Difference between revisions of "Adrenocortical carcinoma"
Jump to navigation
Jump to search
(→Images) |
(→Images) |
||
| Line 73: | Line 73: | ||
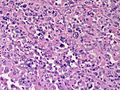
Image:Adrenal CorticalCarcinoma HP PA.JPG|Adrenal Cortical Carcinoma - high power (SKB) | Image:Adrenal CorticalCarcinoma HP PA.JPG|Adrenal Cortical Carcinoma - high power (SKB) | ||
Image:Adrenal CorticalCarcinoma HP3 RBWH.JPG|Adrenal Cortical Carcinoma - high power (SKB) | Image:Adrenal CorticalCarcinoma HP3 RBWH.JPG|Adrenal Cortical Carcinoma - high power (SKB) | ||
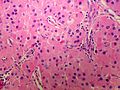
Image:Adrenal CorticalCarcinoma MP CTR (3).jpg|Adrenal Cortical Carcinoma - Medium power(SKB) | |||
Image:Adrenal CorticalCarcinoma MP CTR (4).jpg|Adrenal Cortical Carcinoma - Medium power(SKB) | |||
Image:Adrenal CorticalCarcinoma MP CTR.jpg|Adrenal Cortical Carcinoma - Medium power(SKB) | |||
Image:Adrenal CorticalCarcinoma MP CTR (2).jpg|Adrenal Cortical Carcinoma - Medium power(SKB) | |||
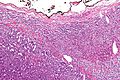
Image:Adrenal CorticalCarcinoma LP PA.JPG|Adrenal Cortical Carcinoma - Low power(SKB) | |||
Image:Adrenal CorticalCarcinoma LP PA (2).JPG|Adrenal Cortical Carcinoma - Low power(SKB) | |||
</gallery> | </gallery> | ||
www: | www: | ||
Revision as of 11:55, 8 March 2015
| Adrenocortical carcinoma | |
|---|---|
| Diagnosis in short | |
 Adrenocortical carcinoma. H&E stain. | |
|
| |
| Synonyms | adrenal cortical carcinoma |
|
| |
| LM | see below - various criteria, dependent on adult vs pediatric |
| IHC | vimentin +ve, melan A +ve, inhibin-alpha +ve, chromogranin A -ve, EMA -ve, S-100 -ve |
| Site | adrenal gland - cortex |
|
| |
| Syndromes | Li-Fraumeni syndrome, Beckwith-Wiedemann syndrome |
|
| |
| Prevalence | uncommon |
| Radiology | adrenal mass, typically large |
| Prognosis | poor |
| Clin. DDx | renal cell carcinoma, other abdominal masses |
| Treatment | surgical excision if feasible |
Adrenocortical carcinoma, abbreviated ACC, is a malignant tumour of the adrenal gland cortex.
It is also known as adrenal cortical carcinoma.
General
- Prognosis poor, especially in adults.
Epidemiology:
- May be associated with a syndrome:[1]
Gross
- +/-Encapsulated.
- Necrotic-appearing.
Image:
Microscopic
Various criteria exist for this diagnosis. The most widely used is the Weiss criteria, which is a big long clunker.
Notes:
- Tumour may contain fat.[2]
Images
www:
Adult
Weiss criteria
Three of the following:[3]
- High nuclear grade.
- High mitotic rate; >5/50 HPF (@ 40X obj.) - definition suffers from HPFitis.
- Atypical mitoses.
- Cleared cytoplasm in >= 25% of tumour cells.
- Sheeting (diffuse architecture) in >= 1/3 of tumour cells.
- Necrosis in nests.
- Venous invasion.
- Adrenal sinusoid invasion; lymphovascular space invasion within the adrenal gland.
- Capsular invasion.
Volante criteria
There is a simplified set of criteria by Volante et al. - that is not widely used:[4]
- Reticular network disruption (with reticulin staining).
- One of the three following:
- Abundant mitoses >5/50 high-power fields - definition suffers from HPFitis.
- Necrosis.
