109/00313021003767355 | PMID = 20438407 }}</ref> | *OCT3/4 +ve.<ref name=pmid20438407>{{Cite journal | last1 = Emerson | first1 = RE. | last2 = Ulbright | first2 = TM. | title = Intratubular germ cell neoplasia of the testis and its associated cancers: the use of novel biomarkers. | journal = Pathology | volume = 42 | issue = 4 | pages = 344-55 | month = Jun | year = 2010 | doi = 10.3109/00313021003767355 | PMID = 20438407 }}</ref> | ||
**Also +ve in embryonal carcinoma.<ref name=pmid18045648>{{Cite journal | last1 = Iczkowski | first1 = KA. | last2 = Butler | first2 = SL. | last3 = Shanks | first3 = JH. | last4 = Hossain | first4 = D. | last5 = Schall | first5 = A. | last6 = Meiers | first6 = I. | last7 = Zhou | first7 = M. | last8 = Torkko | first8 = KC. | last9 = Kim | first9 = SJ. | title = Trials of new germ cell immunohistochemical stains in 93 extragonadal and metastatic germ cell tumors. | journal = Hum Pathol | volume = 39 | issue = 2 | pages = 275-81 | month = Feb | year = 2008 | doi = 10.1016/j.humpath.2007.07.002 | PMID = 18045648 }}</ref> | **Also +ve in embryonal carcinoma.<ref name=pmid18045648>{{Cite journal | last1 = Iczkowski | first1 = KA. | last2 = Butler | first2 = SL. | last3 = Shanks | first3 = JH. | last4 = Hossain | first4 = D. | last5 = Schall | first5 = A. | last6 = Meiers | first6 = I. | last7 = Zhou | first7 = M. | last8 = Torkko | first8 = KC. | last9 = Kim | first9 = SJ. | title = Trials of new germ cell immunohistochemical stains in 93 extragonadal and metastatic germ cell tumors. | journal = Hum Pathol | volume = 39 | issue = 2 | pages = 275-81 | month = Feb | year = 2008 | doi = 10.1016/j.humpath.2007.07.002 | PMID = 18045648 }}</ref> | ||
*[[PLAP]] +ve. | |||
**Largely replaced by ''OCT4'' or ''OCT3/4'' - which is more sensitive.<ref name=pmid15725806 >{{Cite journal | last1 = Hattab | first1 = EM. | last2 = Tu | first2 = PH. | last3 = Wilson | first3 = JD. | last4 = Cheng | first4 = L. | title = OCT4 immunohistochemistry is superior to placental alkaline phosphatase (PLAP) in the diagnosis of central nervous system germinoma. | journal = Am J Surg Pathol | volume = 29 | issue = 3 | pages = 368-71 | month = Mar | year = 2005 | doi = | PMID = 15725806 }}</ref> | |||
==Sign out== | ==Sign out== | ||
<pre> | |||
Right Testicle, Radical Orchitectomy: | |||
- SEMINOMA (pure). | |||
-- Margins clear. | |||
-- Germ cell neoplasia in situ (intratubular germ cell neoplasia) present. | |||
-- Please see synoptic report. | |||
- Background testis consists of Sertoli cells only, NEGATIVE for spermatogenesis. | |||
</pre> | |||
<pre> | |||
Testis, Left, Radical Orchiectomy: | |||
- SEMINOMA (pure). | |||
-- Margins clear. | |||
-- Please see synoptic report. | |||
</pre> | |||
===Biopsy=== | |||
<pre> | <pre> | ||
RETROPERITONEAL SOFT TISSUE, RIGHT, CORE BIOPSY: | RETROPERITONEAL SOFT TISSUE, RIGHT, CORE BIOPSY: | ||
- SEMINOMA. | - SEMINOMA. | ||
</pre> | </pre> | ||
===Micro=== | |||
====Micro==== | |||
The sections show large atypical, discohesive cells with prominent nucleoli, central | The sections show large atypical, discohesive cells with prominent nucleoli, central | ||
nuclei and moderate clear cytoplasm, intermixed with mature lymphocytes. Mitotic | nuclei and moderate clear cytoplasm, intermixed with mature lymphocytes. Mitotic | ||
activity is present. | activity is present. | ||
===Small biopsy=== | ====Small biopsy==== | ||
A mixed germ cell tumour cannot be excluded; given the small quantity of tumour, this | A mixed germ cell tumour cannot be excluded; given the small quantity of tumour, this | ||
biopsy is at a high risk for having undersampled other tumour components should they be | biopsy is at a high risk for having undersampled other tumour components should they be | ||
Latest revision as of 19:24, 12 April 2022
| Seminoma | |
|---|---|
| Diagnosis in short | |
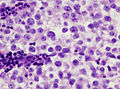
 Seminoma. H&E stain. | |
|
| |
| LM | fried egg-like cells (clear or eosinophilic cytoplasm, central nucleus), lymphocytic infiltrate (common), +/-syncytiotrophoblasts (rare), +/-granulomas (uncommon) |
| LM DDx | embryonal carcinoma, GCNIS, mixed germ cell tumour, granulomatous orchitis, testicular scar, atrophic testis |
| IHC | OCT4 +ve, CD117 +ve, CD30 -ve |
| Gross | solid, white/tan |
| Grossing notes | orchiectomy grossing |
| Staging | testicular cancer staging |
| Site | testis |
|
| |
| Associated Dx | GCNIS |
| Signs | testicular mass, +/-retroperitoneal lymphadenopathy |
| Blood work | LDH elevated, beta-hCG normal or slightly elevated |
| Prognosis | good |
| Clin. DDx | other testicular tumours (germ cell tumours, lymphoma) |
Seminoma is a common testicular germ cell tumour.
