Difference between revisions of "Fecal material"
Jump to navigation
Jump to search
(→Sign out: rm 'no') |
|||
| (11 intermediate revisions by the same user not shown) | |||
| Line 4: | Line 4: | ||
| Width = | | Width = | ||
| Caption = A food particle and a [[traditional adenoma|tubular adenoma]]. [[H&E stain]]. | | Caption = A food particle and a [[traditional adenoma|tubular adenoma]]. [[H&E stain]]. | ||
| Micro = plant matter - has cell walls, meat - skeletal muscle without nuclei, | | Micro = plant matter - has cell walls, meat - skeletal muscle without nuclei, microorganisms (bacilli, cocci), +/-colorectal mucosa | ||
| Subtypes = | | Subtypes = | ||
| LMDDx = [[necrosis]] | | LMDDx = [[necrosis]] | ||
| Line 20: | Line 20: | ||
| Signs = | | Signs = | ||
| Symptoms = | | Symptoms = | ||
| Prevalence = | | Prevalence = relatively common | ||
| Bloodwork = | | Bloodwork = | ||
| Rads = | | Rads = | ||
| Endoscopy = | | Endoscopy = polypoid lesion | ||
| Prognosis = | | Prognosis = benign | ||
| Other = | | Other = | ||
| ClinDDx = [[gastrointestinal polyp]] | | ClinDDx = [[gastrointestinal polyp]] | ||
| Tx = | |||
}} | }} | ||
'''Fecal material''', also '''fecal matter''', is poo. It is seen in [[gastrointestinal pathology]]. | '''Fecal material''', also '''fecal matter''', is poo. It is seen in [[gastrointestinal pathology]]. | ||
| Line 39: | Line 40: | ||
*Soft amorphous material. | *Soft amorphous material. | ||
*+/-Friable. | *+/-Friable. | ||
DDx: | |||
*[[Colonic cast]] - membranous appearance; described as airbladder of fish-like.<ref name=pmid8199700>{{Cite journal | last1 = Yoshiji | first1 = H. | last2 = Nakae | first2 = D. | last3 = Sugiya | first3 = R. | last4 = Mizumoto | first4 = Y. | last5 = Tsutsumi | first5 = M. | last6 = Hiriguchi | first6 = K. | last7 = Yokose | first7 = Y. | last8 = Sakurai | first8 = R. | last9 = Fukui | first9 = H. | title = Spontaneous passage of a colon cast in the absence of abdominal aneurysm. | journal = J Gastroenterol | volume = 29 | issue = 1 | pages = 80-3 | month = Feb | year = 1994 | doi = | PMID = 8199700 }}</ref> | |||
**Arises in [[colonic ischemia]]<ref name=pmid25216411>{{Cite journal | last1 = Abe | first1 = S. | last2 = Yamaguchi | first2 = H. | last3 = Murono | first3 = K. | last4 = Kanazawa | first4 = T. | last5 = Ishihara | first5 = S. | last6 = Sunami | first6 = E. | last7 = Watanabe | first7 = T. | title = Passage of a sigmoid colon cast in a patient with ischemic colitis. | journal = Int Surg | volume = 99 | issue = 5 | pages = 500-5 | month = | year = | doi = 10.9738/INTSURG-D-14-00066.1 | PMID = 25216411 }}</ref> - typically post-AAA repair or after colorectal surgery.<ref name=pmid17564753>{{Cite journal | last1 = Erguney | first1 = S. | last2 = Yavuz | first2 = N. | last3 = Ersoy | first3 = YE. | last4 = Teksoz | first4 = S. | last5 = Selcuk | first5 = D. | last6 = Ogut | first6 = G. | last7 = Dogusoy | first7 = G. | last8 = Alver | first8 = O. | title = Passage of "colonic cast" after colorectal surgery: report of four cases and review of the literature. | journal = J Gastrointest Surg | volume = 11 | issue = 8 | pages = 1045-51 | month = Aug | year = 2007 | doi = 10.1007/s11605-007-0194-z | PMID = 17564753 }}</ref> | |||
==Microscopic== | ==Microscopic== | ||
| Line 55: | Line 60: | ||
*[[Necrosis]]. | *[[Necrosis]]. | ||
**[[Gastrointestinal tract polyps#Colorectal adenocarcinoma|Colorectal adenocarcinoma]]. | **[[Gastrointestinal tract polyps#Colorectal adenocarcinoma|Colorectal adenocarcinoma]]. | ||
*[[Foreign material]]. | |||
===Images=== | ===Images=== | ||
| Line 70: | Line 76: | ||
==Sign out== | ==Sign out== | ||
*Often ignored if colorectal mucosa is present. | |||
<pre> | |||
Submitted as "Polyp", Cecum, Biopsy or Polypectomy: | |||
- Fecal material only. | |||
- NEGATIVE for definite colonic type mucosa. | |||
</pre> | |||
===Block letters=== | |||
<pre> | <pre> | ||
TRANSVERSE COLON, BIOPSY: | TRANSVERSE COLON, BIOPSY: | ||
- FECAL MATERIAL. | - FECAL MATERIAL. | ||
- | - NEGATIVE FOR DEFINITE COLONIC MUCOSA IDENTIFIED. | ||
</pre> | </pre> | ||
| Line 80: | Line 95: | ||
ASCENDING COLON ("POLYP"), REMOVAL: | ASCENDING COLON ("POLYP"), REMOVAL: | ||
