Difference between revisions of "Xanthogranulomatous pyelonephritis"
Jump to navigation
Jump to search
(more) |
|||
| (13 intermediate revisions by the same user not shown) | |||
| Line 1: | Line 1: | ||
{{ Infobox diagnosis | |||
| Name = {{PAGENAME}} | |||
| Image = Xanthogranulomatous_pyelonephritis_cd68.jpg | |||
| Width = | |||
| Caption = Xanthogranulomatous pyelonephritis. CD68 immunostain. | |||
| Synonyms = | |||
| Micro = abundant (foamy) macrophages (associated with the collecting system - medulla, not cortex), +/-giant cells, +/-cholesterol clefts, +/-interstitial lymphocytes and plasma cells, +/-interstitial fibrosis, +/-calcifications | |||
| Subtypes = | |||
| LMDDx = [[malakoplakia]], RCC - especially [[PRCC]], granulomatous disease, [[chronic pyelonephritis]], interstitial nephritis, occasionally [[renal cell carcinoma]] | |||
| Stains = [[PAS-D]] -ve | |||
| IHC = CD68 +ve, CD10 -ve, [[pankeratin]] -ve | |||
| EM = | |||
| Molecular = | |||
| IF = | |||
| Gross = | |||
| Grossing = | |||
| Site = [[kidney]] - see ''[[kidney tumours]]'' | |||
| Assdx = [[diabetes mellitus]], history of UTI, [[nephrolithiasis]], GU obstruction (various causes) | |||
| Syndromes = | |||
| Clinicalhx = | |||
| Signs = | |||
| Symptoms = | |||
| Prevalence = uncommon | |||
| Bloodwork = | |||
| Rads = dilated upper GU system | |||
| Endoscopy = | |||
| Prognosis = | |||
| Other = | |||
| ClinDDx = [[renal cell carcinoma]], [[pyelonephritis]] | |||
| Tx = antibiotics, occasionally nephrectomy | |||
}} | |||
'''Xanthogranulomatous pyelonephritis''', abbreviated '''XGP''', is an inflammatory process of the [[kidney]] that can mimic [[renal cell carcinoma]]. | '''Xanthogranulomatous pyelonephritis''', abbreviated '''XGP''', is an inflammatory process of the [[kidney]] that can mimic [[renal cell carcinoma]]. | ||
| Line 6: | Line 37: | ||
*Associated with: | *Associated with: | ||
**[[Diabetes mellitus]]. | **[[Diabetes mellitus]]. | ||
**History of | **History of [[urinary tract infection]].<ref name=pmid17987581>{{cite journal |author=Afgan F, Mumtaz S, Ather MH |title=Preoperative diagnosis of xanthogranulomatous pyelonephritis |journal=Urol J |volume=4 |issue=3 |pages=169–73 |year=2007 |pmid=17987581 |doi= |url=}}</ref> | ||
**[[Nephrolithiasis]]. | **[[Nephrolithiasis]]. | ||
**GU obstruction.<ref name=pmid17098659>{{cite journal |author=Al-Ghazo MA, Ghalayini IF, Matalka II, Al-Kaisi NS, Khader YS |title=Xanthogranulomatous pyelonephritis: Analysis of 18 cases |journal=Asian J Surg |volume=29 |issue=4 |pages=257–61 |year=2006 |month=October |pmid=17098659 |doi= |url=}}</ref> | **GU obstruction.<ref name=pmid17098659>{{cite journal |author=Al-Ghazo MA, Ghalayini IF, Matalka II, Al-Kaisi NS, Khader YS |title=Xanthogranulomatous pyelonephritis: Analysis of 18 cases |journal=Asian J Surg |volume=29 |issue=4 |pages=257–61 |year=2006 |month=October |pmid=17098659 |doi= |url=}}</ref> | ||
| Line 13: | Line 44: | ||
==Microscopic== | ==Microscopic== | ||
*Abundant macrophages. | Features: | ||
*Abundant (foamy) macrophages. | |||
**Associated with the collecting system - medulla, not cortex. | |||
*+/-Giant cells. | *+/-Giant cells. | ||
*+/-Interstitial lymphocytes and plasma cells. | |||
*+/-Interstitial fibrosis. | |||
*+/-Cholesterol clefts (common). | |||
*+/-Calcifications - dystrophic. | |||
DDx: | DDx: | ||
*[[Malakoplakia]]. | *[[Malakoplakia]]. | ||
**Basophilic inclusions -- inside or outside of macrophages - often size of RBC or larger ([[Michaelis-Gutmann bodies]]). | **Basophilic inclusions -- inside or outside of macrophages - often size of RBC or larger ([[Michaelis-Gutmann bodies]]). | ||
* | *[[Renal cell carcinoma]] - especially [[papillary RCC]] (as this has foamy macrophages). | ||
