Difference between revisions of "Neuroendocrine tumour of the appendix"
Jump to navigation
Jump to search
(→Gross) |
|||
| Line 18: | Line 18: | ||
==Gross== | ==Gross== | ||
*Classically found in the tip of the appendix. | *Classically found in the tip of the appendix. | ||
*Characteristic yellow cut surface | *Characteristic yellow cut surface post-[[fixation]]. | ||
*Circumscribed but not encapsulated | *Circumscribed but not encapsulated. | ||
*Firm (due to desmoplasia) | *Firm (due to desmoplasia). | ||
*Centred in the submucosa | *Centred in the submucosa. | ||
*Nodules that do not usually cause erosion of the overlying mucosa. | *Nodules that do not usually cause erosion of the overlying mucosa. | ||
Revision as of 07:39, 19 March 2015
Neuroendocrine tumour of the appendix is a common tumour of the vermiform appendix. It is also known as appendiceal neuroendocrine tumour, abbreviated appendiceal NET.
It was previously known as appendiceal carcinoid.
General
- Most common tumour of the appendix.[1]
- Not really common though - one is seen in approximately 300 appendectomies.[2]
Presentation
- Often found incidentally, may be microscopic.
- May cause obstruction leading to mucocele or acute appendicitis.
- May precipitate torsion.
Size matters in appendiceal NETs:[3]
- <1.0 cm - do not metastasize.
- 1.0-2.0 cm - rarely metastasize.
Gross
- Classically found in the tip of the appendix.
- Characteristic yellow cut surface post-fixation.
- Circumscribed but not encapsulated.
- Firm (due to desmoplasia).
- Centred in the submucosa.
- Nodules that do not usually cause erosion of the overlying mucosa.
Image
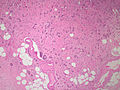
Microscopic
Features:
- Classically subepithelial/mural.
- Various growth patterns:
- Nested (insular).
- Trabecular.
- Palisading.
- Ribbons, rosettes.
- Fibrous stroma in between cell groups.
- Cytomorphology:
- Monotonous appearance with scanty mitoses.
- Round central nuclei.
- Stippled chromatin (AKA salt-and-pepper chromatin and coarse chromatin).
- Eosinophilic granular cytoplasm.
DDx:
- Colorectal adenocarcinoma.
- Adenocarcinoid.
- Crypt cell carcinoma, also known as goblet cell carcinoid.
- Metastatic adenocarcinoma.
- Normal ganglion cells in the Meissner plexus (submucosa) and Auerbach plexus (located between the inner and outer layers of the muscularis propria).
Special Types
- Tubular carcinoid.
- Neuroendocrine cells forming tubules (no cell nests).
- Some tubules can contain mucin.
- Can be confused with adenocarcinoma.
- Features suggesting tubular carcinoid (over adenocarcinoma):
- Arises from base of crypts, with no disruption of surface epithelium.
- No associated epithelial precursor (no adenomatous change).
- Neuroendocrine cytologic features, without prominent atypia.
- IHC (NE markers +ve).
- Goblet cell carcinoid - dealt with in the article crypt cell carcinoma.
- Signet-ring cells forming glandular structures.
- Possibly also with extra-cellular mucin.[citation needed]
Images
www:
- Appendiceal carcinoid (humpath.com).
- Carcinoid of the appendix (brown.edu).
- Appendiceal carcinoid (flickr.com/Qiao).
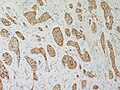
IHC
Features:
- Chromogranin A -ve/+ve.
- Synaptophysin +ve.
- Keratin positive, but CK7/CK20 negative.[citation needed]
- S100 positive for appendix.[citation needed]
See also
References
- ↑ Mitchell, Richard; Kumar, Vinay; Fausto, Nelson; Abbas, Abul K.; Aster, Jon (2011). Pocket Companion to Robbins & Cotran Pathologic Basis of Disease (8th ed.). Elsevier Saunders. pp. 435. ISBN 978-1416054542.
- ↑ Mitra, B.; Pal, M.; Paul, B.; Saha, TN.; Maiti, A. (2013). "Goblet cell carcinoid of appendix: A rare case with literature review.". Int J Surg Case Rep 4 (3): 334-7. doi:10.1016/j.ijscr.2013.01.007. PMID 23416502.
- ↑ Modlin, IM.; Lye, KD.; Kidd, M. (Feb 2003). "A 5-decade analysis of 13,715 carcinoid tumors.". Cancer 97 (4): 934-59. doi:10.1002/cncr.11105. PMID 12569593.