Difference between revisions of "Mucinous carcinoma"
Jump to navigation
Jump to search


| (29 intermediate revisions by the same user not shown) | |||
| Line 1: | Line 1: | ||
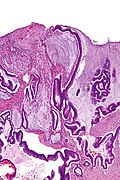
'''Mucinous carcinoma''', also '''mucinous adenocarcinoma''', is an epithelial neoplasm that produces [[mucin]]. Mucinous carcinoma can arise in a number of sites. | [[Image:Colonic mucinous adenocarcinoma - low mag.jpg|thumb|right|Colonic mucinous adenocarcinoma. [[H&E stain]].]] | ||
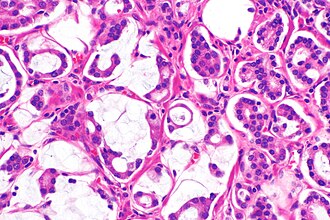
[[Image:Mucinous adenocarcinoma of prostate - 2b -- high mag.jpg|thumb|right|[[Mucinous adenocarcinoma of the prostate]] is a rare type of [[prostate cancer]]. [[H&E stain]].]] | |||
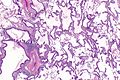
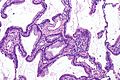
[[Image:Mucinous lung adenocarcinoma and airway -- high mag.jpg|right|thumb|Mucinous [[adenocarcinoma of the lung]] is often cytologically bland as can be seen in this image; on the right is benign ciliated epithelium and on the left is mucinous adenocarcinoma. [[H&E stain]].]] | |||
'''Mucinous carcinoma''', also '''mucinous adenocarcinoma''', is an epithelial neoplasm that produces [[mucin]]. Mucinous carcinoma can arise in a number of sites. It is also known as '''colloid carcinoma'''.<ref>URL: [http://www.merriam-webster.com/dictionary/colloid%20carcinoma http://www.merriam-webster.com/dictionary/colloid%20carcinoma]. Accessed on: 14 February 2014.</ref> | |||
==General== | ==General== | ||
| Line 5: | Line 8: | ||
*[[Mucinous breast carcinoma|Breast mucinous carcinoma]] has a better prognosis. | *[[Mucinous breast carcinoma|Breast mucinous carcinoma]] has a better prognosis. | ||
*Colorectal mucinous carcinoma has a worse prognosis.<ref name=pmid22476818>{{Cite journal | last1 = Hyngstrom | first1 = JR. | last2 = Hu | first2 = CY. | last3 = Xing | first3 = Y. | last4 = You | first4 = YN. | last5 = Feig | first5 = BW. | last6 = Skibber | first6 = JM. | last7 = Rodriguez-Bigas | first7 = MA. | last8 = Cormier | first8 = JN. | last9 = Chang | first9 = GJ. | title = Clinicopathology and Outcomes for Mucinous and Signet Ring Colorectal Adenocarcinoma: Analysis from the National Cancer Data Base. | journal = Ann Surg Oncol | volume = | issue = | pages = | month = Apr | year = 2012 | doi = 10.1245/s10434-012-2321-7 | PMID = 22476818 }}</ref> | *Colorectal mucinous carcinoma has a worse prognosis.<ref name=pmid22476818>{{Cite journal | last1 = Hyngstrom | first1 = JR. | last2 = Hu | first2 = CY. | last3 = Xing | first3 = Y. | last4 = You | first4 = YN. | last5 = Feig | first5 = BW. | last6 = Skibber | first6 = JM. | last7 = Rodriguez-Bigas | first7 = MA. | last8 = Cormier | first8 = JN. | last9 = Chang | first9 = GJ. | title = Clinicopathology and Outcomes for Mucinous and Signet Ring Colorectal Adenocarcinoma: Analysis from the National Cancer Data Base. | journal = Ann Surg Oncol | volume = | issue = | pages = | month = Apr | year = 2012 | doi = 10.1245/s10434-012-2321-7 | PMID = 22476818 }}</ref> | ||
*May be non-significant in esophagus if adjusted for grade and stage.<ref name=pmid23317610>{{Cite journal | last1 = Zheng | first1 = DJ. | last2 = Cooke | first2 = DT. | title = A survival comparison of mucin-producing adenocarcinoma of the esophagus to conventional adenocarcinoma after esophagectomy. | journal = Am Surg | volume = 79 | issue = 1 | pages = 49-53 | month = Jan | year = 2013 | doi = | PMID = 23317610 }}</ref> | |||