It should not be confused with spermatocytic tumour (previously known as spermatocytic seminoma).
General
- Male counterpart of the dysgerminoma, which arise in the ovary.
- Most common germ cell tumour of the testis.
Clinical:
- Elevated serum LDH.
- Normal serum alpha fetoprotein.
- Usually normal beta-hCG or slightly elevated.[1]
Note:
- Rarely, it may present a retroperitoneal mass.[2]
Epidemiology & etiology
- Arises from germ cell neoplasia in situ, abbreviated GCNIS (previously known as intratubular germ cell neoplasia).
Gross
- Solid, white/tan.
Microsopic
Features:
- Cells with fried egg appearance - key feature:
- Clear cytoplasm.
- Central nucleus, with prominent nucleolus.
- Nucleus may have "corners", i.e. it is not round.
- +/-Lymphoctyes - interspersed (very common).
- +/-Syncytiotrophoblasts, AKA syncytiotrophoblastic giant cells (STGCs),[3] present in ~10-20% of seminoma.[4]
- Large + irregular, vesicular nuclei.
- Eosinophilic vacuolated cytoplasm (contains hCG).
- Syncytiotrophoblasts = closest to mom in normal chorionic villi - covers cytotrophoblast.[5]
- +/-Florid granulomatous reaction.
Notes:
- Memory device: 3 Cs - clear cytoplasm, central nucleus, corners on the nuclear membrane.
- Approximately 24% of Stage I seminomas have lymphovascular invasion.[6]
- Stage I = Tx N0 M0.[7]
- Intertubular seminoma may not form a discrete mass and mimic a benign testis.[8]
DDx:
- Embryonal carcinoma.
- Solid variant of yolk sac tumour.
- Lacks fibrous septae and lymphocytes.[9]
- Mixed germ cell tumour.
- Choriocarcinoma - esp. if (multinucleated) syncytiotrophoblasts are present.[10]
- Granulomatous orchitis - if granulomas are present.
- Testicular scar - seminomas may regress spontaneously.
- Testicular atrophy - esp. for intertubular predominant seminoma.[8]
Images
Syncytiotrophoblasts
Intertubular seminoma
Lymph node metastasis
Seminoma with granulomas
IHC
ISUP consensus
A general panel:[11]
- OCT4 +ve.
- Choriocarcinoma, yolk sac tumour and spermatocytic tumour all -ve.
- CD117 +ve.
- -ve in embryonal carcinoma.
- CD30 -ve.
- +ve in embryonal carcinoma.
Seminoma versus choriocarcinoma:[12]
- OCT4 (uniformily) +ve.
- Choriocarcinoma = patchy staining.
Additional notes
- D2-40 +ve ~100% of cases in one series.[13]
- Useful for discriminating from embryonal carcinoma.[14]
- CD117 +ve (ckit) ~92% of cases.[13]
- CD30 -ve.[15]
- Done to r/o embryonal carcinoma.
- Cytokeratins usu. -ve, may have weak focal positivity.[15]
- OCT3/4 +ve.[16]
- Also +ve in embryonal carcinoma.[14]
- PLAP +ve.
- Largely replaced by OCT4 or OCT3/4 - which is more sensitive.[17]
Sign out
Right Testicle, Radical Orchitectomy:
- SEMINOMA (pure).
-- Margins clear.
-- Germ cell neoplasia in situ (intratubular germ cell neoplasia) present.
-- Please see synoptic report.
- Background testis consists of Sertoli cells only, NEGATIVE for spermatogenesis.
Testis, Left, Radical Orchiectomy:
- SEMINOMA (pure).
-- Margins clear.
-- Please see synoptic report.
Biopsy
RETROPERITONEAL SOFT TISSUE, RIGHT, CORE BIOPSY:
- SEMINOMA.
Micro
The sections show large atypical, discohesive cells with prominent nucleoli, central nuclei and moderate clear cytoplasm, intermixed with mature lymphocytes. Mitotic activity is present.
Small biopsy
A mixed germ cell tumour cannot be excluded; given the small quantity of tumour, this biopsy is at a high risk for having undersampled other tumour components should they be present. Correlation with serology and consideration of re-biopsy is suggested.