- Vascular invasion.
Pediatric
The criteria in the pediatric setting are somewhat different. This is discussed by Wieneke et al.[5] and Dehner and Hill.[6]
Dehner and Hill propose a very simple system:[6]
- "Low risk" < 200 g & confined to the adrenal.
- "Intermediate risk" 200-400 g, no mets, +/-microscopic disease outside adrenal.
- "High risk" >400 g, or mets, or gross invasion of adjacent structures.
IHC
- Vimentin +ve.
- Melan A +ve.
- Inhibin-alpha +ve.
- Cytokeratins +ve/-ve.
Others:
- Synaptophysin +ve/-ve.
- Chromogranin A -ve.
- Pheochromocytoma +ve.
- EMA -ve.
- Renal cell carcinoma +ve.
- S100 -ve.
- Pheochromocytoma +ve (sustentacular cells).[7]
- PAX-8 -ve.[8]
- CD10 +ve/-ve -- cannot be used to differentiate from RCC.[9]
See also
References
- ↑ Kumar, Vinay; Abbas, Abul K.; Fausto, Nelson; Aster, Jon (2009). Robbins and Cotran pathologic basis of disease (8th ed.). Elsevier Saunders. pp. 1157. ISBN 978-1416031215.
- ↑ Heye S, Woestenborghs H, Van Kerkhove F, Oyen R (2005). "Adrenocortical carcinoma with fat inclusion: case report". Abdom Imaging 30 (5): 641–3. doi:10.1007/s00261-004-0281-5. PMID 15688105.
- ↑ Jain M, Kapoor S, Mishra A, Gupta S, Agarwal A (2010). "Weiss criteria in large adrenocortical tumors: a validation study". Indian J Pathol Microbiol 53 (2): 222–6. doi:10.4103/0377-4929.64325. PMID 20551521.
- ↑ Volante M, Bollito E, Sperone P, et al. (November 2009). "Clinicopathological study of a series of 92 adrenocortical carcinomas: from a proposal of simplified diagnostic algorithm to prognostic stratification". Histopathology 55 (5): 535–43. doi:10.1111/j.1365-2559.2009.03423.x. PMID 19912359.
- ↑ Wieneke JA, Thompson LD, Heffess CS (July 2003). "Adrenal cortical neoplasms in the pediatric population: a clinicopathologic and immunophenotypic analysis of 83 patients". Am. J. Surg. Pathol. 27 (7): 867–81. PMID 12826878.
- ↑ 6.0 6.1 Dehner LP, Hill DA (2009). "Adrenal cortical neoplasms in children: why so many carcinomas and yet so many survivors?". Pediatr. Dev. Pathol. 12 (4): 284–91. doi:10.2350/08-06-0489.1. PMID 19326954.
- ↑ Unger P, Hoffman K, Pertsemlidis D, Thung S, Wolfe D, Kaneko M (May 1991). "S100 protein-positive sustentacular cells in malignant and locally aggressive adrenal pheochromocytomas". Arch. Pathol. Lab. Med. 115 (5): 484–7. PMID 1673596.
- ↑ Sangoi, AR.; Fujiwara, M.; West, RB.; Montgomery, KD.; Bonventre, JV.; Higgins, JP.; Rouse, RV.; Gokden, N. et al. (May 2011). "Immunohistochemical distinction of primary adrenal cortical lesions from metastatic clear cell renal cell carcinoma: a study of 248 cases.". Am J Surg Pathol 35 (5): 678-86. doi:10.1097/PAS.0b013e3182152629. PMID 21490444.
- ↑ Mete, O.; Kapran, Y.; Güllüoğlu, MG.; Kiliçaslan, I.; Erbil, Y.; Senyürek, YG.; Dizdaroğlu, F. (May 2010). "Anti-CD10 (56C6) is expressed variably in adrenocortical tumors and cannot be used to discriminate clear cell renal cell carcinomas.". Virchows Arch 456 (5): 515-21. doi:10.1007/s00428-010-0901-0. PMID 20390424.
.