===Specific sites=== | |||
*[[Ovarian mucinous adenocarcinoma]]. | |||
*[[Mucinous prostate carcinoma]]. | |||
*[[Mucinous breast carcinoma]]. | |||
*[[Mucinous adenocarcinoma of the lung]]. | |||
==Gross== | |||
*Gelatinous-like material. | |||
**May have a consistency similar to ''Jello''. | |||
===Images=== | |||
*[http://www.flickr.com/photos/pulmonary_pathology/3931951819/ Mucinous adenocarcinoma of the lung (flickr.com)]. | |||
*[http://www.flickr.com/photos/euthman/482649679/ Ovarian mucinous cystadenocarcinoma (flickr.com/euthman)]. | |||
==Microscopic== | ==Microscopic== | ||
| Line 21: | Line 39: | ||
*Adenoma with [[pseudoinvasion]] (pseudocarcinoma).<ref name=Ref_Odze512>{{Ref Odze|512}}</ref> | *Adenoma with [[pseudoinvasion]] (pseudocarcinoma).<ref name=Ref_Odze512>{{Ref Odze|512}}</ref> | ||
*[[Adenocarcinoma]] with mucinous features - see ''proportion of mucin'' section. | *[[Adenocarcinoma]] with mucinous features - see ''proportion of mucin'' section. | ||
*Other [[myxoid tumours]] - has an exhaustive long DDx. | |||
*[ | |||
===Proportion of mucin=== | ===Proportion of mucin=== | ||
| Line 30: | Line 46: | ||
*[[Mucinous colorectal carcinoma]]: > 50% of the tumour.<ref name=pmid17679024 >{{cite journal |author=Tozawa E, Ajioka Y, Watanabe H, ''et al.'' |title=Mucin expression, p53 overexpression, and peritumoral lymphocytic infiltration of advanced colorectal carcinoma with mucus component: is mucinous carcinoma a distinct histological entity? |journal=Pathol. Res. Pract. |volume=203 |issue=8 |pages=567–74 |year=2007 |pmid=17679024 |doi=10.1016/j.prp.2007.04.013 |url=}}</ref> | *[[Mucinous colorectal carcinoma]]: > 50% of the tumour.<ref name=pmid17679024 >{{cite journal |author=Tozawa E, Ajioka Y, Watanabe H, ''et al.'' |title=Mucin expression, p53 overexpression, and peritumoral lymphocytic infiltration of advanced colorectal carcinoma with mucus component: is mucinous carcinoma a distinct histological entity? |journal=Pathol. Res. Pract. |volume=203 |issue=8 |pages=567–74 |year=2007 |pmid=17679024 |doi=10.1016/j.prp.2007.04.013 |url=}}</ref> | ||
*[[Mucinous gastric carcinoma]]: > 50% of the tumour. | *[[Mucinous gastric carcinoma]]: > 50% of the tumour. | ||
*Mucinous (noncystic) carcinoma of the [[pancreas]]: > 80% of the tumour.<ref name=pmid11145249>{{Cite journal | last1 = Adsay | first1 = NV. | last2 = Pierson | first2 = C. | last3 = Sarkar | first3 = F. | last4 = Abrams | first4 = J. | last5 = Weaver | first5 = D. | last6 = Conlon | first6 = KC. | last7 = Brennan | first7 = MF. | last8 = Klimstra | first8 = DS. | title = Colloid (mucinous noncystic) carcinoma of the pancreas. | journal = Am J Surg Pathol | volume = 25 | issue = 1 | pages = 26-42 | month = Jan | year = 2001 | doi = | PMID = 11145249 }}</ref> | |||
*[[Mucinous breast carcinoma]]: > 90% of the tumour.<ref name=pmid22006768>{{Cite journal | last1 = Dogan | first1 = E. | last2 = Aksoy | first2 = S. | last3 = Dizdar | first3 = O. | last4 = Arslan | first4 = C. | last5 = Dede | first5 = DS. | last6 = Ozisik | first6 = Y. | last7 = Altundag | first7 = K. | title = Pure mucinous carcinoma of the breast: a single center experience. | journal = J BUON | volume = 16 | issue = 3 | pages = 565-7 | month = | year = | doi = | PMID = 22006768 }}</ref> | *[[Mucinous breast carcinoma]]: > 90% of the tumour.<ref name=pmid22006768>{{Cite journal | last1 = Dogan | first1 = E. | last2 = Aksoy | first2 = S. | last3 = Dizdar | first3 = O. | last4 = Arslan | first4 = C. | last5 = Dede | first5 = DS. | last6 = Ozisik | first6 = Y. | last7 = Altundag | first7 = K. | title = Pure mucinous carcinoma of the breast: a single center experience. | journal = J BUON | volume = 16 | issue = 3 | pages = 565-7 | month = | year = | doi = | PMID = 22006768 }}</ref> | ||