- CONSISTENT WITH PARTIALLY DIGESTED FOOD. | - CONSISTENT WITH PARTIALLY DIGESTED FOOD. | ||
- | - NEGATIVE FOR DEFINITE COLONIC MUCOSA. | ||
</pre> | </pre> | ||
| Line 91: | Line 106: | ||
RECTUM, BIOPSY: | RECTUM, BIOPSY: | ||
- FECAL MATERIAL. | - FECAL MATERIAL. | ||
- | - NEGATIVE FOR DEFINITE RECTAL MUCOSA. | ||
</pre> | </pre> | ||
==See also== | ==See also== | ||
*[[Gastrointestinal tract polyps]]. | *[[Gastrointestinal tract polyps]]. | ||
*[[Gastrointestinal pathology]]. | *[[Gastrointestinal pathology]]. | ||
*[[Foreign material]]. | |||
==References== | |||
{{Reflist|1}} | |||
[[Category:Colon]] | |||
[[Category:Diagnosis]] | [[Category:Diagnosis]] | ||
Latest revision as of 18:33, 7 August 2018
| Fecal material | |
|---|---|
| Diagnosis in short | |
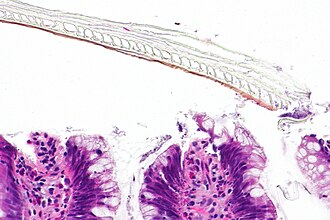 A food particle and a tubular adenoma. H&E stain. | |
|
| |
| LM | plant matter - has cell walls, meat - skeletal muscle without nuclei, microorganisms (bacilli, cocci), +/-colorectal mucosa |
| LM DDx | necrosis |
| Gross | soft material, amorphous, friable |
| Site | cecum, colon, rectum |
|
| |
| Clinical history | poor bowel preparation |
| Prevalence | relatively common |
| Endoscopy | polypoid lesion |
| Prognosis | benign |
| Clin. DDx | gastrointestinal polyp |
Fecal material, also fecal matter, is poo. It is seen in gastrointestinal pathology.
General
- Common.
- Associated with poor bowel preparation.
- People on a low-fibre diet seem to have less of 'em.[1]
- Endoscopists go after anything that is polypoid and that may be nothing more than poo.
Gross
- Soft amorphous material.
- +/-Friable.
DDx:
- Colonic cast - membranous appearance; described as airbladder of fish-like.[2]
- Arises in colonic ischemia[3] - typically post-AAA repair or after colorectal surgery.[4]
Microscopic
Features:
- Plant material:
- Yellow staining chicken wire-like material - may be linear.
- Thick cell walls often without cytoplasm and usually without a nucleus.
- Yellow staining chicken wire-like material - may be linear.
- Meat:
- Essentially ischemic skeletal muscle without inflammation.
- Eosinophilic material without nuclei and without inflammation.
- Honeycomb-like when fibres seen in cross-section.
- Eosinophilic material without nuclei and without inflammation.
- Essentially ischemic skeletal muscle without inflammation.
- +/-Microorganisms.
- +/-Inflammatory cells.
DDx:
Images
TA and plant material - intermed. mag.
Sign out
- Often ignored if colorectal mucosa is present.
Submitted as "Polyp", Cecum, Biopsy or Polypectomy: - Fecal material only. - NEGATIVE for definite colonic type mucosa.
Block letters
TRANSVERSE COLON, BIOPSY: - FECAL MATERIAL. - NEGATIVE FOR DEFINITE COLONIC MUCOSA IDENTIFIED.
Alternate
ASCENDING COLON ("POLYP"), REMOVAL:
- CONSISTENT WITH PARTIALLY DIGESTED FOOD.
- NEGATIVE FOR DEFINITE COLONIC MUCOSA.
Micro
The sections show a fragment of striated muscle without nuclei and without inflammation, with scant microorganisms. No colorectal mucosa is identified.
Rectum
RECTUM, BIOPSY: - FECAL MATERIAL. - NEGATIVE FOR DEFINITE RECTAL MUCOSA.
See also
References
- ↑ Liedenbaum, MH.; Denters, MJ.; de Vries, AH.; van Ravesteijn, VF.; Bipat, S.; Vos, FM.; Dekker, E.; Stoker, J. (Jul 2010). "Low-fiber diet in limited bowel preparation for CT colonography: Influence on image quality and patient acceptance.". AJR Am J Roentgenol 195 (1): W31-7. doi:10.2214/AJR.09.3572. PMID 20566777.
- ↑ Yoshiji, H.; Nakae, D.; Sugiya, R.; Mizumoto, Y.; Tsutsumi, M.; Hiriguchi, K.; Yokose, Y.; Sakurai, R. et al. (Feb 1994). "Spontaneous passage of a colon cast in the absence of abdominal aneurysm.". J Gastroenterol 29 (1): 80-3. PMID 8199700.
- ↑ Abe, S.; Yamaguchi, H.; Murono, K.; Kanazawa, T.; Ishihara, S.; Sunami, E.; Watanabe, T.. "Passage of a sigmoid colon cast in a patient with ischemic colitis.". Int Surg 99 (5): 500-5. doi:10.9738/INTSURG-D-14-00066.1. PMID 25216411.
- ↑ Erguney, S.; Yavuz, N.; Ersoy, YE.; Teksoz, S.; Selcuk, D.; Ogut, G.; Dogusoy, G.; Alver, O. (Aug 2007). "Passage of "colonic cast" after colorectal surgery: report of four cases and review of the literature.". J Gastrointest Surg 11 (8): 1045-51. doi:10.1007/s11605-007-0194-z. PMID 17564753.






