Difference between revisions of "Uterine prolapse"
Jump to navigation
Jump to search
| (One intermediate revision by the same user not shown) | |||
| Line 28: | Line 28: | ||
==Sign out== | ==Sign out== | ||
<pre> | |||
Uterus, Cervix and Vagina Mucosa, Total Hysterectomy: | |||
- Uterine cervix with focal keratinization, otherwise within normal limits. | |||
- Inactive endometrium. | |||
- Squamous mucosa with keratinization, consistent with prolapse-associated | |||
changes in the vagina. | |||
- Medial calcific sclerosis. | |||
- Atherosclerosis, moderate-to-severe. | |||
- NEGATIVE for malignancy. | |||
</pre> | |||
<pre> | <pre> | ||
Submitted as "Uterine Cervix", Excision: | Submitted as "Uterine Cervix", Excision: | ||
| Line 34: | Line 45: | ||
Comment: | Comment: | ||
The stromal atypia is favoured to be benign change, as it is without significant proliferation | The stromal atypia is favoured to be benign change, as it is without significant proliferation, | ||
not mass forming. | not mass forming and near the stromal-epithelial interface. | ||
The stromal cells stain as follows: | The stromal cells stain as follows: | ||
Latest revision as of 19:10, 8 July 2016
Uterine prolapse is a frequent benign pathology of the uterus and a common reason for hysterectomy.
General
- Clinical diagnosis.
- A common indication for a total hysterectomy.
- Hysterectomy specimen usually comes with some vaginal mucosa.
- Parous women, usually menopausal.[1]
- Possibly obesity - studies vary.[2]
Gross
- Long cervix.
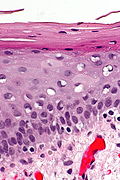
Microscopic
Features:
- Uterus: non-specific.
- Vaginal mucosa: (focal) keratinization due to rubbing - common finding.
Note:
Images
Sign out
Uterus, Cervix and Vagina Mucosa, Total Hysterectomy: - Uterine cervix with focal keratinization, otherwise within normal limits. - Inactive endometrium. - Squamous mucosa with keratinization, consistent with prolapse-associated changes in the vagina. - Medial calcific sclerosis. - Atherosclerosis, moderate-to-severe. - NEGATIVE for malignancy.
Submitted as "Uterine Cervix", Excision: - Squamous mucosa with hyperplasia, parakeratosis, and stromal atypia, see comment. - NEGATIVE for dysplasia and NEGATIVE for evidence of malignancy. Comment: The stromal atypia is favoured to be benign change, as it is without significant proliferation, not mass forming and near the stromal-epithelial interface. The stromal cells stain as follows: POSITIVE: vimentin, ER. NEGATIVE: AE1/AE3, CD10. PROLIFERATION (Ki-67): <1%.
Block letters
UTERUS AND CERVIX, TOTAL HYSTERECTOMY: - UTERINE CERVIX WITH FOCAL KERATINIZATION OTHERWISE WITHIN NORMAL LIMITS. - NONPROLIFERATIVE ENDOMETRIUM.
UTERUS AND CERVIX, TOTAL HYSTERECTOMY: - UTERINE CERVIX WITH KERATINIZATION, OTHERWISE WITHIN NORMAL LIMITS. - CYSTIC NONPROLIFERATIVE ENDOMETRIUM. - UTERINE SMOOTH MUSCLE AND SEROSA WITHIN NORMAL LIMITS. - NEGATIVE FOR MALIGNANCY.
Denudated exocervix
UTERUS AND CERVIX, TOTAL HYSTERECTOMY: - UTERINE CERVIX WITH MILD CHRONIC INFLAMMATION AND EXOCERVICAL DENUDATION, NO EVIDENCE OF DYSPLASIA. - CYSTIC NONPROLIFERATIVE ENDOMETRIUM. - UTERINE CORPUS WITH BENIGN HYALINIZED NODULE. - NEGATIVE FOR MALIGNANCY. COMMENT: Levels were cut on the uterine cervix sections (A1 and A2).
Focal ulceration
- UTERINE CERVIX WITH PARAKERATOSIS, ACANTHOSIS, CHRONIC INFLAMMATION, AND FOCAL ULCERATION ASSOCIATED WITH GRANULATION TISSUE FORMATION. - PARTIALLY CYSTIC NONPROLIFERATIVE ENDOMETRIUM. - UTERINE CORPUS WITH LEIOMYOMA. - NO EVIDENCE OF DYSPLASIA. - NEGATIVE FOR HYPERPLASIA AND NEGATIVE FOR MALIGNANCY.
With endometrial polyp
UTERUS AND CERVIX, TOTAL HYSTERECTOMY: - BENIGN ENDOMETRIAL POLYP WITH NONPROLIFERATIVE ENDOMETRIAL GLANDS. - UTERINE CERVIX WITH MILD CHRONIC INFLAMMATION AND FOCAL EXOCERVICAL DENUDATION, NO EVIDENCE OF DYSPLASIA. - VERY WEAKLY PROLIFERATIVE ENDOMETRIUM, MOSTLY ATROPHIC APPEARING, NEGATIVE FOR ENDOMETRIAL HYPERPLASIA. - UTERINE CORPUS WITHIN NORMAL LIMITS. - NEGATIVE FOR MALIGNANCY.
See also
References
- ↑ Mladenović-Segedi, L.; Segedi, D.. "[Most important etiologic factors in the development of genital prolapse].". Srp Arh Celok Lek 138 (5-6): 315-8. PMID 20607975.
- ↑ Thubert, T.; Deffieux, X.; Letouzey, V.; Hermieu, JF. (Jul 2012). "[Obesity and urogynecology: a systematic review].". Prog Urol 22 (8): 445-53. doi:10.1016/j.purol.2012.03.009. PMID 22732579.
- ↑ Nucci, MR.; Young, RH.; Fletcher, CD. (Feb 2000). "Cellular pseudosarcomatous fibroepithelial stromal polyps of the lower female genital tract: an underrecognized lesion often misdiagnosed as sarcoma.". Am J Surg Pathol 24 (2): 231-40. PMID 10680891.
- ↑ Rodrigues, MI et al. (April-June 2009). [http://www.medigraphic.com/pdfs/patrevlat/rlp-2009/rlp092e.pdf "Atypical stromal cells as a diagnostic pitfall in lesions of the lower female genital tract and uterus: a review and presentation of some unusual cases"]. Patología 47 (2): 103-7. http://www.medigraphic.com/pdfs/patrevlat/rlp-2009/rlp092e.pdf.