Difference between revisions of "Intranodal palisaded myofibroblastoma"
Jump to navigation
Jump to search
(+images) |
|||
| Line 1: | Line 1: | ||
{{ Infobox diagnosis | |||
| Name = {{PAGENAME}} | |||
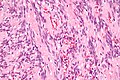
| Image = Intranodal palisaded myofibroblastoma - very high mag.jpg | |||
| Caption = IPM. [[H&E stain]]. | |||
| Micro = Spindle cells with nuclear palisading, RBC extravasation | |||
| Subtypes = | |||
| DDx = [[Schwannoma]] | |||
| Stains = | |||
| IHC = SMA +ve, S-100 -ve | |||
| EM = | |||
| Molecular = | |||
| IF = | |||
| Gross = | |||
| SignsSx = Mass lesion | |||
| Clinical = | |||
| Site = | |||
}} | |||
'''Intranodal palisaded myofibroblastoma''', abbreviated '''IPM''', is a rare tumour that classically presents as an inguinal mass.<ref name=pmid17284119>{{Cite journal | last1 = Nguyen | first1 = T. | last2 = Eltorky | first2 = MA. | title = Intranodal palisaded myofibroblastoma. | journal = Arch Pathol Lab Med | volume = 131 | issue = 2 | pages = 306-10 | month = Feb | year = 2007 | doi = 10.1043/1543-2165(2007)131[306:IPM]2.0.CO;2 | PMID = 17284119 }}</ref> | '''Intranodal palisaded myofibroblastoma''', abbreviated '''IPM''', is a rare tumour that classically presents as an inguinal mass.<ref name=pmid17284119>{{Cite journal | last1 = Nguyen | first1 = T. | last2 = Eltorky | first2 = MA. | title = Intranodal palisaded myofibroblastoma. | journal = Arch Pathol Lab Med | volume = 131 | issue = 2 | pages = 306-10 | month = Feb | year = 2007 | doi = 10.1043/1543-2165(2007)131[306:IPM]2.0.CO;2 | PMID = 17284119 }}</ref> | ||
Revision as of 04:08, 24 May 2013
| Intranodal palisaded myofibroblastoma | |
|---|---|
| Diagnosis in short | |
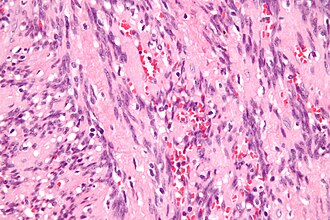 IPM. H&E stain. | |
|
| |
| LM | Spindle cells with nuclear palisading, RBC extravasation |
| IHC | SMA +ve, S-100 -ve |
Intranodal palisaded myofibroblastoma, abbreviated IPM, is a rare tumour that classically presents as an inguinal mass.[1]
General
- Rare ~ 55 cases in the world literature.[2]
Demographics:
- Male:female = 2:1.
- Adults - middle age.
Location:
- Usually inguinal lymph node.
- Reported in retroperitoneum.[2]
Treatment:
- Simple excision; rare recurrences have been reported.[3]
Microscopic
Features:
- Rim of peripheral lymphoid tissue.
- Remnant of lymph node.
- Spindle cells with nuclear palisading - key feature.
- RBC extravasation/hemorrhage.
- Amianthoid fibers - blood vessel surrounded by collagen with (fine) peripheral spokes.[4]
- Paucicellular regions.[5]
- Intracellular and extracellular fuchsinophilic bodies.
- Smooth muscle actin +ve.
DDx:
Notes:
- Fuchsinophilic = affinity for the acid dye fuchsin.[6]
- Image: Fuchsinophilic material (flickr.com) - red.
Images
www:
- IPM (surgicalpathologyatlas.com).
- Amianthoid fibers (nih.gov).[4]
- Amianthoid fibers (nih.gov).[2]
- IPM - several images (upmc.edu).
IHC
- SMA +ve.
- Cyclin D1 +ve.
Other:
- S100 -ve
- Excludes schwannoma.
- GFAP -ve.
- CD34 -ve.
- Desmin -ve
- Ki-67 - low.
See also
References
- ↑ Nguyen, T.; Eltorky, MA. (Feb 2007). "Intranodal palisaded myofibroblastoma.". Arch Pathol Lab Med 131 (2): 306-10. doi:10.1043/1543-2165(2007)131[306:IPM]2.0.CO;2. PMID 17284119.
- ↑ 2.0 2.1 2.2 Sagar, J.; Vargiamidou, A.; Manikkapurath, H. (2011). "Intranodal palisaded myofibroblastoma originating from retroperitoneum: an unusual origin.". BMC Clin Pathol 11: 7. doi:10.1186/1472-6890-11-7. PMC 3146916. PMID 21718465. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3146916/.
- ↑ Creager, AJ.; Garwacki, CP. (May 1999). "Recurrent intranodal palisaded myofibroblastoma with metaplastic bone formation.". Arch Pathol Lab Med 123 (5): 433-6. doi:10.1043/0003-9985(1999)1230433:RIPMWM2.0.CO;2. PMID 10235504.
- ↑ 4.0 4.1 Bigotti, G.; Coli, A.; Mottolese, M.; Di Filippo, F. (Sep 1991). "Selective location of palisaded myofibroblastoma with amianthoid fibres.". J Clin Pathol 44 (9): 761-4. PMID 1918406.
- ↑ URL: http://path.upmc.edu/cases/case121/micro.html. Accessed on: 3 January 2012.
- ↑ URL: http://www.merriam-webster.com/medical/fuchsinophilic. Accessed on: 3 October 2011.