Difference between revisions of "Diversion colitis"
Jump to navigation
Jump to search
(split-out) |
(+infobox) |
||
| Line 1: | Line 1: | ||
{{ Infobox diagnosis | |||
| Name = {{PAGENAME}} | |||
| Image = Diversion_proctitis_-_low_mag.jpg | |||
| Width = | |||
| Caption = Diversion proctitis. [[H&E stain]]. | |||
| Micro = | |||
| Subtypes = | |||
| LMDDx = | |||
| Stains = | |||
| IHC = | |||
| EM = | |||
| Molecular = | |||
| IF = | |||
| Gross = | |||
| Grossing = | |||
| Site = [[colon]], [[rectum]] | |||
| Assdx = | |||
| Syndromes = | |||
| Clinicalhx = previous diversion - very important | |||
| Signs = | |||
| Symptoms = | |||
| Prevalence = uncommon | |||
| Bloodwork = | |||
| Rads = | |||
| Endoscopy = | |||
| Prognosis = usu. resolves with re-anastomosis | |||
| Other = | |||
| ClinDDx = other cause of [[colitis]] | |||
}} | |||
'''Diversion colitis''' is [[colitis]] due to a diversion, i.e. a [[stoma]]. '''Diversion proctitis''' redirects here. | '''Diversion colitis''' is [[colitis]] due to a diversion, i.e. a [[stoma]]. '''Diversion proctitis''' redirects here. | ||
Revision as of 01:34, 12 December 2013
| Diversion colitis | |
|---|---|
| Diagnosis in short | |
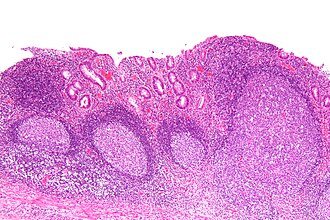 Diversion proctitis. H&E stain. | |
| Site | colon, rectum |
|
| |
| Clinical history | previous diversion - very important |
| Prevalence | uncommon |
| Prognosis | usu. resolves with re-anastomosis |
| Clin. DDx | other cause of colitis |
Diversion colitis is colitis due to a diversion, i.e. a stoma. Diversion proctitis redirects here.
General
- Segment of de-functioned bowel due to surgical diversion, i.e. stoma (ileostomy or colostomy).
- Diagnosis dependent on history - key point.
Gross
Features:[1]
- Ulceration - classic.
- Surgical changes, e.g. fibrotic-appearing thickened wall.
- May not be apparent.
Microscopic
Features:[1]
- Follicular lymphoid hyperplasia - key feature.[2]
- Abundant lymphoid nodules.
- Plasma cells and lymphocytes.
- +/-Changes of an active colitis - uncommon:[3]
- Cryptitis.
- Crypt abscesses.
Notes:
- May show IBD-like changes.[4]
- IBD should not be diagnosed on a diverted segment of bowel.
DDx:[5]
- Inflammatory bowel disease - no stoma.
- Ischemic colitis.
- Infectious colitis.
Images
Sign out
SIGMOID COLON, BIOPSIES: - MILD ACTIVE COLITIS WITH LAMINA PROPRIA FIBROSIS, SEE COMMENT. - NEGATIVE FOR DYSPLASIA. COMMENT: No granulomas are identified. Follicular lymphoid hyperplasia is not identified; however, there is no definite submucosa present. Diverted segments of bowel can have inflammatory bowel disease-like changes. In the context of a diverted segment of bowel, the findings are compatible with a diversion colitis.
RECTUM, BIOPSY: - CHRONIC ACTIVE PROCTITIS WITH FOCAL ULCERATION, CRYPTITIS AND CRYPT ABSCESSES. - GRANULATION TISSUE. - NEGATIVE FOR DYSPLASIA. COMMENT: No lymphoid hyperplasia is present. A small lymphoid aggregate is present. Architectural distortion is present. In the context of a diverted segment of bowel, the findings are compatible with a diversion colitis.
See also
References
- ↑ 1.0 1.1 Edwards, CM.; George, B.; Warren, B. (Jan 1999). "Diversion colitis--new light through old windows.". Histopathology 34 (1): 1-5. PMID 9934577.
- ↑ Yeong, ML.; Bethwaite, PB.; Prasad, J.; Isbister, WH. (Jul 1991). "Lymphoid follicular hyperplasia--a distinctive feature of diversion colitis.". Histopathology 19 (1): 55-61. PMID 1916687.
- ↑ Ma, CK.; Gottlieb, C.; Haas, PA. (Apr 1990). "Diversion colitis: a clinicopathologic study of 21 cases.". Hum Pathol 21 (4): 429-36. PMID 2318485.
- ↑ Yantiss, RK.; Odze, RD. (Jan 2006). "Diagnostic difficulties in inflammatory bowel disease pathology.". Histopathology 48 (2): 116-32. doi:10.1111/j.1365-2559.2005.02248.x. PMID 16405661.
- ↑ Thorsen, AJ. (Feb 2007). "Noninfectious colitides: collagenous colitis, lymphocytic colitis, diversion colitis, and chemically induced colitis.". Clin Colon Rectal Surg 20 (1): 47-57. doi:10.1055/s-2007-970200. PMC 2780148. PMID 20011361. http://www.ncbi.nlm.nih.gov/pmc/articles/PMC2780148/.