**One source suggests: > 50% of the tumour.<ref name=pmid20191033>{{cite journal |author=Park S, Koo J, Kim JH, Yang WI, Park BW, Lee KS |title=Clinicopathological characteristics of mucinous carcinoma of the breast in Korea: comparison with invasive ductal carcinoma-not otherwise specified |journal=J. Korean Med. Sci. |volume=25 |issue=3 |pages=361–8 |year=2010 |month=March |pmid=20191033 |pmc=2826751 |doi=10.3346/jkms.2010.25.3.361 |url=}}</ref> | **One source suggests: > 50% of the tumour.<ref name=pmid20191033>{{cite journal |author=Park S, Koo J, Kim JH, Yang WI, Park BW, Lee KS |title=Clinicopathological characteristics of mucinous carcinoma of the breast in Korea: comparison with invasive ductal carcinoma-not otherwise specified |journal=J. Korean Med. Sci. |volume=25 |issue=3 |pages=361–8 |year=2010 |month=March |pmid=20191033 |pmc=2826751 |doi=10.3346/jkms.2010.25.3.361 |url=}}</ref> | ||
====Images==== | |||
=====Case===== | |||
<gallery> | |||
Image:Colonic_mucinous_adenocarcinoma_-_very_low_mag.jpg | [[Colorectal adenocarcinoma|Colonic mucinous adenocarcinoma]] - very low mag. (WC/Nephron) | |||
Image:Colonic_mucinous_adenocarcinoma_-_low_mag.jpg | Colonic mucinous adenocarcinoma - low mag. (WC/Nephron) | |||
</gallery> | |||
=====Case===== | |||
<gallery> | |||
Image: Mucinous lung adenocarcinoma -- very low mag.jpg | Mucinous [[lung adenocarcinoma]] (MLA) - very low mag. | |||
Image: Mucinous lung adenocarcinoma -- low mag.jpg | MLA - low mag. | |||
Image: Mucinous lung adenocarcinoma -- intermed mag.jpg | MLA - intermed. mag. | |||
Image: Mucinous lung adenocarcinoma - alt -- intermed mag.jpg | MLA - intermed. mag. | |||
Image: Mucinous lung adenocarcinoma -- high mag.jpg | MLA - high mag. | |||
Image: Mucinous lung adenocarcinoma -- very high mag.jpg | MLA - very high mag. | |||
Image: Mucinous lung adenocarcinoma and airway -- intermed mag.jpg | MLA - intermed. mag. | |||
Image: Mucinous lung adenocarcinoma and airway -- high mag.jpg | MLA - high mag. | |||
Image: Mucinous lung adenocarcinoma and airway - alt -- high mag.jpg | MLA - high mag. | |||
</gallery> | |||
=====www===== | |||
*[http://www.flickr.com/photos/pulmonary_pathology/3931951819/ Mucinous tumours of the ovary - several images (flickr.com)]. | |||
==Molecular== | |||
*''May'' be associated with a [[KRAS mutation]]. | |||
==IHC== | |||
IHC can be used to suggest a primary site for a mucinous adenocarcinoma:<ref name=pmid21881489>{{Cite journal | last1 = Chu | first1 = PG. | last2 = Chung | first2 = L. | last3 = Weiss | first3 = LM. | last4 = Lau | first4 = SK. | title = Determining the site of origin of mucinous adenocarcinoma: an immunohistochemical study of 175 cases. | journal = Am J Surg Pathol | volume = 35 | issue = 12 | pages = 1830-6 | month = Dec | year = 2011 | doi = 10.1097/PAS.0b013e3182299c25 | PMID = 21881489 }}</ref> | |||
*Upper GI tract: CK7 +ve (38/41 cases), CDX2 -ve (4 +ve/41 cases). | |||