*Granulomatous disease. | *[[Granulomatous disease]]. | ||
*[[Chronic pyelonephritis]]. | *[[Chronic pyelonephritis]]. | ||
*[[Interstitial nephritis]]. | *[[Interstitial nephritis]]. | ||
*[[Renal cell carcinoma]] - foamy macrophages may be abundant.<ref name=pmid8378177>{{Cite journal | last1 = Iskandar | first1 = SS. | last2 = Prahlow | first2 = JA. | last3 = White | first3 = WL. | title = Lipid-laden foamy macrophages in renal cell carcinoma. Potential frozen section diagnostic pitfall. | journal = Pathol Res Pract | volume = 189 | issue = 5 | pages = 549-52 | month = Jun | year = 1993 | doi = 10.1016/S0344-0338(11)80364-X | PMID = 8378177 }}</ref> | |||
=== | ===Images=== | ||
<gallery> | <gallery> | ||
Image:Xanthogranulomatous_pyelonephritis_cd68.jpg | Xanthogranulomatous pyelonephritis - CD68 stain. (WC/Nephron) | Image:Xanthogranulomatous_pyelonephritis_cd68.jpg | Xanthogranulomatous pyelonephritis - CD68 stain. (WC/Nephron) | ||
</gallery> | </gallery> | ||
www: | |||
*[http://www.archivesofpathology.org/na101/home/literatum/publisher/pinnacle/journals/content/arpa/2011/15432165-135.5/2009-0769-rsr.1/production/images/large/i1543-2165-135-5-671-f01.jpeg Several images of XGP (archivesofpathology.org)].<ref name=pmid21526966>{{Cite journal | last1 = Li | first1 = L. | last2 = Parwani | first2 = AV. | title = Xanthogranulomatous pyelonephritis. | journal = Arch Pathol Lab Med | volume = 135 | issue = 5 | pages = 671-4 | month = May | year = 2011 | doi = 10.1043/2009-0769-RSR.1 | PMID = 21526966 }}</ref> | |||
==Stains== | ==Stains== | ||
| Line 43: | Line 82: | ||
- CHRONIC INTERSTITIAL NEPHRITIS. | - CHRONIC INTERSTITIAL NEPHRITIS. | ||
- INCREASED NUMBERS OF TOTALLY SCLEROSED GLOMERULI AND GLOMERULI WITH FOCAL | - INCREASED NUMBERS OF TOTALLY SCLEROSED GLOMERULI AND GLOMERULI WITH FOCAL | ||
SCLEROSIS. | |||
- MARKED INTERSTITIAL FIBROSIS. | - MARKED INTERSTITIAL FIBROSIS. | ||
- NEGATIVE FOR MALIGNANCY. | - NEGATIVE FOR MALIGNANCY. | ||
| Line 66: | Line 105: | ||
immunostain. | immunostain. | ||
</pre> | </pre> | ||
===Micro=== | |||
The sections show degenerative renal parenchyma with surrounding histiocytes, other inflammatory cells, fibrosis and cholesterol clefts. | |||
==See also== | ==See also== | ||
*[[Kidney tumours]]. | *[[Kidney tumours]]. | ||
*[[Acute pyelonephritis]]. | |||
*[[Xanthogranulomatous cystitis]]. | |||
==References== | ==References== | ||
Latest revision as of 02:38, 22 February 2017
| Xanthogranulomatous pyelonephritis | |
|---|---|
| Diagnosis in short | |
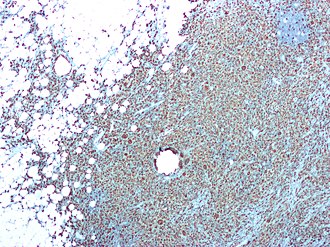 Xanthogranulomatous pyelonephritis. CD68 immunostain. | |
|
| |
| LM | abundant (foamy) macrophages (associated with the collecting system - medulla, not cortex), +/-giant cells, +/-cholesterol clefts, +/-interstitial lymphocytes and plasma cells, +/-interstitial fibrosis, +/-calcifications |
| LM DDx | malakoplakia, RCC - especially PRCC, granulomatous disease, chronic pyelonephritis, interstitial nephritis, occasionally renal cell carcinoma |
| Stains | PAS-D -ve |
| IHC | CD68 +ve, CD10 -ve, pankeratin -ve |
| Site | kidney - see kidney tumours |
|
| |
| Associated Dx | diabetes mellitus, history of UTI, nephrolithiasis, GU obstruction (various causes) |
| Prevalence | uncommon |
| Radiology | dilated upper GU system |
| Clin. DDx | renal cell carcinoma, pyelonephritis |
| Treatment | antibiotics, occasionally nephrectomy |
Xanthogranulomatous pyelonephritis, abbreviated XGP, is an inflammatory process of the kidney that can mimic renal cell carcinoma.