See also
References
- ↑ Hori K, Uematsu K, Yasoshima H, Yamada A, Sakurai K, Ohya M (September 1997). "Testicular seminoma with human chorionic gonadotropin production". Pathol Int 47 (9): 592–9. doi:10.1111/j.1440-1827.1997.tb04547.x. PMID 9311009.
- ↑ Preda, O.; Nicolae, A.; Loghin, A.; Borda, A.; Nogales, FF. (2011). "Retroperitoneal seminoma as a first manifestation of a partially regressed (burnt-out) testicular germ cell tumor.". Rom J Morphol Embryol 52 (1): 193-6. PMID 21424055.
- ↑ Zhou, Ming; Magi-Galluzzi, Cristina (2006). Genitourinary Pathology: A Volume in Foundations in Diagnostic Pathology Series (1st ed.). Churchill Livingstone. pp. 542. ISBN 978-0443066771.
- ↑ URL: http://www.webpathology.com/image.asp?case=31&n=10. Accessed on: 22 May 2012.
- ↑ URL: http://upload.wikimedia.org/wikipedia/commons/4/45/Gray37.png. Accessed on: 31 May 2010.
- ↑ Soper, MS.; Hastings, JR.; Cosmatos, HA.; Slezak, JM.; Wang, R.; Lodin, K. (Aug 2014). "Observation versus adjuvant radiation or chemotherapy in the management of stage I seminoma: clinical outcomes and prognostic factors for relapse in a large US cohort.". Am J Clin Oncol 37 (4): 356-9. doi:10.1097/COC.0b013e318277d839. PMID 23275274.
- ↑ URL: http://emedicine.medscape.com/article/2006777-overview. Accessed on: October 8, 2014.
- ↑ 8.0 8.1 Henley, JD.; Young, RH.; Wade, CL.; Ulbright, TM. (Sep 2004). "Seminomas with exclusive intertubular growth: a report of 12 clinically and grossly inconspicuous tumors.". Am J Surg Pathol 28 (9): 1163-8. PMID 15316315.
- ↑ URL: http://webpathology.com/image.asp?case=34&n=8. Accessed on: March 8, 2010.
- ↑ Hedinger, C.; von Hochstetter, AR.; Egloff, B. (Jul 1979). "Seminoma with syncytiotrophoblastic giant cells. A special form of seminoma.". Virchows Arch A Pathol Anat Histol 383 (1): 59-67. PMID 157614.
- ↑ Ulbright TM, Tickoo SK, Berney DM, Srigley JR (August 2014). "Best practices recommendations in the application of immunohistochemistry in testicular tumors: report from the international society of urological pathology consensus conference". Am. J. Surg. Pathol. 38 (8): e50–9. doi:10.1097/PAS.0000000000000233. PMID 24832161.
- ↑ Amin, MB.; Epstein, JI.; Ulbright, TM.; Humphrey, PA.; Egevad, L.; Montironi, R.; Grignon, D.; Trpkov, K. et al. (Aug 2014). "Best practices recommendations in the application of immunohistochemistry in urologic pathology: report from the international society of urological pathology consensus conference.". Am J Surg Pathol 38 (8): 1017-22. doi:10.1097/PAS.0000000000000254. PMID 25025364.
- ↑ 13.0 13.1 Lau, SK.; Weiss, LM.; Chu, PG. (Mar 2007). "D2-40 immunohistochemistry in the differential diagnosis of seminoma and embryonal carcinoma: a comparative immunohistochemical study with KIT (CD117) and CD30.". Mod Pathol 20 (3): 320-5. doi:10.1038/modpathol.3800749. PMID 17277761.
- ↑ 14.0 14.1 Iczkowski, KA.; Butler, SL.; Shanks, JH.; Hossain, D.; Schall, A.; Meiers, I.; Zhou, M.; Torkko, KC. et al. (Feb 2008). "Trials of new germ cell immunohistochemical stains in 93 extragonadal and metastatic germ cell tumors.". Hum Pathol 39 (2): 275-81. doi:10.1016/j.humpath.2007.07.002. PMID 18045648.
- ↑ 15.0 15.1 Cossu-Rocca, P.; Jones, TD.; Roth, LM.; Eble, JN.; Zheng, W.; Karim, FW.; Cheng, L. (Aug 2006). "Cytokeratin and CD30 expression in dysgerminoma.". Hum Pathol 37 (8): 1015-21. doi:10.1016/j.humpath.2006.02.018. PMID 16867864.
- ↑ Emerson, RE.; Ulbright, TM. (Jun 2010). "Intratubular germ cell neoplasia of the testis and its associated cancers: the use of novel biomarkers.". Pathology 42 (4): 344-55. doi:10.3109/00313021003767355. PMID 20438407.
- ↑ Hattab, EM.; Tu, PH.; Wilson, JD.; Cheng, L. (Mar 2005). "OCT4 immunohistochemistry is superior to placental alkaline phosphatase (PLAP) in the diagnosis of central nervous system germinoma.". Am J Surg Pathol 29 (3): 368-71. PMID 15725806.