*Lower GI tract: CDX2 +ve (42/42 cases), CK20 +ve (41/42 cases), CK7 -ve (8 +ve/42 cases) positive cases usu. in rectum/anus, beta-catenin (nuclear) +ve (27/42 cases). | |||
*Breast: CK7 +ve (18/18 cases), ER +ve (16/18 cases). | |||
*Lung: CK7 +ve (16/16 cases). | |||
*Gynecologic: CK7 +ve (25/27 cases). | |||
A panel: | |||
*CK7, CK20, beta-catenin, CDX2. | |||
==Sign out== | |||
In biopsies: | |||
*''Adenocarcinoma with a mucinous component'' is probably the most objective way to sign out a case, if the primary site is not firmly established and a non-mucinous component is present. | |||
<pre> | |||
OMENTUM, CORE BIOPSY: | |||
- METASTATIC MUCINOUS ADENOCARCINOMA, SEE COMMENT. | |||
COMMENT: | |||
The tumour cells stain as follows: | |||
POSITIVE: CK20, CDX2. | |||
NEGATIVE: CK7. | |||
The immunostains are suggestive of a lower gastrointestinal tract primary. Radiologic | |||
and endoscopic correlation is suggested. | |||
</pre> | |||
==See also== | ==See also== | ||
*[[Renal mucinous tubular and spindle cell carcinoma]]. | *[[Renal mucinous tubular and spindle cell carcinoma]]. | ||
*[[ | *[[Myxoid tumours]]. | ||
==References== | ==References== | ||
Latest revision as of 15:11, 22 December 2017

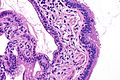
Colonic mucinous adenocarcinoma. H&E stain.

Mucinous adenocarcinoma of the lung is often cytologically bland as can be seen in this image; on the right is benign ciliated epithelium and on the left is mucinous adenocarcinoma. H&E stain.
Mucinous carcinoma, also mucinous adenocarcinoma, is an epithelial neoplasm that produces mucin. Mucinous carcinoma can arise in a number of sites. It is also known as colloid carcinoma.[1]
General
Prognostic significance dependent on the primary site:
- Breast mucinous carcinoma has a better prognosis.
- Colorectal mucinous carcinoma has a worse prognosis.[2]
- May be non-significant in esophagus if adjusted for grade and stage.[3]
Specific sites
- Ovarian mucinous adenocarcinoma.
- Mucinous prostate carcinoma.
- Mucinous breast carcinoma.
- Mucinous adenocarcinoma of the lung.
Gross
- Gelatinous-like material.
- May have a consistency similar to Jello.
Images
- Mucinous adenocarcinoma of the lung (flickr.com).
- Ovarian mucinous cystadenocarcinoma (flickr.com/euthman).
Microscopic
Features:
- Mucin - amphormous whispy or cream material.
- Cytologically atypical cells within the mucin.
- +/-Tumour without mucin.
- Maximum amount acceptable depends on the primary site (see proportion of mucin section below).
Note:
- Mucin alone -- should prompt a search for atypical cells, i.e. levels should be done.
DDx:
- Benign mucocele.
- Mucin extravasation - no malignant cells present.
- Adenoma with pseudoinvasion (pseudocarcinoma).[4]
- Adenocarcinoma with mucinous features - see proportion of mucin section.
- Other myxoid tumours - has an exhaustive long DDx.
Proportion of mucin
The criteria for diagnosing "mucinous carcinoma" varies by the anatomical site:
- Mucinous prostate carcinoma: > 25% of the tumour.[5]
- Mucinous colorectal carcinoma: > 50% of the tumour.[6]
- Mucinous gastric carcinoma: > 50% of the tumour.
- Mucinous (noncystic) carcinoma of the pancreas: > 80% of the tumour.[7]
- Mucinous breast carcinoma: > 90% of the tumour.[8]
- One source suggests: > 50% of the tumour.[9]
Images
Case
Colonic mucinous adenocarcinoma - very low mag. (WC/Nephron)
Case
Mucinous lung adenocarcinoma (MLA) - very low mag.
www
Molecular
- May be associated with a KRAS mutation.