General
- May mimic renal cell carcinoma - especially radiologically.
- Usually lower pole.[citation needed]
- Associated with:
- Diabetes mellitus.
- History of urinary tract infection.[1]
- Nephrolithiasis.
- GU obstruction.[2]
- Occasionally an indication for nephrectomy.[1][2]
- Most common organism (in the context of nephrectomy specimens) - Proteus mirabilis.[2]
Microscopic
Features:
- Abundant (foamy) macrophages.
- Associated with the collecting system - medulla, not cortex.
- +/-Giant cells.
- +/-Interstitial lymphocytes and plasma cells.
- +/-Interstitial fibrosis.
- +/-Cholesterol clefts (common).
- +/-Calcifications - dystrophic.
DDx:
- Malakoplakia.
- Basophilic inclusions -- inside or outside of macrophages - often size of RBC or larger (Michaelis-Gutmann bodies).
- Renal cell carcinoma - especially papillary RCC (as this has foamy macrophages).
- Granulomatous disease.
- Chronic pyelonephritis.
- Interstitial nephritis.
- Renal cell carcinoma - foamy macrophages may be abundant.[3]
Images
www:
Stains
- PAS-D -ve.
- Done to look for malakoplakia.
IHC
- CD68 +ve.
- RCC markers (CD10, RCC) all negative.
Sign out
RIGHT KIDNEY, NEPHRECTOMY: - XANTHOGRANULOMATOUS PYELONEPHRITIS. - CHRONIC INTERSTITIAL NEPHRITIS. - INCREASED NUMBERS OF TOTALLY SCLEROSED GLOMERULI AND GLOMERULI WITH FOCAL SCLEROSIS. - MARKED INTERSTITIAL FIBROSIS. - NEGATIVE FOR MALIGNANCY. COMMENT: Immunostaining demonstrates abundant CD68 positive cells (macrophages). A CD10 immunostain is non-concerning (it highlights glomeruli). A pankeratin immunostain is non-concerning (it highlights benign renal tubules).
Compatible XGP
"KIDNEY" LESION, LEFT, BIOPSY: - FIBROMUSCULAR TISSUE WITH A MIXED INFLAMMATORY INFILTRATE. - CELLULAR DEBRIS WITH SURROUNDING LOOSELY AGGREGATED HISTIOCYTES. - NO RENAL PARENCHYMA IDENTIFIED. - NEGATIVE FOR MALIGNANCY. COMMENT: A SMA immunostain highlights the muscle component, and a CD68 immunostain marks abundant histiocytes. No epithelial component is identified with a pankeratin immunostain.
Micro
The sections show degenerative renal parenchyma with surrounding histiocytes, other inflammatory cells, fibrosis and cholesterol clefts.
See also
References
- ↑ 1.0 1.1 Afgan F, Mumtaz S, Ather MH (2007). "Preoperative diagnosis of xanthogranulomatous pyelonephritis". Urol J 4 (3): 169–73. PMID 17987581.
- ↑ 2.0 2.1 2.2 Al-Ghazo MA, Ghalayini IF, Matalka II, Al-Kaisi NS, Khader YS (October 2006). "Xanthogranulomatous pyelonephritis: Analysis of 18 cases". Asian J Surg 29 (4): 257–61. PMID 17098659.
- ↑ Iskandar, SS.; Prahlow, JA.; White, WL. (Jun 1993). "Lipid-laden foamy macrophages in renal cell carcinoma. Potential frozen section diagnostic pitfall.". Pathol Res Pract 189 (5): 549-52. doi:10.1016/S0344-0338(11)80364-X. PMID 8378177.
- ↑ Li, L.; Parwani, AV. (May 2011). "Xanthogranulomatous pyelonephritis.". Arch Pathol Lab Med 135 (5): 671-4. doi:10.1043/2009-0769-RSR.1. PMID 21526966.