IHC
IHC can be used to suggest a primary site for a mucinous adenocarcinoma:[10]
- Upper GI tract: CK7 +ve (38/41 cases), CDX2 -ve (4 +ve/41 cases).
- Lower GI tract: CDX2 +ve (42/42 cases), CK20 +ve (41/42 cases), CK7 -ve (8 +ve/42 cases) positive cases usu. in rectum/anus, beta-catenin (nuclear) +ve (27/42 cases).
- Breast: CK7 +ve (18/18 cases), ER +ve (16/18 cases).
- Lung: CK7 +ve (16/16 cases).
- Gynecologic: CK7 +ve (25/27 cases).
A panel:
- CK7, CK20, beta-catenin, CDX2.
Sign out
In biopsies:
- Adenocarcinoma with a mucinous component is probably the most objective way to sign out a case, if the primary site is not firmly established and a non-mucinous component is present.
OMENTUM, CORE BIOPSY: - METASTATIC MUCINOUS ADENOCARCINOMA, SEE COMMENT. COMMENT: The tumour cells stain as follows: POSITIVE: CK20, CDX2. NEGATIVE: CK7. The immunostains are suggestive of a lower gastrointestinal tract primary. Radiologic and endoscopic correlation is suggested.
See also
References
- ↑ URL: http://www.merriam-webster.com/dictionary/colloid%20carcinoma. Accessed on: 14 February 2014.
- ↑ Hyngstrom, JR.; Hu, CY.; Xing, Y.; You, YN.; Feig, BW.; Skibber, JM.; Rodriguez-Bigas, MA.; Cormier, JN. et al. (Apr 2012). "Clinicopathology and Outcomes for Mucinous and Signet Ring Colorectal Adenocarcinoma: Analysis from the National Cancer Data Base.". Ann Surg Oncol. doi:10.1245/s10434-012-2321-7. PMID 22476818.
- ↑ Zheng, DJ.; Cooke, DT. (Jan 2013). "A survival comparison of mucin-producing adenocarcinoma of the esophagus to conventional adenocarcinoma after esophagectomy.". Am Surg 79 (1): 49-53. PMID 23317610.
- ↑ Odze, Robert D.; Goldblum, John R. (2009). Surgical pathology of the GI tract, liver, biliary tract and pancreas (2nd ed.). Saunders. pp. 512. ISBN 978-1416040590.
- ↑ Grignon DJ (March 2004). "Unusual subtypes of prostate cancer". Mod. Pathol. 17 (3): 316–27. doi:10.1038/modpathol.3800052. PMID 14976541.
- ↑ Tozawa E, Ajioka Y, Watanabe H, et al. (2007). "Mucin expression, p53 overexpression, and peritumoral lymphocytic infiltration of advanced colorectal carcinoma with mucus component: is mucinous carcinoma a distinct histological entity?". Pathol. Res. Pract. 203 (8): 567–74. doi:10.1016/j.prp.2007.04.013. PMID 17679024.
- ↑ Adsay, NV.; Pierson, C.; Sarkar, F.; Abrams, J.; Weaver, D.; Conlon, KC.; Brennan, MF.; Klimstra, DS. (Jan 2001). "Colloid (mucinous noncystic) carcinoma of the pancreas.". Am J Surg Pathol 25 (1): 26-42. PMID 11145249.
- ↑ Dogan, E.; Aksoy, S.; Dizdar, O.; Arslan, C.; Dede, DS.; Ozisik, Y.; Altundag, K.. "Pure mucinous carcinoma of the breast: a single center experience.". J BUON 16 (3): 565-7. PMID 22006768.
- ↑ Park S, Koo J, Kim JH, Yang WI, Park BW, Lee KS (March 2010). "Clinicopathological characteristics of mucinous carcinoma of the breast in Korea: comparison with invasive ductal carcinoma-not otherwise specified". J. Korean Med. Sci. 25 (3): 361–8. doi:10.3346/jkms.2010.25.3.361. PMC 2826751. PMID 20191033. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2826751/.
- ↑ Chu, PG.; Chung, L.; Weiss, LM.; Lau, SK. (Dec 2011). "Determining the site of origin of mucinous adenocarcinoma: an immunohistochemical study of 175 cases.". Am J Surg Pathol 35 (12): 1830-6. doi:10.1097/PAS.0b013e3182299c25. PMID 21881489.